Disorders of the intercellular substance
- Disorders of the amorphous component – mucus dystrophy (accumulation or loss of mesenchymal mucus).
- Disorders of the fibrous component
- Hyaline dystrophy – strengthening of bonds between collagen building units – hyaline is a structureless eosinophilic mass of various composition and origin, macroscopically vitreous in appearance, it is stained the same as collagen (pink in HE, blue in blue trichrome).
- Fibrinoid dystrophy – loss of the fibrous arrangement of collagen and change in coloration (materials stain similarly to fibrin – intensely red in HE, red in blue trichrome and yellow in Weigert).
Normal image of the intercellular mass[edit | edit source]
Detection of proteins can be performed both histochemically and serologically (labeled antibodies against the given protein):
- Fibrous component
- collagen (type I – collagen ligament, type II – cartilage, type III – reticular fibers, type IV – basement membranes) – stains pink in HE eosin, yellow, blue and green in trichromes, red in Weigert van Gieson;
- elastin – staining for elastic (orcein, aldehyde-fuchsin, resorcin-fuchsin);
- reticular fibers (collagen III) – silvering (argyrophilic), PAS+.
- Amorphous component
- proteoglycans (proteins + glycosaminoglycans) – neutral mucus (mesenchymal origin);
- glycoproteins.
Mucosubstances (mucus) are demonstrated non-specifically by mucicarmine.
- Acidic mucus (mucin - of epithelial origin) - alcian blue;
- Neutral mucus (mucoid – mesenchymal origin) – PAS+.
Mucous dystrophy[edit | edit source]
Mucous dystrophy is a disorder of the amorphous component of the intercellular mass that involves the accumulation or loss of mucus.
Accumulation of mucus of epithelial origin (acidic mucopolysaccharides - mucin)[edit | edit source]
- Mucus hypersecretion during inflammation
If the inflammation affects the mucous membrane, hypersecretion of mucus occurs, which then mixes with the exudate – the so-called catarrhal inflammation .
- Alopecia mucinosa
Accumulation of mucosubstances between the epithelia lining the hair follicles.
- Cystic fibrosis (cystic fibrosis)
Congenital metabolic disorder, AR hereditary disease. It is caused by a mutation in the CFTR gene on chromosome 7 , which is expressed in the epithelial cells lining the gland ducts. Its product is a transmembrane protein that serves as a Cl - and H 2 O transporter across the membrane. The result of the defect is a great thickening of the secretion. It affects the lungs, pancreas, liver, intestine, gonads.
For more detailed information, see the Cystic Fibrosis page .
- Increased mucus production in some tumors
E.g. mucinous carcinoma ( carcinoma adenomatosum muciparum ) or gelatinous carcinoma from signet ring cells.
Accumulation of mucus of mesenchymal origin (neutral mucopolysaccharides – mucoid)[edit | edit source]
- Ganglion
It arises when tissue is repeatedly traumatized (e.g. in the subcutaneous tissue in the area of tendon attachments) as a tissue-encapsulated cavity filled with mucus. A similar process in the artery wall is referred to as cystic adventitial degeneration .
- Myxedema
Accumulation of mucous substances in the joint during hypothyroidism (can be acquired - hypothyroidism , or congenital - cretinism ). Mucopolysaccharides bind water and edema occurs - pretibial, hands, feet, eyelids, tongue and submucosal tissue of the larynx (thickening of the voice).
- Erdheim's cystic medionecrosis
It affects the media of the aorta, in which the muscle and elastic disappear, sinuses filled with mucus are formed. These predispose to aortic dissection .
- Mucopolysaccharidoses
Accumulation of mucus in various tissues due to enzyme defect. They can be acquired or congenital.
They can be divided into mucopolysaccharidoses:
- with mucopolysacchariduria (enzymopathy affecting lysosomes) - mucus often accumulates in the corium (thickening of the skin - gargoyles - gargoyles) or in the bones (growth disorders);
- without mucopolysacchariduria (incorrect distribution of enzymes - absent in lysosomes, found extracellularly).
Loss of mucus of mesenchymal origin[edit | edit source]
- Sclerosis
A relative increase in collagen (due to a decrease in GAG), e.g. in senile atrophied skin. In atherosclerosis , the ratio in the representation of mucosubstances also changes (increase in dermatan and heparan sulfate, decrease in the amount of chondroitin sulfate).
- Fibrosis
Absolute increase in collagen (the amount of GAG remains normal).
Hyaline dystrophy[edit | edit source]
In hyaline dystrophy, there is a strengthening of the bonds between the structural components of collagen, which in EM have the appearance of thin, disordered fibrils, with more amorphous protein matter between them.
Under the light microscope, the hyaline appears as an eosinophilic mass. It stains like collagen – pink in HE , blue in blue trichrome. It resembles amyloid , macroscopically its deposits resemble cartilage .
In hyaline dystrophy, it is extracellular hyaline, in contrast to hyaline ossification , where amorphous eosinophilic masses are localized intracellularly.
Hyaline-degenerated tissue (so-called hyalinized tissue - stiff, hardened tissue) has a tendency to steatosis and calcification (typically in atherosclerosis ). Hyaline is often found in scars and chronic inflammation. In the case of primarily proliferative inflammation of the serous membranes - polyserositis (Curschmann's disease) cartilaginous hard whitish deposits form, e.g. in the capsule of the spleen - coating spleen ( perisplenitis cartilaginea ) or on the surface of free bodies in the peritoneal cavity ( corpus liberum ).
Fibrinoid dystrophy[edit | edit source]
Fibrinoid dystrophy is a loss of the fibrous arrangement of collagen and a change in colorability:
- Matters staining like fibrin – in HE brick red, in Weigert yellow, in blue trichrome red.
- In fact, it is really fibrin. The name fibrinoid was coined earlier when the true composition of this "fibrin-like substance" was unknown.
Macroscopically, there are no changes. It arises on an autoimmune basis as fibrinoid necrosis :
- Interstitial fibrinoid – the focus of necrosis is penetrated by inflammatory exudate in interstitial fibrinous inflammation. Examples:
- rheumatic fever - affecting mainly the heart - pancarditis - when microscopic deposits are formed in the endocardium and myocardium ( granulomas - Aschoff's nodules - fibrinoid necrosis in the center, which is surrounded by a border of Aschoff's cells);
- polyarteritis nodosa ;
- collagenosis – systemic lupus erythematosus , scleroderma , dermatomyositis .
- Vascular fibrinoid must be distinguished from interstitial fibrinoid :
- It occurs in the wall of the arteries (especially the arterioles of the kidneys, spleen and pancreas) during hypertension , when plasma penetrates the vessel wall (plasmorhagia) and its protein components (fibrinogen, immunoglobulins) stain as fibrin.
Hyaline petrification[edit | edit source]
Intracellular occurrence of hyaline in the form of deposits or droplets, examples:
- Mallory hyalin – cytokeratin coiled into a ball in the cytoplasm of hepatocytes in alcoholic cirrhosis
- Councilman's bodies - apoptotic bodies in hepatocytes in hepatitis , tend to be inside the ER (as well as inclusions of α 1 -antitrypsin deficiency ).
- Crooke's cells - non-neoplastic cells in the vicinity of a pituitary adenoma producing ACTH (and thus causing Cushing's disease ). They contain spirally coiled cytokeratins in the cytoplasm.
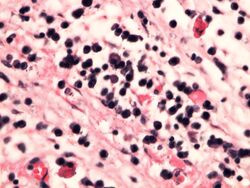
- Russell bodies – inclusions in the cytoplasm of plasma cells during chronic inflammation (correspond to Ig accumulated in GER). The cell takes on a silky appearance, when it ruptures, the hyaline gets into the extracellular space.
- Trachoma bodies – in the cytoplasm of the conjunctival epithelium during Chlamydia trachomatis infection , they contain glycogen.
- Viral inclusions - they are formed either by own viral inclusions or by proteins of cells damaged by the virus, they can be:
- intranuclear – e.g. in keratinocytes in herpes infections;
- intracytoplasmic – e.g. in ganglion cells in rabies (so-called Negri bodies ).
- Dystrophic changes of ganglion cells – in degenerative brain diseases, e.g. Lewy bodies (spherical eosinophilic inclusions in the cytoplasm of ganglion cells, there is a clearing around them, they are larger than the nucleus).
Links[edit | edit source]
Source[edit | edit source]
- PASTOR, Jan. Langenbeck's medical web page [online]. ©2006. [feeling. 2011-10-22]. < https://langenbeck.webs.com/ [1]>.