Thermoregulation
Maintaining an optimal body temperature despite the environmental conditions is a necessary function of the organism of warm-blooded animals, including humans. A relatively constant body temperature is necessary for the normal functioning of metabolism and the course of enzymatic reactions. Body temperature is determined by the result between intake, production and output of heat. The balance between these events is ensured by thermoregulation.
Thermoregulation of the human body is based on the principle of negative feedback or homeostasis. The regulatory center is the hypothalamus, where signals from thermoreceptors are evaluated . Based on this, the production and release of heat by the organism is controlled. The core of the human body is warm-blooded (homoiothermal) – even in the case of large fluctuations in the ambient temperature, its temperature changes only minimally. Peripheral parts of the body (skin, limbs), on the other hand, are cold-blooded (poikilothermic) and partially adapt their temperature to the environment, which prevents high heat losses.
The average body temperature at rest is 36,6–37 °C[1],in the mouth, 0,6 °C[1] higher in the rectum. Most organs require a temperature of around 37 °C, but we normally range up to 35,5–40 °C, this is due to various physiological influences such as circadian rhythms (during the day it fluctuates from 36 do 37,5 °C[1], minimum in the morning, maximum in the afternoon), the menstrual cycle (during ovulation a drop of 0,3 °C, in the second half of the cycle due to progesterone and also during pregnancy up to + 0,5 °C [2]), physical load, food intake, age (greater effect of ambient temperature on children), surrounding environment (thermal comfort is a state where, thanks to an adequate ambient temperature, the organism does not need to engage thermoregulatory mechanisms (20–21 °C dressed, 28–30 °C naked) and mental state (up to + 2–3 °C). During exertion, the temperature in the rectum can rise up to 40 °C[2].
Heat production in the body[edit | edit source]
Heat is created in the body primarily as a side effect of metabolic processes and a consequence of muscle work. At rest, more than half (56 %[3]) of heat is produced in the internal organs. The following contribute to the generation of heat:
- the average basal metabolism of all cells The amount of heat released in such a way can be measured either calorimetrically or indirectly, i.e. by measuring the consumption of oxygen involved in the release of 95% of the energy from the ingested food. If we know the energy equivalent of oxygen for individual nutrients, i.e. how much energy is released by the consumption of 1 liter of oxygen, we can calculate the total energy released for a given time period;
- thermogenic effect of food;
- increased metabolism activated as a result of the action of regulatory hormones, e.g. sympathetic, adrenaline, noradrenaline, thyroxine, etc. (This factor manifests itself especially in the long term.);
- increased metabolism due to muscle strain, chills, digestion;
- increased metabolism due to increased cell temperature due to an increase in the rate of ongoing chemical reactions;
- thermogenesis in brown fat (chemical non-shivering thermogenesis).
Approximately 18 %[3] of heat is generated at rest in muscles. The rest of the heat is produced by the brain and other tissues. During exertion, the proportion of muscle work can rise up to 90 %[3]. If the temperature of the human body drops below 35,5 °C[2], muscle tremors begin.
Heat output[edit | edit source]
The thermal insulation properties of individual tissues are essential for controlling body heat loss:
Heat insulation[edit | edit source]
The vascular system transfers heat very well and it is conducted from the core to the periphery mainly through this route. By regulating blood flow through the subcutaneous venous plexuses, it is possible to significantly influence heat loss. In contrast, skin, subcutaneous fat and fat are insulators – they have one-third the ability to conduct heat and protect the body from losses. Large losses of heat in the periphery are also prevented by a countercurrent mechanism, where the warm arterial blood flowing from the core to the periphery transfers the heat to the cooler venous blood returning back.
Regular clothing will reduce heat loss by half, special clothing by up to one-sixth. Wet clothing, on the other hand, allows up to 20x higher heat loss.[1]
Heat loss occurs through mechanisms that are divided into direct and indirect.
"Direct heat loss"
- radiation;
- conduction;
- convection (flow).
"Indirect heat loss"
- evaporation from the lungs;
- evaporation (sweating), imperceptible/perceptible.
Direct heat loss[edit | edit source]
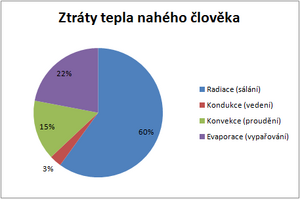
- radiation – in our climatic conditions , an important heat loss factor accounting for up to 60% of total heat loss (if we ignore extreme climatic conditions such as high air temperature, high humidity, high air velocity, etc.). An organism, like any other material object with a temperature higher than absolute zero, emits thermal electromagnetic radiation into the environment. Infrared radiation with a wavelength of 5–20 µm is important for the human body. The amount of energy emitted is according to the Stefan-Boltzman law directly proportional to the fourth power of the body's absolute temperature. However, the surrounding bodies act on the human organism through exactly the same mechanism. The total radiated energy is thus given by the difference of the fourth powers of the surface temperature of the human body and the temperature of the bodies in its immediate vicinity. The so-called thermal comfort of a person in living spaces is directly related to radiation, which is affected by both the temperature of the air in the room and the temperature of the surface of the walls. (The sum of these two temperatures is approx. 37 °C)
- conduction – the transfer of heat in a material environment from a place with a higher temperature to a place with a lower temperature by transferring the kinetic energy of the oscillatory movement of the elements of this environment. Conduction is therefore not a process associated with mass transfer, but only with thermal energy. The amount of energy Q thus transferred during the time τ (s) between two places depends on the difference in their temperatures Δt (K), the distance d (m), the area S (m²) over which the heat transfer takes place, and the thermal conductivity coefficient λ ( J/msK) expressing the ability of the substance to conduct heat, according to the following relationship: Q = λ.S.Δt.τ/d. In the human body, blood is a good conductor, and fat tissue is a thermal insulator. Under standard conditions, i.e. in a closed room at normal temperature without clothing, a person loses approximately 15% of thermal energy. Heat is conducted into the air and bodies, which are in direct contact with the surface of the human body (skin). Under normal conditions, i.e. if it does not flow around the body, air is a very good thermal insulator. However, a diametrically different situation occurs if the surrounding environment is water or very dense and fast-flowing air. Then the decisive heat losses will be given by conduction.
- convection, flow – a process closely related to conduction. First, the heat must be transferred to the substance by conduction, which is then removed to the surroundings by convection. In contrast to radiation and conduction, in addition to energy transfer, matter is also transferred during convection. The amount of heat Q that is removed during a given time τ (s) from the surface of a body with an area S (m²) to the environment with a temperature lower by Δt (K) is given by the relation: Q = α.S.Δt.τ, where α ( W/K.m²) is the interface heat transfer coefficient.
The coefficient of heat transfer through the interface α (W/K.m²) cannot be included among the so-called material constants, which unambiguously characterize a given substance or environment, because the value depends on many theoretically vaguely formulated and practically difficult to measure factors. The coefficient α cannot therefore be calculated, but it can be determined experimentally using so-called alphameters.
The effects of conduction and convection are particularly noticeable under extreme climatic conditions. An example can be, for example, the different tolerance of the organism under different conditions: The human organism tolerates frost much better when there is no wind at low relative air humidity than a temperature slightly above the freezing point with intense air flow and high humidity.
Indirect heat losses[edit | edit source]
Evaporation of water
Due to the large specific heat of evaporation of water, evaporation under normal conditions accounts for up to 25% of heat loss from the body. Evaporation of water occurs during respiration and evaporation. During respiration, the exhaled air is almost completely saturated with water vapor, the partial pressure of which reaches up to 6.3 kPa at normal atmospheric pressure. We distinguish between perceptible and imperceptible evaporation (inspiratio insensibilis). No noticeable evaporation is the process of spontaneous diffusion of water through the skin without the participation of sweat glands, which is almost unregulated by the human body. Quantitatively, it is mainly determined by the nature of the external environment (temperature, relative humidity, speed of air flow, etc.) Under normal conditions, the human body loses approximately 660 ml of water per day through imperceptible evaporation. Perceptible sweating, i.e. evaporation with the participation of sweat glands, is energetically more significant. Water loss can be up to 1.5 liters per hour under extreme conditions. Perceptible evaporation is regulated by the organism, but its efficiency is again noticeably influenced by the properties of the surrounding environment.
Perceptible sweating is the basic mechanism of body removal in the human organism under conditions when the high temperature of the environment does not allow the application of other mechanisms of heat loss (in a sauna, where the air is dry, a person can stay at a much higher temperature than in a steam bath, where the air is 100% humid).
The sweat glands are innervated cholinergically from the sympathetic nervous system (the only exception being that acetylcholine is a sympathetic postganglionic neurotransmitter). Sweat is first formed as primary sweat (filtered protein-free plasma). Reabsorption occurs in the duct depending on the rate of secretion:
- slow – Na and Cl reabsorption → water reabsorption → ↑urea, lactate, potassium;
- fast – little reabsorption → ↓urea, lactate, potassium.
An ordinary person is able to sweat 1 liter per hour, after acclimatization to a warm environment, perspiration rises to 3 liters per hour. At the same time, due to the higher production of aldosterone, excessive losses of Na and Cl are prevented.[1]
Thermoregulation[edit | edit source]
The center of temperature regulation is the hypothalamus. Central thermoreceptors are located in the anterior hypothalamus (ncl. preopticus, ncl. hypothalami anterior[1]). Two-thirds of them react to heat, a third to cold.[4] The posterior hypothalamus ocontains a center that evaluates signals from the anterior hypothalamus (inhibition) and from peripheral thermoreceptors , which are located mainly in the skin and spinal cord. There are ten times more cold receptors than heat receptors in the periphery.
Lowering the temperature[edit | edit source]
In the case of increased body temperature, the anterior hypothalamus, is activated , which leads to the inhibition of sympathetic centers in the posterior hypothalamus.
Basic regulatory mechanisms for lowering body temperature (increasing heat flow to the environment):
- vasodilatation – while normally 5% of cardiac output flows into the skin, this proportion can be increased up to 30% by maximum dilation. This will increase heat transfer to the skin up to eight times;[1];
- noticeable sweating – from 37 °C;
- limitation of heat production.
When the ambient temperature rises above 30 °C a paradoxical rise in temperature occurs due to increased delivery mechanisms (increased metabolism)!
Increase in temperature[edit | edit source]
The reaction to cold is the opposite. The posterior hypothalamus is stimulated by cold receptors from the periphery.
Basic regulatory mechanisms for increasing body temperature (reducing heat flow to the environment):
- vasoconstriction (from 36,8 °C);[2];
- increase in heat production;
- thermogenesis – cold shivering (muscle work uncontrollable by consciousness), chemical thermogenesis, regulation of thyroxine;
- increase in metabolism (action of calorigenic hormones);
- "goosebumps" (reaction of the autonomic nervous system, a residue from animals which, by bristling the fur, increase its insulating properties);
- piloerection – little significance in humans;
- hunger.
Muscle tremors[edit | edit source]
The primary tremor motor center located in the dorsomedial part of the posterior hypothalamus is inhibited from the anterior hypothalamus at normal temperature. In case of activation by peripheral thermoreceptors (temperature drop below 35,5 °C[2]) stimulation of the anterior spinal motoneurons occurs, which will increase resting muscle tone. Thanks to the feedback mechanism through the muscle spindle, muscle tremors are likely to occur. Heat production in the muscles can thus increase up to five times.[1]
Chemical (non-shaking) thermogenesis[edit | edit source]
Noradrenaline from sympathetic nerve endings or an increased level of adrenaline in the peripheral blood activates the protein thermogenin (uncoupling protein 1, UCP1) β3-adrenergic receptors.[5] This will enable the respiratory chain to be disconnected ofrom ATP production on the inner mitochondrial membrane. The gradient of protons is thus used to produce heat.
This mechanism takes place in brown adipose tissue, it is of fundamental importance for humans in newborns, when it allows heat production to be increased up to twofold. Brown fat is located in the area under the shoulder blade and around the large vessels, even in an adult, but the importance of this mechanism is considerably lower in adults and allows for an increase in heat production by 10-15%..[1]
Regulation of metabolism by thyroxine[edit | edit source]
As a result of long-term (several weeks) exposure to low temperatures, the production of the hormone thyroxine increases in animals. However, the significance of this mechanism in humans is still questionable. [1]
Extreme temperatures[edit | edit source]
The regulatory mechanisms of the human body make it possible to maintain a constant core temperature at ambient temperatures of 12–54 °C[4]. In the case of higher temperature fluctuations and extreme temperatures, free regulation is essential - i.e. clothing, finding shelter, active movement.
High temperatures[edit | edit source]
VExcessive sweating occurs when exposed to high temperatures. Adaptation mechanisms to high temperatures are, for example, the overproduction of aldosterone, which during sweating prevents high losses of ions or an increase in blood volume. Elderly people often have a lower than normal body temperature due to lower physical activity and cardiovascular capacity. At a high ambient temperature, there is a danger of peripheral vasodilation, impaired cardiac output, dehydration, which can lead to thermal collapse.
Sunstroke[edit | edit source]
Heat stroke occurs when the body temperature is raised above 40,5 °C[6]. Such a high temperature is no longer tolerated by the brain, therefore increased sweating, especially in the face, cools the venous blood, which subsequently lowers the blood temperature in the internal carotid artery in the cavernous sinus.[6] f the increase in temperature lasts for a long time, the thermoregulatory centers fail, confusion and loss of consciousness appear, hypovolemic shock may develop due to high fluid losses.[1] If the body temperature is not reduced (e.g. by immersion in cold water), brain edema occurs and the patient dies.[6]
Sunburn[edit | edit source]
Burns are mainly caused by direct sunlight falling on the head and neck area, when there is a rapid rise in temperature in the thermoregulatory centers. It leads to malaise, impaired concentration, headache, dizziness, nausea, vomiting, stiff neck, congestion of the cerebral membranes (up to serous meningitis, brain edema), and can be fatal.[6]
Low temperatures[edit | edit source]
Resistance to low temperatures is higher. When cooled by a few degrees, a spontaneous increase in temperature occurs after returning to a normal environment, and the organism is usually not damaged. If the core temperature drops below 28 °C, spontaneous return is impossible , but when warmed up, it returns to normal. A person can tolerate a temperature drop of up to 21 °C, without consequences, which is used in surgery.[2] However, twenty to thirty minutes in ice water, when the human body cools down to 24 °C, will cause cardiac arrest and death without help.[1]
Newborns are more prone to hypothermia due to their relatively large body surface area, small amount of subcutaneous fat, and immature shivering thermogenesis.
Fever[edit | edit source]
Fever is caused by setting the regulation (set-point) to a higher temperature than normal. It causes a feeling of coldness, chills, and hair standing on end. After some time, the set temperature drops, which leads to overheating and profuse sweating (flush).
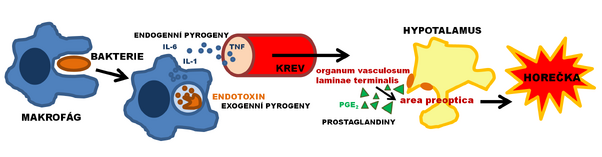
A fever is a response to an inflammatory reaction in the body. Cells of the immune system activated by infection (monocytes, macrophages and Kupffer cells) trigger the production of cytokines (IL-1, IL-6, β-IFN, µ-IFN, TNF-α), which are referred to as pyrogeny. Via the organum vasculosum laminae terminalis (circumventricular organ of the third cerebral ventricle), the area preoptica of the hypothalamus is activated and prostaglandins are produced, which set the regulatory set-point to a higher value and thereby cause fever. Acetylsalicylic acid (aspirin) and other nonsteroidal antirheumatic drugs, like paracetamol, reduce the production of prostaglandins by inhibiting cyclooxygenase.
The importance of fever lies in the inhibition of the activity of microbes, among other things by reducing the plasma concentrations of iron or copper, and in limiting the replication of cells affected by viruses.[6]
Links[edit | edit source]
[edit | edit source]
- Malignant hyperthermia
- Effects of extreme temperatures on living organisms
- Thermotherapy
- Effects of high temperatures on the organism
- Body heat loss
- Hyperthermia
- Fever
External links[edit | edit source]
Reference[edit | edit source]
- ↑ a b c d e f g h i j k l GUYTON, Arthur C – HALL, John E. Textbook of Medical Physiology. 11. edition. Elsevier, 2006. 11; pp. 782–784. ISBN 978-0-7216-0240-0.
- ↑ a b c d e f GANONG, William F. Review of Medical Physiology. 20. edition. Prague : Galén, 2005. 890 pp. pp. 495. ISBN 80-7262-311-7.
- ↑ a b c SILBERNAGL, Stefan – DESPOPOULOS, Agamemnon. Atlas of Human Physiology. 6. edition. Prague : Grada, 2004. 448 pp. pp. 238. ISBN 80-247-0630-X.
- ↑ a b FRANĚK, Miloslav: Thermoregulation. Lecture for the 2nd year of the 3rd LF UK (Physiology), 10. 1. 2011.
- ↑ -,. Wikipedia: Otevřená encyklopedie: Thermogenin [online]. [cit. 2011-04-16]. <https://en.wikipedia.org/w/index.php?title=Thermogenin&oldid=403720650>.
- ↑ a b c d e SILBERNAGL, Stefan – LANG, Florian. Atlas of human pathophysiology. 1st czech edition. Prague : Grada, 2001. 390 pp. ISBN 80-7169-968-3.
References[edit | edit source]
- GUYTON, Arthur C – HALL, John E. Textbook of Medical Physiology. 11. edition. Elsevier, 2006. 11; pp. 782–784. ISBN 978-0-7216-0240-0.
- FRANĚK, Miloslav. Thermoregulation [lecture for subject physiology, specialization general medicine, 3rd LF UK]. Prague. 10.1. 2011. Avaliable from <https://docplayer.cz/26965954-Termoregulace-doc-mudr-miloslav-franek-ph-d.html>.