Epidural hematoma
From WikiLectures
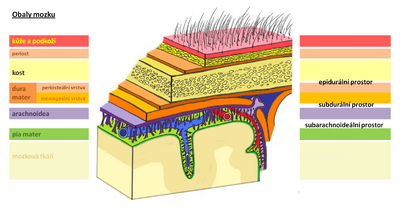
An epidural hematoma is a collection of blood between the dura mater and the calva. In the supratentorial space, it most often arises on the basis of arterial bleeding, most often bleeding from the medial meningeal artery. In the infratentorial region, venous sinuses tend to be the source of bleeding.[1] Over the age of 60, it occurs rather rarely, because the dura mater adheres tightly to the bone.[2]
Clinical picture[edit | edit source]
- Small - asymptomatic;
- focal symptoms of a progressive nature;
- disorders of consciousness;
- anisocoria = the result of compression of the oculomotor nerve as an initial symptom of temporal herniation (in 85%, mydriasis is on the side of the hematoma);
- hemiparesis (on the opposite side to the hematoma);
- craniocaudal deterioration;
- n a third of patients there is a so-called lucid interval –after the injury, consciousness is first preserved, only after that the symptoms begin to appear;
- typical course – fter the injury there is unconsciousness (given by brain coma), then he wakes up to consciousness (the so-called lucid interval) and then there is a rapidly worsening state of consciousness ending in death (this time caused by hematoma oppression);
- only about 15-20% of epidural hematomas have such a course,
- in about a fifth of cases, the injury may not cause unconsciousness (the patient may have the feeling of a hot liquid being spilled in the head),
- or, on the contrary, the injury is more severe and there is no lucid interval at all,
- the entire process can be obscured by the effect of alcohol,
- warning signs –hemiparesis – contralateral (by compression of the cortex), later also ipsilateral (compression of the bilateral pyramidal pathway against the tentorium),
- anisocoria – ipsilateral mydriasis is caused by compression of the III nerve at the junction with the a. cerebri post.,
- for a hematoma in the posterior cranial fossa, a warning symptom is a change in breathing, often while still conscious.
Diagnosis[edit | edit source]
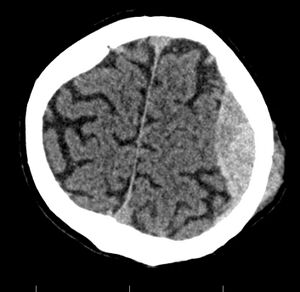
- CT – biconvex hyperdense mass in the calf, often at the site of a skull fracture.
Therapy[edit | edit source]
- Neurosurgical removal of the hematoma and ligation of the artery, venous bleeding can be treated conservatively under CT monitoring[1],
- it is a life-saving procedure, in the case of an acute course it cannot be delayed or delayed by longer transport!,
- must be performed regardless of the patient's condition,
- as a rule, we make a temporal drill and then split the bone or perform a craniotomy,
- sometimes we have to go all the way to the foramen spinosum and plug it,
- due to recurrences, we suture the dura to the periosteum.
Links[edit | edit source]
Související články[edit | edit source]
- Craniocerebral trauma
- Acute subdural hematoma
- Subdural hematoma
- Subarachnoid hemorrhage
- Chronic subdural hematoma
Source[edit | edit source]
- BENEŠ, Jiří. Study materials [online]. ©2010. [feeling. 2009]. < http://jirben.wz.cz >.
Reference[edit | edit source]
External links[edit | edit source]
Literature[edit | edit source]
- NEVŠÍMALOVÁ, Soňa, Evžen RŮŽIČKA and Jiří TICHÝ. Neurology. 1st edition. Prague: Galén, 2005. pp. 163-170. ISBN 80-7262-160-2 .
- AMBLER, Zdenek. Basics of neurology. 6th edition. Prague: Galén, 2006. pp. 171-181. ISBN 80-7262-433-4 .
- ZEMAN, Miroslav, et al. Special surgery. 2nd edition. Prague: Galén, 2004. 575 pp. ISBN 80-7262-260-9 .