Dissection of the thoracic aorta
From WikiLectures
Dissection of the thoracic aorta is a sudden vascular event with a dramatic course, immediately threatening life.
Pathogenesis[edit | edit source]
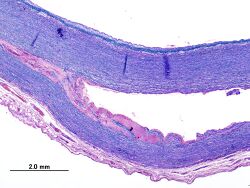
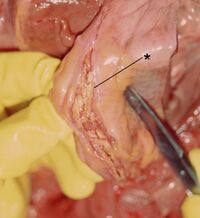
- Splitting of the aortic wall caused by the penetration of blood through a tear in the intima and media.
- The tear most often occurs above the separation of the coronary arteries or in the area of the aortic isthmus.
- From the site of the tear, the dissection can spread peripherally or centrally, it can affect the entire circumference or only a part. The channel can also spread to the carotids or the visceral branches of the aorta.
- At the end of the dissection, another crack (reentry) can occur and a communicating channel is formed
Consequences
- The channel compresses the right lumen of the aorta with gaps.
- The dissection created above the coronary arteries often spreads centrally and tears off the commissures of the aortic valve, causing significant insufficiency.
Causes
- Degenerative changes of the media (cystic medianecrosis) or aneurysm in combination with hypertension, less often atherosclerosis.
- It is often seen in Marfan's disease (young patients) and in other systemic diseases of the connective tissue (Ehlers-Danlos syndrome, Loyes-Dietz syndrome).
- Other predisposing factors include bicuspid aortic valve, coarctation of the aorta or trauma (falls, car accidents),
Classification[edit | edit source]
Classification according to DeBakey[edit | edit source]
- Type I – begins in the ascending aorta and continues to the abdomen,
- Type II – limited to the region of the ascending aorta,
- Type III – begins in the aortic isthmus and affects the descending aorta, or continues to the abdomen.
Stanford classification[edit | edit source]
- Type A – the ascending aorta is affected (2x more often than type B),
- Type B – the descending aorta is affected.
Clinical picture[edit | edit source]
- Sudden shocking pain behind the sternum and in the back , may progress to the abdomen.
- Sometimes a shock state follows (bleeding, tamponade, acute cardiac insufficiency) - they usually die suddenly.
- Sometimes the symptoms gradually subside and the condition stabilizes temporarily or permanently.
- Vascular symptoms:
- different, depending on which branches of the aorta are compressed or torn off,
- cranial arteries – unconsciousness, hemiparesis,
- subclavian – HF ischemia,
- upper mesentery – intestinal ischemia,
- renal arteries – anuria, oliguria,
- peripheral arteries – deficit or asymmetry of pulsations (typically variable in time), lateral asymmetry of pressures on the HCC, etc.
Diagnosis[edit | edit source]
- Typical history (suddenly occurring sharp pain),
- physical examination: deficit or asymmetry of pulsations on peripheral arteries,
- auxiliary methods:
- exclusion of AMI (ECG),
- X- ray of the chest - expansion of the shadow of the upper mediastinum to the left,
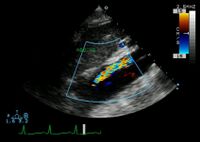
- ECHO, CTA, aortography.
- The sovereign method - transesophageal echocardiography - determines the diagnosis in 98%.
Indications for surgery[edit | edit source]
- According to the type, extent, vascular involvement and overall condition:
- with type A, about half of those affected die within 24 hours, the hope decreases with every hour → type A is always indicated for an immediate surgical solution,
- for type B, we mainly choose a conservative procedure, if there is no vascular symptomatology or there is no threat of rupture.
Therapy[edit | edit source]
- Immediately after establishing the diagnosis, we will start medical treatment: antihypertensives, beta blockers and vasodilators, diuresis support . We monitor the patient, administer analgesics (insufficient pain treatment leads to failure of antihypertensive drugs). In patients with hypotension, it is necessary to rule out cardiac tamponade by echocardiography.
Type A[edit | edit source]
The principle of the operation – we try to cancel the inflow into the aneurysm, several methods:
- transverse incision of the ascending aorta at the site of the tear, suturing of both ends of the aorta through the external and internal meatal pads, subsequent suture of the aorta,
- resection of the ascending aorta, strengthening of the ends with a suture and replacement of the aorta with a prosthesis,
- Bentall's operation – replacement of the aortic valve and ascending aorta with a conduit with a valve, implantation of coronary arteries into a prosthesis,
- closing the entrance to the dissection with tissue glue with an aortic suture or with a substitute,
- implantation of an intraluminal annular prosthesis into the ascending aorta.
Type B[edit | edit source]
- Uncomplicated type B dissection is treated conservatively (stabilization, antihypertensives).
- For complicated dissections, it is necessary to proceed to invasive treatment:
- endovascular stent graft implantation,
- surgical solution.
The principle of surgical treatment
- In the right lateral position, from a left thoracotomy, usually without ECC, some bypass is sometimes used to protect the kidneys and spinal cord from ischemia .
- Resection of the section with a tear, replacement with a prosthesis, or implantation of an intraluminal prosthesis – we cancel the entry and it is closed by thrombosis. The operation is more complicated when the visceral arteries diverge from the dissection channel – a laparotomy must be performed and those arteries reconnected to the aorta.
Complications[edit | edit source]
Stanford A dissection can cause acute aortic insufficiency, heart failure, hypotension. Coronary artery occlusion by dissection leads to AMI (diaphragmatic infarction is most often caused by ACD occlusion ). Rupture of the dissection into the pericardium will result in cardiac tamponade.
Stanford B dissection can be complicated by spinal, visceral, renal or limb ischemia.
Links[edit | edit source]
Related articles[edit | edit source]
External links[edit | edit source]
- Aortic Dissection - video on youtube.com DOESN'T work
References[edit | edit source]
- ZEMAN, Miroslav, et al. Special surgery. 2. edition. prague : Galén, 2006. ISBN 80-7262-260-9.
- ČEŠKA, Richard, ŠTULC, Tomáš, Vladimír TESAŘ a Milan LUKÁŠ, et al. Interna. 3. edition. Prague : Stanislav Juhaňák - Triton, 2020. 964 pp. ISBN 978-80-7553-780-5.
Source[edit | edit source]
- BENEŠ, Jiří. Studying material [online]. [cit. 17.5.2010]. <http://jirben.wz.cz>.