Motor system
The motor system controls muscle activity (ensures an upright position, work, food intake, communication). Purposeful movement is coordinated by a greater number of muscle groups at the same time. All sections of the CNS participate in motor control.
The activity of the motor system is:
- 1. Involuntary (stereotypical, fast) and we evoke it with a stimulus
- 2. Free
During movement, a combination of both types occurs.
Corticospinal pathway[edit | edit source]
Corticospinal tract (pyramidal) begins in the primary and secondary motor cortex (gyrus precentralis, superior frontal gyrus and parietal landscape). Pyramidal and extrapyramidal pathways lead from them, the pyramidal pathway itself from Betz cells forms only a smaller part. The Tractus corticospinalis runs from the capsula interna (end brain, cerebral cortex), most of the fibers cross in the decussatio pyramidorum (lower part of the medulla oblongata) and continue in the contralateral lateral cords spinal cord. A brain lesion in the region of the pathway causes paralysis of the muscles on the contralateral side. 75% of the fibers end on interneurons (the interface of the anterior and posterior horns) and 25% of the fibers end on motoneurons (the anterior horns of the spinal cord).
Motor unit[edit | edit source]
The Motor Unit is the basis of the motor system. It is a set of muscle fibers innervated by one motoneuron, and at the same time it is the smallest component that can be independently activated. Axon of a motoneuron branches after entering a muscle, its terminal fiber innervates one muscle fiber at a time. A synapse is formed - neuromuscular plate. Motor units represent the peripheral motoneuron.
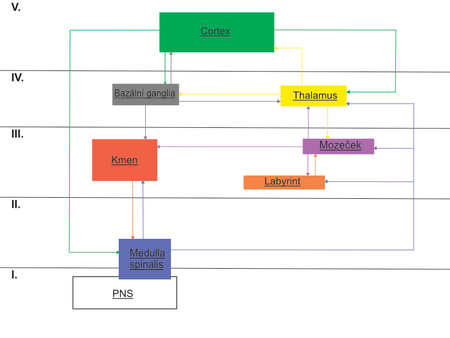
Motion Control Principle[edit | edit source]
Motion control takes place on several levels.
- Spinal cord
- Brain stem
- Cerebellum
- Basal ganglia
- Cerebral cortex
Mutual coordination of agonists, antagonists and synergists is essential. The main role of proprioception is to inform the center about probable movement. The basic impulse to free movement goes through the corticospinal pathway, the control of intensity is in the presence of proprioceptive reflexes. The receptors are muscle spindle (activated during muscle stretch, agonist facilitation and antagonist inhibition) and Golgi tendon bodies (inhibit agonists and facilitate antagonists). The feedback function is that the result of an activity affects the increase or decrease of the given activity
Spinal motor circuit[edit | edit source]
At the level of the spinal cord, in the anterior corners of the spinal cord
- α-motoneurons – large neurons of the anterior horns of the spinal cord, where the corticospinal pathway ends and the motor unit begins
- γ-motoneurons – small neurons of the anterior horns of the spinal cord, innervate muscle spindles
When the spindle is stretched, the excitations facilitate the direct collateral activity of the own α-motoneuron (agonist) and inhibit the antagonist collaterally (via an interneuron). Muscle contraction is caused by a direct stimulus from α-motoneurons, or indirectly reflexively via γ-motoneurons
Principles of motor coordination[edit | edit source]
- Reciprocal innervation – the opposite effect on the motoneurons of antagonistic muscles
- Negative feedback – upon its activation, the interneuron releases the inhibitory transmitter and inhibits its own motoneuron
- The principle of the superiority of higher sections of the CNS - more perfect control of movement
- The principle of the final common pathway - all influences causing muscle contraction are applied by α-motoneurons
Functional unit of the nervous system (reflex)[edit | edit source]
Determined by the reflex arc, consists of 5 parts: receptor, afferent pathway, center, efferent pathway and effector
- Monosynaptic spinal reflexes (proprioceptive, myotactic, stretching) - the impulse is transferred to the α-motoneurons of the same muscle
- Polysynaptic spinal reflexes (exteroceptive) - arises from the activation of a different number of interneurons, when sensitive receptors in the skin are irritated
Muscle tone[edit | edit source]
Degree of resistance during passive movement in the joint
- Reflexively maintained muscle tension
- The cause is the low-frequency excitatory activity of α-motoneurons
- It results from the bombardment of AP(action potentials) coming from higher levels of the CNS and afferent fibers of somatosensory receptors
Lesions[edit | edit source]
In the case of central and peripheral motoneuron lesions, a movement disorder appears (slight muscle strength, clumsiness, loss of active movement - partial or complete)
- Light lesion - frustrating
- Partial movement disorder - paresis
- Monoparesis – one limb is affected
- Hemiparesis – one half of the body is affected
- Paraparesis – the lower limbs are affected
- Triparesis – impairment of three limbs
- Quadriparesis – impairment of all limbs
- Complete movement disorder - plegia (disappearing lesion syndrome)
Symptomatology[edit | edit source]
Momentum[edit | edit source]
- Central lesion – several muscle groups are damaged
- on the upper limbs, extension of the fingers, elbow and abduction in the shoulder are more affected
- flexion in the hip, knee and dorsiflexion of the leg is affected on the lower limbs
- Peripheral lesion – corresponds to a disorder of respective innervation areas
Myotatic reflexes[edit | edit source]
- Central lesion - increased reflexes due to spasticity
- Peripheral lesions – reduced or extinguished reflexes
Muscle tone[edit | edit source]
- Central lesion (spastic) - hypertonia, in the acute phase - pseudoweak paresis
- Peripheral lesion (weak) – hypotonia, atonia
Rigidity – basal ganglia lesions, agonist and antagonist hypertonia, α-motoneuron hyperactivity
Trophics[edit | edit source]
Interruption of the influence of motoneurons of the anterior horns of the spinal cord - muscle atrophy
- Central lesion – trophic level is normal
- Peripheral lesion – damage to any part of the motor unit results in muscle atrophy
Pathological polysynaptic reflexes (spastic phenomena)[edit | edit source]
Manifestation of central lesions positive spastic pyramidal phenomenon (Babinsky reflex – inversion of the cutaneous plantar reflex)
Fasciculation[edit | edit source]
Manifestation of peripheral disorders of spontaneous contraction of groups of muscle fibers
Fibrillation[edit | edit source]
Manifestation of peripheral involvement - spontaneous contractions of one muscle fiber (not visible, only on EMG)
Links[edit | edit source]
Related Articles[edit | edit source]
References[edit | edit source]
- AMBLER, Zdeněk. Fundamentals of Neurology. 6. edition. Galen, 2006. pp. 66-67. ISBN 80-7262-433-4.