Craniocerebral trauma
Trauma to the skull and brain can result in death or severe permanent damage to an individual. They occur independently or are part of polytraumas. The most common are traffic, industrial and sports injuries.[1]
Mechanisms of craniocerebral trauma[edit | edit source]
Two basic physical mechanisms apply to head injuries:
- A translational head injury occurs when the head hits an object. There will be a mutual transfer of kinetic energy.
- An acceleration head injury occurs without a direct impact of the head on another body. We distinguish between linear and rotational acceleration injury.[2]
Classification of craniocerebral trauma[edit | edit source]
- Primary craniocerebral trauma
They arise immediately in connection with trauma.
- Fractures of the skull;
- brain injury:
- Secondary craniocerebral trauma
They arise with a time gap from the trauma (as a delayed consequence). They can be influenced therapeutically.
- Intracranial hematomas:
- cerebral edema;
- injury of supply and cerebral arteries;
- intracranial infection;
- liquorice;
- other post-traumatic complications.
Classification according to clinical severity and duration of unconsciousness: light, medium and severe injuries.[2]
Primary craniocerebral trauma[edit | edit source]
Fractures of the skull[edit | edit source]
Closed × open.
Penetrating × non-penetrating.
According to the fracture line:
- linear (cracks, fissures);
- fragmentary (cominutive)with impression or elevation of the edges;
- impressive (impressive).
The brain is most damaged at the site of the skull injury (coup) and at the site of the opposite impact (contre coup).[2]
Diagnosis: X-ray of the skull.
Brain injury[edit | edit source]
Primary × Secondary.
Focal × diffuse.
Concussion[edit | edit source]
A brain concussion (commotio cerebri, concussion) is a sudden, short-term, reversible traumatic disorder of the CNS. It has no lasting effects. The objective neurological findings are without focal changes.
Etiology: dysfunction of the ascending reticular formation.
Clinical picture:
- loss of consciousness for 5 minutes or less [2], max 30 minutes;[1]
- pretraumatic amnesia (retrograde);
- post-traumatic amnesia (anterograde)lasts less than 1 hour.[2]
After awakening from unconsciousness:
- nausea, vomiting, diffuse headache;
- diziness, uncertainty in space during sudden movements, looking up, walking upstairs;
- orthostatic tachycardia and hypotension;
- disorders of concentration, memory, sweating, palpitations, [sleep disorders]].
In 50% of those affected, these symptoms persist as the so-called post-concussion syndrome, sometimes developing several days after discharge from the hospital. This condition can last for several months.[1]
Diagnosis: medical history + normal neurological findings.
Auxiliary examinations: X-ray of the skull and cervical spine.
Treatment: hospitalization in the surgical department, bed rest, observation for 3–5 days – monitoring of the state of consciousness (every 2 hours.), mobility and pupils, symptomatic therapy, incapacity for work for 7–14 days[2] ev. up to 3 weeks.[1]
Prognosis: good, resolve without lasting effects.[2]
Brain contusion[edit | edit source]
Contusion of the brain (contusio cerebri, contusion) is morphological damage to brain tissue often associated with bleeding.
Etiology: translational or acceleration mechanism of injury.
Clinical picture:
- highly variable;
- symptoms often caused by perifocal edema;
- loss of consciousness for minutes to hours;
- several days or weeks of confusion;
- often cardiac dysrhythmias.
Diagnosis: medical history (head injury, unconsciousness, confusion) + focal neurological findings.
Auxiliary examinations: CT (must be repeated 24–48 h apart), X-ray of the skull and cervical spine, examination of the fundus of the eye, EEG within 3 months after the injury to assess focal changes.
Treatment: hospitalization in the surgical department, possibly in ICU, bed rest, anti-edematous treatment (mannitol), nootropics, vitamin C, E, B-complex, etc. rehabilitation.
Prognosis: good, but cognitive and psychosocial disability persists for several months.[2]
Rupture of the brain[edit | edit source]
Rupture of the brain (dilaceratio cerebri) is severe morphological damage to the brain tissue.
Etiology: translational or acceleration mechanism of injury, often associated with contusions and hematomas.
Clinical picture:
- loss of consciousness lasting days, weeks or months;
- further as in contusion, but more pronounced.
Diagnosis: medical history (head injury, unconsciousness) + neurological findings.
Auxiliary examinations: CT (must be repeated 24–48 h apart), x-ray of the skull and cervical spine, examination of the fundus of the eye, EEG within 3 months after the injury to assess focal changes.
Treatment: hospitalization in the surgical department, possibly in ICU, bed rest, antiedematous treatment (mannitol), nootropics, vitamin C, E, B-complex, ev. rehabilitation.
Prognosis: poor, in case of survival there is the persistence of various degrees of physical and psychological deficit.[2]
Diffuse axonal injury[edit | edit source]
Diffuse axonal injury is a traumatic injury to axons. Gray and white matter have different specific weights, and therefore their mutual shear movement occurs during an injury. Axons (white matter) become stretched, damaged and then degenerate.
Etiology: acceleration mechanism of injury.
Clinical picture:
- disturbance of consciousness with focal symptoms;
- there may be decortication rigidity as a reflection of the involvement of motor pathway axons at the level of the internal capsule;
- may be decerebrate rigidity as a result of brainstem involvement.
Diagnosis: medical history (head injury, unconsciousness) + negative CT scan.
Ancillary examinations MRI – small focal changes especially in the area of the corpus callosum, in the subcortical white matter, basal ganglia, thalamus and pons.[1]
Treatment: hospitalization, provision of an internal environment, nootropics (piracetam, approx. 12 g per day).
Prognosis: poor, ad integrum adjustment is not possible, and varying degrees of physical and mental deficit tend to persist.[2]
Secondary craniocerebral trauma[edit | edit source]
Intracranial hematomas[edit | edit source]
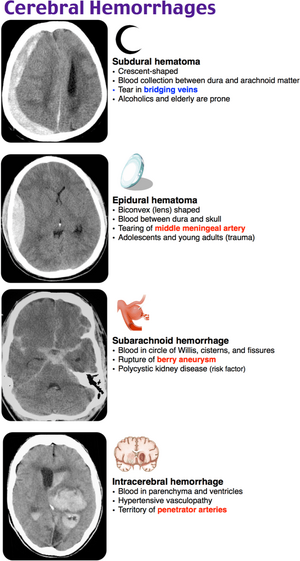
Epidural hematoma[edit | edit source]
An epidural hematoma is a collection of blood between the dura mater and calva. In the supratentorial space, it most often arises on the basis of arterial bleeding, most often bleeding from the middle meningeal artery. In the infratentorial region, venous sinuses tend to be the source of bleeding.[2] Over the age of 60, it occurs rather rarely, because the dura mater adheres tightly to the bone. [1]
Clinical picture:
- small – asymptomatic;
- focal symptoms of a progressive nature;
- impaired consciousness;
- anisocoria – the result of compression of the oculomotor nerve as an initial symptom of temporal herniation (in 85%, mydriasis is on the side of the hematoma);
- hemiparesis (on the opposite side to the hematoma);
- craniocaudal deterioration;
- in a third of patients, there is a so-called lucid interval - after the injury, consciousness is first preserved, and only after that do the symptoms begin to appear.
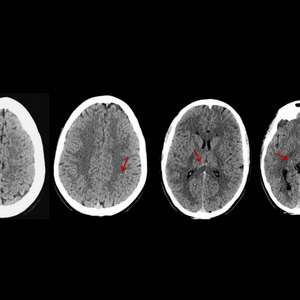
Diagnosis: CT – biconvex hyperdense mass in the calf, often at the site of a skull fracture.
Treatment: neurosurgical removal of the hematoma and ligation of the artery, venous bleeding can be treated conservatively under CT monitoring. [2]
Subdural hematoma[edit | edit source]
A subdural hematoma is a collection of blood between the dura mater and the arachnoid.
- Acute – manifestation within 24–48 h after injury;
- Subacute – manifestation within 3 weeks after the injury;
- Chronic – manifestations over weeks or months. [1]
Clinical picture:
- as in epidural hematoma, but slower progress;
- if a lucid interval is present, it tends to be longer;
- hemiparesis (usually on the opposite side to the hematoma, but can be on the same side if there has been brainstem displacement);
- anisocoria - less often.
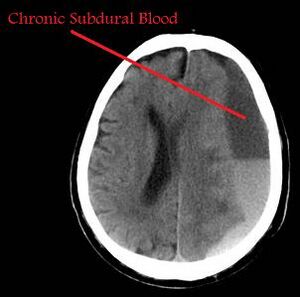
A so-called chronic subdural hematoma is formed when the blood hematoma becomes large. It has its own capsule and inside is a serous fluid. It is most often caused by bleeding of bridging veins (they lead from the surface of the brain to the sinus dura matrix). It is almost always accompanied by cerebral contusion. A chronic hematoma enlarges due to an osmotic mechanism (the capsule is a semipermeable membrane) and due to repeated minor subdural bleeding from proliferating capillaries on the hematoma membrane. It manifests clinically only after a long delay, for example in 3 months or 3 years. [2]
Predisposing factors for the development of chronic subdural bleeding: older age, alcoholism, arachnoid cysts, coagulopathy, anticoagulant therapy, arterial hypertension, epilepsy,… [2]
Clinical Picture
- headache, vomiting, congestion in the background of the eye;
- personality changes and deterioration of intellect;
- quantitative disorders of consciousness with hemiparesis.
Diagnosis: CT.
Treatment: conservative (spontaneous resorption of the hematoma) ev. neurosurgical treatment.
Prognosis: good, with timely treatment without consequences. [2]
The essence of chronic subdural hematoma (from the English CSDH – chronic subdural hematoma) is bleeding from bridging veins in patients with varying degrees of cortical atrophy (elderly patients, alcoholics), and ininfants. CSDH was first described by Rudolf Virchow in 1857 as"pachymeningitis haemorrhagica interna" [3], after which Wilfred Totter described the basics of the pathophysiology of CSDH and thus defined that hemorrhage from bridging veins is its underlying cause and named it "subdural hemorrhagic cyst" [4].
It is important to adequately differentiate CSDH from acute subdural hematoma. Compared to CSDH, acute SDH typically occurs in younger people primarily as a result of more serious craniotraumas and is associated with symptomatic compression of the brain parenchyma, which typically manifests itself within 72 hours. On the contrary, in the case of CSDH, the bleeding is clinically asymptomatic for a longer period of time, on the order of several weeks or months, and most often occurs after minor injuries. The incidence of CSDH in the population is around 1.72/100,000 inhabitants per year, in the population aged 70-79 this value increases to 7.35/100,000 per year, thus further confirming the fact of a higher risk of CSDH in the elderly.
Risk Factors[edit | edit source]
Cerebral atrophy, associated with older age, is among the basic risk factors. In direct proportion to ageing, the space between the calva and the parenchyma itself increases from the original 6% to 11%. This allows the brain to move to the sides, so in the event of trauma, damage to the bridging veins can occur more easily and thus the formation of CSDH [5]. Trauma itself is not the only cause of CSDH, patients with anticoagulant medication, alcoholism or epilepsy are also at risk (up to 10% of patients with CSDH are alcoholics or people with a history of epileptic seizures) [6].
Pathophysiology and symptomatology[edit | edit source]
Damage to the bridging veins (eg in the case of trauma) will result in bleeding into the subdural space, approximately one day after hematoma with a thin layer of fibrin and fibroblast forming around the hematoma itself. Fibrin and fibroblasts continue to proliferate and migrate, creating a kind of membrane (about 4 days after the incident), which then progressively enlarges. Part of the CSDH reabsorbs spontaneously, but the majority grows in volume and results in clinically symptomatic CSDH [7], neurologically manifested by headaches, confusion or, in a more advanced stage, contralateral hemiparesis.
Diagnosis[edit | edit source]
CT is used to visualize the hematoma, it will clearly show the resulting hematoma. It is typically a hypodense extracerebral bed, see figure.
Therapy[edit | edit source]
In the case of non-extensive CSDH without expansive tendencies and the patient's clinically good status, it is not necessary to evacuate the hematoma, conservative treatment consists of thorough monitoring of the patient [8]. In the case of a progressive symptomatic lesion, we indicate a trepanation drill, i.e. the evacuation of colic blood and the introduction of temporary subdural drainage from the site under local anesthesia. In some cases, a craniotomy, is performed, especially in patients with recurrent hematomas, in persons showing reaccumulation of blood after a trenapal puncture, or in the presence of a solid hematoma. It is important to rehydrate the patient and take care of the patency of the drainage under strictly sterile conditions, while after 3 days a control CT is performed and if the findings are satisfactory, the drain is removed. [9][10]
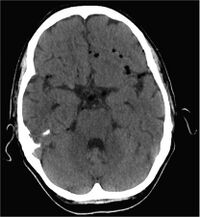
Subarachnoid hemorrhage[edit | edit source]
A subarachnoid hemorrhage is a blood between the arachnoid and the brain tissue itself.
Clinical picture:
- often obscured by dominant injury;
- meningeal syndrome;
- vasospasm (prevention: calcium channel blockers or repeated lumbar puncture).
Prognosis: good.
Complications: vasospasm, communicating hyporesorptive hydrocephalus. [2]
Intracerebral hemorrhage[edit | edit source]
An intracerebral hemorrhage causes focal intraparenchymal blood collections with expansive behavior.
- Acute traumatic hematomas – arise at the moment of injury, and belong to primary brain injuries;
- Delayed bleeding - from 6 hours to several weeks after the trauma
Clinical picture:
- initially a short period of confusion or loss of consciousness;
- further according to localization, size of the hematoma and speed of enlargement.
Diagnosis: CT.
Treatment: conservative (care for the internal environment, antiedematous treatment) or neurosurgical removal.
Prognosis: depends on the location and extent of bleeding, usually, focal neurological deficit remains. [2]
Cerebral edema[edit | edit source]
Generalized × bearing.
Vasogenic × cytotoxic.
Generalized cerebral edema - occurs most often as a result of hypoxia of the brain.
Clinical picture:
- intracranial hypertension syndrome
Diagnosis: CT – reduction of the cerebrospinal fluid space and erasure of the difference between gray and white matter.
Focal cerebral edema – usually occurs around the focus of contusion and intracerebral hematomas.
Clinical picture:
- focal neurological symptoms
Diagnosis: CT – focal hypodense
Treatment: antiedematous (mannitol, Dexona), possibly, craniotomy and external decompression.
Injury to supply and cerebral arteries[edit | edit source]
The cervical and cavernous section of the internal carotid artery arteria carotis interna is most often injured, but these are rare cases. Bleeding into the wall of the vessel creates a dissecting aneurysm, which is manifested by focal symptoms.[2]
Intracranial infection[edit | edit source]
Cerebrospinal Fluid[edit | edit source]
The cerebrospinal fluid is the communication between the subarachnoid and extracranial spaces. It is most often caused by a traumatic mechanism. In the case of a fracture in the area of the front cranial fossa, communication with the nasal cavity and leakage of cerebrospinal fluid through the nose may occur - the so-called rhinorrhea. With fractures of the petrous bone, cerebrospinal fluid can leak from the ear - the so-called otorrhoea. A massive leakage of cerebrospinal fluid causes post-traumatic cerebrospinal fluid hypotension, which manifests itself clinically in almost the same way as the syndrome of intracranial hypertension.[2]
Diagnosis:
- identification CSF(biochemically);
- neuroradiological evidence of communication - isotope cisternography or CT cisternography.
Complications: risk of intracranial infection.
Other post-traumatic complications[edit | edit source]
- Post-traumatic hydrocephalus – most commonly communicating hyporesorptive hydrocephalus;
- post-traumatic epilepsy;
- post-traumatic encephalopathy;
- post-traumatic Parkinson syndrome;
- cranial nerve injury;
- post-traumatic pneumocephalus (air in the cerebrospinal fluid space);
- cerebral turgescence (brain congestion or hyperemia) – increase in cerebral blood volume, e.g. in hypoxia, hypercapnia and lactic acidosis. [1]
Links[edit | edit source]
Related Articles[edit | edit source]
- Assessment of consciousness
- Glasgow Depth of Unconsciousness Scale
- Craniocerebral and spinal cord trauma/PGS
- Acute epidural hematoma/PGS
- Diffuse axonal involvement/PGS
- Concussion/PGS
- Spinal trauma/PGS/diagnosis
External links[edit | edit source]
Craniocerebral trauma- interactive algorithm + test
Reference[edit | edit source]
- ↑ a b c d e f g h AMBLER, Zdeněk. Fundamentals of Neurology. 1. edition. 2006. pp. 171-181. ISBN 80-7262-433-4.
- ↑ a b c d e f g h i j k l m n o p q r s NEVŠÍMALOVÁ, Sona – RŮŽIČKA, Evžen – TICHÝ, Jiří. Neurology. 1. edition. Galén, 2005. pp. 163-170. ISBN 80-7262-160-2.
- ↑ ADHIYAMAN, V.. Chronic subdural haematoma in the elderly. Postgraduate Medical Journal. 2002, vol. 78, no. 916, p. 71-75, ISSN 0032-5473. DOI: 10.1136/pmj.78.916.71.
- ↑ FURLOW, Leonard T.. CHRONIC SUBDURAL HEMATOMA. Archives of Surgery. 1936, vol. 32, no. 4, p. 688, ISSN 0004-0010. DOI: 10.1001/archsurg.1936.01180220114007.
- ↑ ELLIS, G L. Subdural hematoma in the elderly. Emerg Med Clin North Am [online]. 1990, vol. 8, no. 2, p. 281-94, Available from <https://www.ncbi.nlm.nih.gov/pubmed/2187683>. ISSN 0733-8627.
- ↑ JONES, S. A prospective study of chronic subdural haematomas in elderly patients. Age and Ageing. 1999, vol. 28, no. 6, p. 519-521, ISSN 1468-2834. DOI: 10.1093/ageing/28.6.519.
- ↑ MUNRO, DONALD. SURGICAL PATHOLOGY OF SUBDURAL HEMATOMA. Archives of Neurology & Psychiatry. 1936, vol. 35, no. 1, p. 64, ISSN 0096-6754. DOI: 10.1001/archneurpsyc.1936.02260010074005.
- ↑ NAGANUMA, Hirofumi – FUKAMACHI, Akira – KAWAKAMI, Motomasa. Spontaneous Resolution of Chronic Subdural Hematomas. Neurosurgery. 1986, vol. 19, no. 5, p. 794-798, ISSN 0148-396X. DOI: 10.1227/00006123-198611000-00013.
- ↑ SMELY, C. – MADLINGER, A. – SCHEREMET, R.. Chronic subdural haematoma ? a comparison of two different treatment modalities. Acta Neurochirurgica. 1997, vol. 139, no. 9, p. 818-826, ISSN 0001-6268. DOI: 10.1007/bf01411399.
- ↑ BENDER, M. B. – CHRISTOFF, N.. Nonsurgical Treatment of Subdural Hematomas. Archives of Neurology. 1974, vol. 31, no. 2, p. 73-79, ISSN 0003-9942. DOI: 10.1001/archneur.1974.00490380021001.