Impaired consciousness and seizures (paediatrics)
Definition and pathogenesis[edit | edit source]
Impairment of consciousness is an imprecise term, it is a general term for the depression of the cerebral cortex. In Anglo-Saxon literature, the name Altered Level of Consciousness – ALOC is used.
Consciousness is the ability to think, to be aware of oneself and one's surroundings. Consciousness requires the function of both cerebral hemispheres and the reticular activating system. It is a disorder of the ascending activation system of the stem and interbrain reticular formation, reticulocortical pathways or a generalized disorder of the cortical functions of both hemispheres. Impairment of consciousness can be divided into qualitative and quantitative .
- Coma is a state in which the child does not regain consciousness even after painful stimuli.
- Lethargy is a state similar to sleep, the child gains consciousness after sound or mechanical stimuli, but immediately falls back into it.
Recent literature recommends not using terms such as sopor, stupor, shallow or deep coma. The most widely used scale for quantitatively evaluating consciousness is the Glasgow coma scale.
The state of consciousness is mediated by neurons of the ascending reticular activating system, which are located in the brainstem and pons. Neural pathways from these areas project throughout the cortex, which is responsible for consciousness. If the function of these neurons is impaired or both hemispheres are affected, ALOC occurs.
The proper function of the ascending reticular activating system and the cerebral hemispheres depends on a number of factors, including the supply of energy to the brain cells, adequate blood flow, the absence of metabolic wastes, i.e. internal and external toxins in plasma, the maintenance of body temperature in the physiological range, the absence of neuronal excitation during convulsive states , absence of CNS infection.
| character | older children | infants | points |
|---|---|---|---|
| opening the eyes | spontaneously | spontaneously | 4 |
| to address | to address | 3 | |
| for pain | for pain | 2 | |
| none | none | 1 | |
| verbal response | oriented | vocalizes | 5 |
| confused | irritating cry | 4 | |
| not snug | crying on algic stimulus | 3 | |
| incomprehensible | moan | 2 | |
| none | none | 1 | |
| motor response | obeys the command | spontaneous momentum | 6 |
| localizes the pain | dodges to a tactile stimulus | 5 | |
| dodges the algic stimulus | dodges the algic stimulus | 4 | |
| decortication reaction | decortication reaction | 3 | |
| decerebrate reaction | decerebrate reaction | 2 | |
| no answer | no answer | 1 |
Evaluation: Glasgow coma score (GCS) is presented as one number from the interval 3-15, which is created by the sum of the individual points. The maximum number is 15 points, the minimum number is 3 points.
Disorders that lead to ALOC due to intracranial hypertension are caused by an increase in the volume of one of these compartments: brain tissue, cerebrospinal fluid, blood. Various herniations can occur due to intracranial hypertension.
Impairment of consciousness can be accompanied by the development of convulsions and vice versa. It follows that even the differential diagnosis of ALOC and convulsions have the same denominators.
Differential diagnosis[edit | edit source]
Differential diagnosis of ALOC and convulsions according to anatomical lesion[edit | edit source]
Clinic of supratentorial lesions leading to coma[edit | edit source]
The supratentorial compartment consists of the cortex, thalamus and other structures above the midbrain. Asymmetric findings on physical examination suggest a cortical lesion. Hemiparesis thus corresponds to a lesion of the contralateral upper motor neuron. Acute unilateral cortical lesions often result in ALOC, but not of a severe degree. However, a significant expansive cortical lesion can lead to severe grade ALOC through the development of intracranial hypertension. A decorticating posture is typical for lesions above the level of the midbrain.
Sudden onset of ALOC in previously healthy children may indicate cerebrovascular events such as bleeding from an arteriovenous malformation, bleeding from the CNS tumor, rarely rupture of the aneurysm. In addition to cerebrovascular events, CNS infections, shock states including sepsis, cerebral trauma (including epidural and subdural bleeding), some tumors, convulsions, neurocutaneous syndromes (phakomatosis) lead to impaired consciousness in supratentorial lesions.
Clinic of subtentorial lesions leading to coma[edit | edit source]
The subtentorial compartment represents the space below the tentorium, includes most of the brain stem, cerebellum and the spaces of the cerebrospinal fluid circulation. Impairment can lead to dysfunction by a mechanism of destruction or compression. Brainstem lesions can be caused by demyelinating or cerebrovascular disease, tumors, trauma. The brainstem is also the site of cranial nerve nuclei. Beacuse the cranial nerves innervate homolateral structures but long pathways innervate contralateral structures, a unilateral brainstem lesion results in ipsilateral cranial nerve dysfunction but contralateral hemiplegia and hemisensory loss (hemiplegia alternans). Anatomically, we can define the site of CNS involvement according to the deficit in the function of the cranial nerves.
Lesions of the midbrain often lead to contralateral hemiplegia, homolaterally we find a pupil that does not respond to light, but in an intermediate position due to palsy ofn. III. Polio III. of the cranial nerve usually causes deviation of the eyeballs laterally or laterally and simultaneously downwards (a sign of the setting sun – Anglo-Saxon literature). A decorticating or decerebrate posture is induced in response to a painful stimulus in patients with midbrain lesions.
Pontus lesions are presented with a decerebrate posture, bilateral miosis, but with a preserved response to illumination, wandering eyeball movements (conjugated horizontal movements are missing, vertical movements and accommodation are preserved), the eyes are often deviated medially. The breathing pattern is varied - we can find central hyperpnea as well as Biot's or apneustic breathing. There is often hemiplegia with contralateral paralysis of the VI and/or VII nerve.
Although hypertonia is a typical symptom of corticospinal tract involvement, it can also be seen in acute midbrain or pontine involvement.
Illness of the medulla oblongata is typical for weakness of the lower limbs, normal pupil size, but no reaction to light, the mobility of the eyeballs is usually preserved, usually nystagmus. Apnea occurs when the respiratory center is affected . We find hemiplegia with weak paresis, problems with swallowing , articulation and coordination.
| the site of the lesion | response to pain | pupil | eye position and movements | respiration | motor skills |
|---|---|---|---|---|---|
| bilateral cortical involvement | evasive maneuver | small, reactive | extraocular movements, ipsilateral deviations in frontal lobe lesions may be induced | posthyperventilation apnea or the Cheyne-Stokes pattern | |
| thalamus | decorticating posture | small and isochoric unless the optic tract is also damaged | eye deviation down and towards the side of the lesion | posthyperventilation apnea or the Cheyne-Stokes pattern | contralateral hemiparesis |
| mesencephalon | decorticate or decerebrate posture | unresponsive to illumination, spontaneously changing size | there may be nystagmus, preserved horizontal movement, absence of vertical movement, loss of adduction ability, both eyes may be deviated laterally and downwards with a lesion of n. III | usually posthyperventilatory apnea or Cheyne-Stokes pattern, possibly central reflex hyperpnea | hemiplegia with contralateral disorder of n. III |
| pons Varoli | decerebrate posture | beat. miosis with preserved reaction to light Horner's syndrome. in a lateral lesion | "floating" bulbs, absence of horizontal movement with preserved vertical movement and accommodation, frequent deviation of the eyes medially, damage to n. VII | central reflex hyperpnea, Biot's pattern, apneustic pattern | hemiplegia with contralateral nerve VI and/or VII disorder |
| medulla oblongata | weak or no DK flexion | normal size, unresponsive, Horner's sy. in a lateral lesion | usually no impairment of spontaneous movement, nystagmus | rarely ataxic respiration, apnea with damage to the respiratory center | weak paresis, difficult swallowing with discoordination, difficult phonation |
| spinal cord | no answer | normal reaction | normal answer | normal | weak paresis, urinary and stool incontinence |
Differential diagnosis of structural and non-structural causes of ALOC and convulsions[edit | edit source]
| structural lesions | toxic, metabolic and infectious causes |
initially focal signs with asymmetric neurological findings, retrocaudal progression
initially often symptomatology from brainstem involvement, sudden onset of severe ALOC, cranial nerve involvement, pathological breathing patterns |
|
Differential diagnosis of ALOC and convulsions according to etiology[edit | edit source]
Overview of ALOC/convulsion causes[edit | edit source]
fever +[edit | edit source]
- febrile convulsions complicated x uncomplicated
- neuroinfection
- meningitis
- encephalitis
- focal infection (brain abscess, subdural empyema, epidural abscess)
- systemic infections with CNS involvement
fever −[edit | edit source]
- tumors
- hydrocephalus
- obstructive (tumor or other causes)
- VP shunt malfunction
- traumas
- commotion
- contusion
- diffuse axonal involvement
- bleeding: intraparenchymal, subarachnoid, subdural, epidural
- brain edema
- intoxication
- sedatives: antihistamines, barbiturates, benzodiazepines, ethanol, narcotics, phenothiazines
- tricyclic antidepressants
- antiepileptic drugs
- salicylates
- epilepsy × postictal state
- body temperature abnormalities: hypothermia × hyperthermia
- hypoxia – ischemia
- circulatory or ventilatory failure
- rival
- heating
- strangulation
- severe anemia
- methemoglobinemia
- carboxyhemoglobinemia
- posthypoxic encephalopathy
- vascular disease
- cerebral infarction (thrombosis, hemorrhage, embolism)
- central venous thrombosis
- subarachnoid hemorrhage
- hypotension × hypertension
- metabolic disorders
- hypoglycemia × diabetic ketoacidosis
- MAC × MAL
- hyponatremia × hypernatremia
- hypocalcemia × hypercalcemia
- hypomagnesemia × hypermagnesemia
- kidney failure
- liver failure
- Reye's syndrome
- hyperammonemia
- hereditary metabolic disorders
- endocrine disorders
- adrenal insufficiency
- thyroid disorders
- hypoparathyroidism
- vitamin deficiency
- pyridoxine deficiency
- thiamine deficiency
- niacin deficiency
- other
- intussusception
- dehydration
- sepsis
- psychiatric illness × affective attacks
- Munchausen syndrome by proxy
Clinical images[edit | edit source]
Convulsions, epilepsy[edit | edit source]
Convulsions lead to a significant impairment of consciousness both during the convulsions and after the seizure. Generalized tonic-clonic convulsions are easily diagnosed, but focal convulsions or absences may have a subtle clinical course: rigid gaze, tremor, blinking, inappropriate discrete and repetitive motor activity. Seizures of all types, except petit mal, can lead to a postictal period with impaired consciousness during which patients slowly regain full consciousness. Posttraumatic or de novo focal seizures must lead to consideration of an intracranial lesion until proven otherwise. In children taking antiepileptic drugs, it is always necessary to check whether the serum level of antiepileptic drugs is within the physiological range. Subtherapeutic levels may induce seizures in decompensated epilepsy with postictal ALOC, while supratherapeutic doses may induce ALOC of intoxication character of different nature depending on the type of medication used. The presence of temperature requires a differential diagnosis to distinguish uncomplicated versus complicated febrile convulsions. In the smallest children, definitely rule out neuroinfection.
Trauma[edit | edit source]
Coma caused by craniotrauma can include subdural and epidural hematomas, subarachnoid and intraparenchymal hemorrhage, penetrating injuries, cerebral contusion and coma, diffuse cerebral edema. Most cases of childhood head injury result from damage to brain tissue during rapid deceleration. This type of disability is most common in the youngest children. The site of bleeding may be located on the opposite side of the blow, due to the rebound movement of the brain within the solid intracranial ("contrecoup" injury). Trauma patients may be unconscious or conscious for varying lengths of time after the insult. All CNS injuries can lead to intracranial hypertension syndrome. Clinically, they present themselves with vomiting, lethargy, varying degrees of impaired consciousness. An increase in ICP leads to a decrease in cerebral perfusion and may result in herniation.
An epidural hematoma is caused by bleeding from cerebral arteries or veins. The hematoma is located in the space between the dura mater and the calva. In 85% it is associated with a skull fracture. An epidural hematoma can occur even after relatively minor trauma. A typical location is the temporal lobe area due to a rupture of the middle meningeal artery. Such an injury leads to a faster development of symptomatology (headaches, vomiting, ALOC) than venous bleeding. The first of the diagnostic symptoms, but already very late, is the dilation of the pupil into mydriasis, typically on the side of the hematoma with contralateral limb deficit = hemiparesis. Approximately 40% of patients may initially be neurologically free of pathology during the so-called lucid interval (lucid interval = immediately after the injury the patient is without symptoms or only with signs of coma, after a certain interval somnolence, impaired consciousness, unconsciousness, coma ) . In young children and infants, the lucid interval is rather an exception. On the CT scan, epidural hematomas are sharply demarcated, unilaterally located, lenticular in shape. Severe progressive anemia, changes in the quality of consciousness, an external head injury, and the finding of a fissure on X-ray of the elbow can alert us to the possibility of epidural bleeding.
Subdural hematomas are caused by injury to the bridging veins between the dura and the arachnoid. They can be bilateral and are 5-10 times more common than epidural hematomas. The symptomatology is similar to epidural bleeding, but the development is often slower. There is therefore more time for a more detailed examination. A lucid interval is more common. Subdurals can appear in a chronic form, often in abused children. In 30% they are associated with a skull fracture, in 75% of patients we find retinal hemorrhages on the background of the eye. On a CT scan, subdural hematomas have a crescent shape.
Subarachnoid hemorrhage as posttraumatic can complicate any type of craniocerebral trauma or is bleeding from a vascular malformation. Clinically, it manifests as meningeal syndrome and severe headaches. As part of the diagnosis, we perform an LP, which is characterized by the finding of erythrocytes, and a CT scan. Many authors mention progressive severe anemia as the leading symptom of intracranial bleeding in the youngest children. It is typical for infancy that clinical symptoms may be completely non-specific or minimal at first. ![]() A normal finding on an X-ray image of the skull does not exclude the intracranial bleeding. It means that in children it is important to perform a blood count examination immediately after the injury and then after a few hours. The finding of progressive anemia is a warning sign.
A normal finding on an X-ray image of the skull does not exclude the intracranial bleeding. It means that in children it is important to perform a blood count examination immediately after the injury and then after a few hours. The finding of progressive anemia is a warning sign.
Diffuse cerebral edema is more common than focal lesions after brain injury and, unfortunately, does not allow for neurosurgical intervention. A characteristic CT finding is the loss of the interface of the gray and white brain matter, but this is only noticeable 12-24 hours after the injury. Radiographic abnormalities may be similar to those resulting from hypoxic injury.
Cerebral coma is an imprecise term for a transient alteration of consciousness during normal neurological function, often involving a transient loss of consciousness after an injury. Post coma syndrome can last for hours to days and is characterized by nausea, vomiting, dizziness, headache. Imaging methods are free of pathology.
Infection[edit | edit source]
The history of fever leads to the consideration of meningitis or encephalitis with different etiology, ALOC can also be part of septic shock. CNS infections leading to coma can affect large parts of brain structures (meningitis, encephalitis) or can be limited to smaller areas (abscess, empyema). Meningitis může být způsobena bakteriální, virovou (enteroviry), mykotickou (Candida, Cryptococcus), Meningitis can be caused by a bacterial, viral (enterovirus), fungal (Candida, Cryptococcus), mycobacterial or parasitic (cysticercosis) etiology. Encephalitides are the result of a viral disease or immunological mechanisms. Varicella encephalitis comes 2-9 days after the seeding of the rash. Brain abscesses are rare in childhood, often in connection with chronic inflammation of the paranasal sinuses or middle ear, dental infection, endocarditis, congenital malformations of the heart. Acute sinusitis can lead to intracerebral or subdural empyema because the infection can spread per continuitatem or hematogenously. Orbitocellulitis can cause thrombosis of the cavernous sinuses.
Intoxication[edit | edit source]
Especially in toddlers and adolescents who have no signs of craniotrauma or lack of evidence of convulsions, we must think about possible intoxication. ALOC associated with intoxication usually has a slower onset than impaired consciousness associated with injury. An important source of information in intoxications is the state of the pupils. Miotic pupils are found in intoxication with narcotics, organophosphates, phenothiazines, barbiturates and ethanol. Mydriatic pupils, on the contrary, in intoxication with anticholinergics (atropine, antihistamines, tricyclic antidepressants), sympathomimetics (amfetamin, caffeine, nicotine, cocaine, LSD), methemoglobinemia, carboxyhemoglobinemia, cyanide poisoning. Nystagmus is found in poisoning with barbiturates, ketamine or phenytoin. In general, the pupillary response is more preserved in coma from intoxication or metabolic causes than in craniotrauma. We do not find anisocoria in cases of intoxication and metabolic causes . On the contrary, anisocoria is an indication for imaging methods of the CNS (statistically CT scan). To diagnose intoxications, we use toxicological screening from blood and urine, possibly gastric contents from lavage. Some intoxications cannot be proven in a toxicology screening, but the state of the pupils can be helpful. In cases of intoxication and metabolic causes, we do not find anisocoria! On the contrary, anisocoria is an indication for imaging methods of the CNS (statistically CT scan).
Tumors[edit | edit source]
ALOC results from convulsions, hemorrhage, increased ICP with decreased cerebral perfusion, or direct invasion of the ascending reticular activating system. The localization of tumors often determines the clinical manifestations. Infratentorial tumors present with ataxia or vomiting, supratentorial tumors with convulsions, hemiparesis, speech disorder, personality disorders. The emergence of acute hydrocephalus in connection with tumors is presented by headaches, lethargy and vomiting.
Vascular causes[edit | edit source]
ALOC of cerebrovascular origin is caused by interruption of blood flow in the CNS. The cause is bleeding, thrombosis or embolism. Bleeding is mostly non-traumatic, conditioned by the presence of vascular abnormalities – arteriovenous malformation, aneurysm or cavernous hemangioma. ![]() Rupture of the AV malformation is the most common cause of spontaneous intracranial hemorrhage in pediatric patients. The bleeding is of arterial origin, localized in the brain parenchyma, but sometimes it also penetrates into the ventricles and subarachnoid space. Aneurysm rupture is less common. In this case, repeated episodes of bleeding may occur, with each subsequent episode increasing morbidity and mortality. Bleeding from venous and cavernous hemangiomas is usually of a smaller scale, so the onset of problems is less acute. Stroke can also occur as part of thrombosis or embolism in undamaged vessels. Cerebral infarctions are caused by occlusion of the anterior, medial, or posterior arteries and result in local neurological impairment, not coma. Cerebral infarction in children may be associated with nephrotic syndrome, sickle cell anemia, homocystinuria, leukemia, vasculitides (SLE, Henoch-Schoenlein purpura, HUS, TTP) nebo thrombophilic conditions (protein C or S deficiency).
Acute carotid artery occlusion due to hemispheric edema with the possibility of herniation can cause coma. Thrombosis of central venous vessels is a consequence of middle ear infection or sinusitis, it can also be related to a hypercoagulable state. Stroke leading to hemorrhage and/or cerebral edema with decreased cerebral perfusion. The result is ALOC, in the most severe cases coma. Less severe impairments usually cause focal neurological defects, where clinical manifestations depend on the localization of CNS damage. Vascular involvement in the cerebellar region leads to ataxia, vertigo, nausea, headaches in the occipital region, and neck stiffness. Occlusion of the basilar artery can affect the upper part of the brainstem. The result is a fast-onset coma. We see the same picture with bleeding or heart attack in the area of the pontine.
Rupture of the AV malformation is the most common cause of spontaneous intracranial hemorrhage in pediatric patients. The bleeding is of arterial origin, localized in the brain parenchyma, but sometimes it also penetrates into the ventricles and subarachnoid space. Aneurysm rupture is less common. In this case, repeated episodes of bleeding may occur, with each subsequent episode increasing morbidity and mortality. Bleeding from venous and cavernous hemangiomas is usually of a smaller scale, so the onset of problems is less acute. Stroke can also occur as part of thrombosis or embolism in undamaged vessels. Cerebral infarctions are caused by occlusion of the anterior, medial, or posterior arteries and result in local neurological impairment, not coma. Cerebral infarction in children may be associated with nephrotic syndrome, sickle cell anemia, homocystinuria, leukemia, vasculitides (SLE, Henoch-Schoenlein purpura, HUS, TTP) nebo thrombophilic conditions (protein C or S deficiency).
Acute carotid artery occlusion due to hemispheric edema with the possibility of herniation can cause coma. Thrombosis of central venous vessels is a consequence of middle ear infection or sinusitis, it can also be related to a hypercoagulable state. Stroke leading to hemorrhage and/or cerebral edema with decreased cerebral perfusion. The result is ALOC, in the most severe cases coma. Less severe impairments usually cause focal neurological defects, where clinical manifestations depend on the localization of CNS damage. Vascular involvement in the cerebellar region leads to ataxia, vertigo, nausea, headaches in the occipital region, and neck stiffness. Occlusion of the basilar artery can affect the upper part of the brainstem. The result is a fast-onset coma. We see the same picture with bleeding or heart attack in the area of the pontine.
Problems associated with VP shunt[edit | edit source]
The most common type of shunt in children with hydrocephalus is the ventriculo-peritoneal shunt, which drains the cerebrospinal fluid from the lateral cerebral ventricle through a small opening in the skull, then through a valve with an attached reservoir located under the scalp. It enters the peritoneal cavity through a catheter placed under the skin of the neck, chest and abdomen. VP shunts can be dysfunctional for a variety of reasons: catheter rupture, valve failure, fluid outflow blockage, catheter disconnection. A serious complication is shunt infection. The risk is highest in the first 6 months after shunt insertion or revision.
Hypoxia[edit | edit source]
Hypoxia severely affects the function of neurons, as neurons are extremely sensitive to oxygen. Permanent damage to CNS cells occurs after 4–5 minutes of total anoxia at normal body temperature. Hypothermia can have a protective effect to some extent. Hypercapnia accompanying hypoxia is also responsible for the degree of neurological damage and the development of coma.
Cardiovascular causes[edit | edit source]
Hypotension of various etiology leads to insufficient cerebral perfusion and thus to alteration of the mental state. Adequate MAP values are necessary to maintain physiological CPP values, which is especially important in conditions with intracranial hypertension. Hypertension with BP values > 99.p. can lead to hypertensive encephalopathy symptomatology including headache, nausea, vomiting, visa disturbances, altered mental status up to coma. A hypertensive crisis in childhood is almost always associated with a secondary cause of hypertension. A complication can be cerebral hemorrhage. Hypertension in association with bradycardia may indicate advanced intracranial hypertension.
Thermoregulation disorders[edit | edit source]
Hypothermia or hyperthermia in childhood is most often associated with an external cause - staying in cold water or overheating in a car standing in the sun. Impairment of consciousness in hypothermia is directly proportional to the drop in core body temperature, as a 1°C drop means a 6% reduction in brain flow. At TT 29–31 °C, confusion, delirium, muscle rigidity come, patients with TT 25–29 °C are comatose, have extinguished deep tendon reflexes and fixed, dilated pupils. Clinical symptomatology of hyperthermia includes headache, vomiting, impaired consciousness, can lead to convulsions or coma. Risky is TT > 41 °C in the rectum = hyperpyrexia.
Metabolic disorders[edit | edit source]
Pathological reduction or, conversely, elevation of a number of ions, disturbances in acid-base balance can be the cause of ALOC. Hypoglycemia as part of metabolic disorders is the most common cause of ALOC, especially in the category of infants and young children. The reason is the limited capacity for hepatic gluconeogenesis. Diabetes mellitus with severe acidosis is also a cause of ALOC due to a combination of hyperosmolality, dehydration, hypotension and MAC (lactate, ketone bodies). Patients in whom as a result of insulin treatment there is too rapid a drop in blood glucose and osmolar shifts are also at risk of ALOC due to brain edema. Impairment of consciousness is also caused by severe ABR disorders, specifically MAC and MAL. The most common cause of MAC is severe dehydration. Even dehydration alone without ion imbalance can lead to ALOC. Dysbalance of sodium, calcium, magnesium, phosphorus occurs in various diseases. The degree of impairment of consciousness depends on how quickly the imbalance occurred and also on the depth of the imbalance. Other causes of ALOC are, more rarely, renal failure with uremia and liver failure. Urea cycle disorders lead to ALOC and hyperammonemia. Reye's syndrome is an extremely rare cause of ALOC today. Organ dysfunction in this syndrome can affect practically all organs, but the liver and brain are most often affected. Disturbances of consciousness due to an as yet unexplained mitochondrial impairment are also rare.
Intracranial hypertension[edit | edit source]
A number of patients with the above-mentioned causes of ALOC fall under this clinical unit. Non-traumatic causes of elevated intracranial pressure include tumors, neuroinfections, malfunction of VP shunts, cerebral hemorrhage, prolonged convulsions. In these patients we find headache, vomiting, confusion, lethargy, meningismus, focal neurological symptoms, convulsions or deep coma. Incipient signs of increased ICP include a bulging fontanelle in infants and a pupillary reaction. A more severe or prolonged increase in ICP leads to anisocoria, cranial nerve lesions (III, IV, VI), papilledema and the so-called Cushing's triad (hypertension, bradycardia, periodic breathing). All these signs signal impending or already progressing herniation. From a clinical point of view, the identification of the type of herniation is not important, as all types are life-threatening and the treatment is identical. hyperventilate and possibly administer mannitol (due to the frequent rebound phenomenon it is no longer recommended[1]). After stabilization of vital functions, we will perform a CT scan with contrast. Regardless of the location of the CNS lesion, a neurosurgeon must be consulted. In patients with VP shunt, shunt control is required.
Other causes[edit | edit source]
Children with intussusception may present with significant apathy or lethargy in combination with vomiting, intermittent abdominal pain, and enterorrhagia. They may often be treated for dehydration, sepsis, or meningitis before a proper diagnosis is made. The presence of "raspberry jelly" during rectal examination and the finding of an abdominal mass during abdominal palpation support the diagnosis of intussusception. Psychiatric illnesses can sometimes mimic ALOC. Only a careful neurological examination will reveal the origin of their disability. Patients with a psychiatric disability, i.e. "conscious", react by ducking when hit in the face, resist opening their eyes, we record an increase in heart rate after acoustic or painful stimuli, have intact deep musculoskeletal reflexes, present oculovestibular and oculocephalic reflexes.
Access to the ALOC patient[edit | edit source]
Patients require a quick evaluation of vital functions and subsequently a search for the cause of the disturbance of consciousness. The simplified procedure can be summarized in the following points:
- provision of vital functions (timely intubation and UPV with provision of normoxemia and normocapnia, provision of access to the vascular bed, possibly, depending on the condition, introduce
- history of head injury, convulsions or intoxication
- signs of increased ICP or focal neurological findings
- TT value
- laboratory results (modification of the internal environment: do not allow hypovolemia , anemia, hyponatremia, hyperglycemia, parenteral nutrition, accurate fluid balance)
- CT scan of the CNS
- CSF analysis
The evaluation of a comatose patient must first rule out immediately life-threatening causes - hypoxia, hypotension, hypoglycemia, intracranial hypertension, convulsions. In the case of these causes, timely resuscitation and provision of vital functions takes precedence over further diagnostic procedures. The patient must be placed on JIRP. In all disorders of consciousness, hypoxia and perfusion disorders are a determining factor in the secondary involvement of the CNS.
In all disorders of consciousness, hypoxia and perfusion disorders are a determining factor in the secondary involvement of the CNS.
History and basic examination[edit | edit source]
If it is possible to take an anamnesis, we ask about the possibility of intoxication with drugs or other toxic substances, we look for a recent injury, we ask about the presence of convulsions, temperature, headaches, irritability, vomiting, gait disturbances, behavioral changes. We are interested in the duration of the disturbance of consciousness, the details of the beginning of the disturbance of consciousness and its course. A physical examination must rule out a head injury: we look for changes on the scalp and skull, an eye examination can show retinal hemorrhages, we can find hemotympanum, otorrhea or rhinorrhea, postauricular hematoma (Battle's sign), periorbital hematoma. Intoxication or a metabolic cause is likely if we find no signs of trauma in an afebrile patient. The presence of fever leads to the consideration of a neuroinfection, as does the finding of purpura or varicelliform efflorescences supports an infectious etiology. Other important physical signs are anisocoria or non-reactive dilated pupils, papilledema, nuchal rigidity. Urinating and/or tarnishing indicates possible spasms.
Assessment of vital signs[edit | edit source]
Assessment and securing of the airway, ventilation and circulation is a priority before addressing the neurological causes of ALOC. We demonstrate hypoxia by measuring SaO 2 , but the values can be false in shock circulation and hemoglobinopathies. Hypoxia is evidenced by cyanosis of the lips and nail beds and SaO 2< 90%. Blood gas analysis is essential for quantitative assessment of respiratory distress and assessment of oxemia. Hypotension is assessed based on BP values according to age, gender and height. However, pale acre, prolonged capillary return, and poorly palpable peripheral pulsations are typical physical findings. Hypertension is a rarer cause of ALOC, the clinic tends to be polymorphic. After correction of BP to "safe" values, if we find a persistent pathological neurological finding, we indicate a CT scan of the head. Pathophysiologically, it is worth noting the fact that hypertension in patients with high ICP leads to an improvement in cerebral perfusion by means of an increase in MAP, and therefore slightly hypertensive BP values are not harmful. We always determine hypothermia and hyperthermia according to rectal temperature values (core temperature). Hypothermia is TT < 35.0 °C, hyperthermia > 41.0 °C.
Neurological examination[edit | edit source]
A neurologic examination of a comatose patient includes standard tests such as eye opening and response to verbal or tactile stimulation, deep musculoskeletal reflexes, and other specialized examinations. Local neurological findings often make it possible to localize the area of CNS involvement. Conversely, focal dysfunctions can lead to misinterpretation and omission of ALOC as a cause (e.g. perceptual aphasia is mistaken for confusion or psychosis).
Eye examination[edit | edit source]
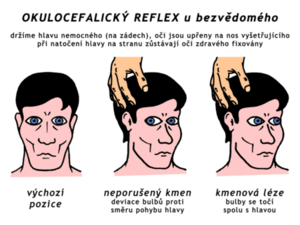
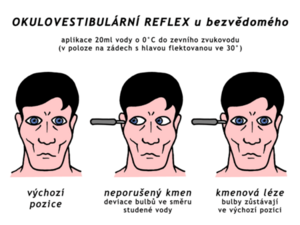
We evaluate pupil size, isokoria and reaction to light. Pupillary response provides a "window into the CNS" in the comatose patient. It is necessary to carefully consider whether the artificially induced mydriasis for the evaluation of the fundus by the ophthalmologist does not overlap with other minima. 24 hours of pupillary reaction, which is sometimes a decisive clinical finding. However, evaluation of the fundus with an ophthalmoscope may reveal fundus congestion (papilledema) or retinal hemorrhage. Edema papillae (bulging on the fundus of the eye) is a sign of intracranial hypertension, although it may be absent at the beginning. Blurred optic disc borders and reduced venous pulsation are typical. Retinal hemorrhages on the background of the eye are a frequent finding in subarachnoid hemorrhage of traumatic or non-traumatic origin. They are often found in CAN syndrome and are associated with head injury. As part of the evaluation of the reaction of the pupils - miosis, we find, in addition to intoxications (e.g. opiates lead to such extreme miosis that the pupils often have the character of a "small pin" and are only visible when examined with an ophthalmoscope), in irritation of the nucleus III (e.g. in case of subarachnoid hemorrhage ). In addition to intoxications, mydriasis can also be found with lesions of the III nuclei, e.g. with massive brain edema (typically bilat. enlarged and unresponsive pupils). Anisocoria is found in uncal herniation caused by unilateral intracranial expansion. A unilaterally enlarged pupil (> 5 mm) and concomitant loss of light reactivity suggests either midbrain or medial temporal lobe displacement or caudal displacement of the upper brainstem. The pupillary reflex remains equipped in intoxications or metabolic disorders (even if modified by miosis or mydriasis present), therefore the equipment or lack of pupillary reflexes is a simple method to distinguish between a structural lesion and a metabolic cause, or intoxication. Conditions that diffusely affect the brain usually do not lead to a distinct pathological reaction of the pupils, except in intoxication. In milder forms of metabolically induced coma, we can observe a wandering conjugate movement of the bulbs from side to side. Persistent deviation of gaze to one side may be associated with a focal CNS lesion or as a postictal state following focal seizure activity. Oculocephalic reflex ("blinking virgin" reflex) = during rapid head rotation, a conjugate movement of the bulbs occurs to the opposite side to the direction of rotation. We do not use this reflex if we suspect an injury to the cervical spine. The ability of this reflex in a comatose patient should indicate normal brainstem function. Conjugate deviation of the eyes tends to be to the same side as the side of the cerebral lesion, but opposite to the site of the brainstem lesion. The depth of ALOC can also be evaluated by the disappearance of spontaneous blinking, in the most severe cases, by the disappearance of the corneal reflex. Conjugate deviation of the eyes tends to be to the same side as the side of the cerebral lesion, but opposite to the site of the brainstem lesion. The depth of ALOC can also be evaluated by the disappearance of spontaneous blinking, in the most severe cases, by the disappearance of the corneal reflex. Conjugate deviation of the eyes tends to be to the same side as the side of the cerebral lesion, but opposite to the site of the brainstem lesion. The depth of ALOC can also be evaluated by the disappearance of spontaneous blinking, in the most severe cases, by the disappearance of the corneal reflex.
Meningeal signs[edit | edit source]
Pathological breathing patterns[edit | edit source]
Pathological breathing patterns are also common in CNS lesions:
- Cheyne-Stokes breathing has an ascending (crescendo) phase, when the frequency and depth of breathing increase, and a descending phase (decrescendo), which ends with an apneic pause (apnea is not a condition, however). It occurs in case of CNS injury, intoxication (depression of the respiratory center), uremia, immaturity, heart failure, increased intracranial pressure.
- Biot's breathing is periodic labored breathing followed by apnea. It is accompanied by CNS involvement in the region of the posterior fossa of the cranium or brainstem, it can be observed when the irritability of the respiratory center decreases during meningitis or encephalitis.
Damage to the brainstem (midbrain, pons Varoli) or dysfunction of both hemispheres may be associated with central hyperventilation, which may lead to significant respiratory alkalosis. An apneustic pattern of breathing, where a 2-3 second pause is observed after each breath, is observed in pontus lesions. However, hyperventilation may only be a physiological response to the presence of fever, MAC (Kussmaul respiration) and hypoxia. Hypoventilation is found in intoxications with barbiturates, alcohol, benzodiazepines and narcotics. Intact respiration while awake, but respiratory failure during sleep (Ondine's curse syndrome) is often associated with a lesion of the spinal cord. Apnea occurs when the spinal cord is damaged up to the C4 area, peripheral nerves or neuromuscular plate.
| respiratory pattern | characteristic | site of disability |
|---|---|---|
| posthyperventilation apnea | posthyperventilation apnea | bilateral hemispheric dysfunction |
| Cheyne-Stokes respiration | breathing has an ascending (crescendo) phase, when the frequency and depth of breathing increases, and a descending phase (decrescendo), which ends with an apneic pause (apnea is not a condition, however) | bilateral hemispheric dysfunction |
| Central reflex hyperpnea | continuous deep breathing | bilateral hemispheric dysfunction
damage to the lower part of the mesencephalon or the upper part of the pontine |
| apneustic respiration | lengthening of the end-inspiratory pause (each breath is followed by a 2-3 second pause = "inspiratory cramp") | Mr |
| Biot's breathing | periodic breathing with respiratory effort followed by apnea | Mr |
| ataxic respiration | sparse irregular breaths | the lower part of the pons, the upper part of the medulla oblongata |
| Ondine's course | failure of involuntary breathing (sleep), preserved free breathing | elongated spinal cord |
| apnea | no respiratory effort | extended spinal cord to C4 level, peripheral nerves, neuromuscular junction |
Movement and Posture Assessment[edit | edit source]
Uncoordinated bilateral limb movements and postural changes can be observed in patients with a milder degree of ALOC. Unilateral twitching of limbs or muscle groups suggests focal convulsive activity or generalized convulsions in a patient with hemiparesis. The decerebrate posture is not constantly permanent. It usually appears intermittently in patients with mesencephalic compression, cerebellar lesions, or metabolic disorders. Decortication posture is found in lesions of a higher level of the CNS, usually in the area of the white matter of the brain, the internal capsule or the thalamus.
- decortication posture includes tonic flexion of the upper limbs and tonic extension, adduction and internal rotation of the lower limbs
- decerebrate posture includes tonic extension of the upper limbs and extension, adduction and internal rotation of the lower limbs
Laboratory and imaging methods[edit | edit source]
Laboratory tests in patients with ALOC should routinely include KO+dif., hemocoagulation, blood group, electrolytes, urea, creatinine, glucose, transaminases, ammonia, lactate, CRP, serum and urine osmolality, Astrup and levels of anticonvulsants in established epileptics. Toxicological and metabolic screening from blood and urine is indicated in patients with ALOC of unclear origin, in the absence of signs of trauma. In these patients, blood glucose should be determined at the bedside. If an infectious cause is suspected, we complete a microbiological examination, blood culture, perform LP (if there are no contraindications). A native CT scan can reveal cerebral edema, hydrocephalus, tumor, hematoma and bleeding. Contrast-enhanced CT requires evidence of cerebral infarction due to thrombosis or embolism. We use MRI and MR angiography for a more detailed evaluation of the structure of the CNS and blood vessels. In newborns and infants with an open fontanelle, an ultrasound examination of the CNS through a window through the large fontanelle can also be beneficial (bed-side examination is also possible). EEG also provides important information.
Coma of unknown origin[edit | edit source]
In patients where the cause of the disturbance of consciousness is not clear, a neurological examination, CT scan without contrast and LP should be performed. Positive meningeal signs without fever or other signs of infection may indicate subarachnoid hemorrhage. The most common errors in the assessment and provision of children with ALOC are:
- excluding the possibility of trauma or intoxication with a negative medical history
- negligence in ensuring vital functions (especially airway patency and ventilation) before performing imaging methods
- hyperventilation of an intubated patient leading to a pCO 2 well below 4.5 kPa
- not providing analgosedation to patients with ALOC
- ruling out possible intoxication if the screening is negative
| tests enabling "supportive therapy" | specific tests |
|---|---|
Astrup
|
Complete examination of cerebrospinal fluid (biochemistry, cytology, culture, PCR, immunology, possible metabolic defects)
|
Links[edit | edit source]
Reference[edit | edit source]
- ↑ ČERNÁ, Olga. Poruchy vědomí u dětí [lecture for subject Předstátnicová stáž z pediatrie, specialization Pediatrie, 1. lékařská fakulta Univerzita Karlova]. Prague. 4. 10. 2019.
Related articles[edit | edit source]
External links[edit | edit source]
- Febrile seizures 2019 — interactive algorithm + test
- Febrile convulsions in children — interactive algorithm + test
Source[edit | edit source]
- HAVRÁNEK, Jiří: Porucha vědomí a křeče.