Pathological calcification
Calcification[edit | edit source]
Deposition of calcium (in the form of calcium salts - phosphates or carbonates) in tissues that are not normally calcified (calcified).
Proof of calcification
- In histology, it appears when staining with haematoxylin (the affinity of calcified tissue to haematoxylin is not due to calcium salts, but to organic components of mineralised tissue, probably phosphoproteins/phospholipids[1]; they stain blue - basophilic);
- Koss reaction - reaction with AgNO3 based on reduction of Ag+ to Ag0 - phosphate salts stain black, calcium itself needs to be proven by another method (e.g. Alizarin red).
Classification of pathological calcification
- Dystrophic - into tissues previously pathologically altered in normal calcemia.
- Metastatic - deposition of calcium into certain tissues (lung interstitium, gastric mucosa, kidney, internal elasticity of arteries)[1] in the presence of increased calcemia (parathyroid adenoma with PTH hypersecretion, tumor bone destruction, hypervitaminosis D), as blood pH is physiologically elevated in these tissues and Ca2+ salt solubility is reduced.
Dystrophic calcification[edit | edit source]
Deposition of calcium salts in pathologically altered tissues during normocalcaemia (2.25-2.75 mmol/l[1]), the calcified tissue may subsequently ossify (metaplastic ossification). Calcification begins with the formation of small intracellular vesicles bound to mitochondrial remnants (via phospholipids):
- Necrotic tissue - mostly in caseous necrosis in TB (almost never calcifies infarction), in typhus necrosis of mesenteric nodes, fetal calcification in ectopic pregnancy - lithopedion, calcification of necrotic and desquamated epithelia of the kidneys in sublimate poisoning (mercury nephrosis).
- Hyaline altered connective tissue - anular sclerosis of heart valves, senile cataract (lens calcification), cartilage calcification in old age.
- Inflammatory new-formed connective tissue - calcification in the cores of pericardial leaves after pericarditis (pericarditis petrosa), in the wall of chronically inflamed gallbladder (porcelain gallbladder).
- In blood vessels - calcification of thrombus (phlebolith - mixed Ca and Fe deposits - siderocalcinosis), atherosclerotic plaques, media of muscular arteries (Mönckeberg's medial calcinosis - unlike classical atherosclerosis, sclerosing and then calcifying process does not take place primarily in the intima, but in the media).
- Calcospherites - spherical or mulberry-like calcified formations. If they resemble grains of sand, we speak of psamomatous bodies. These are probably calcified microtubules, present in the dura mater and choroid plexus, in the pineal gland (in older people they appear as a sac filled with fine sand - acervulus), in various tumors (meningioma, papillary cystadenomas of the ovary).
- Calcification of tumors (leiomyoma, thyroid).
Metastatic calcification[edit | edit source]
Deposition of calcium salts in certain, pathologically unchanged tissues in hypercalcemia. The cause of hypercalcemia can be parathyroid adenoma, bone decalcification by tumor, hypervitaminosis D (for example, in TB and sarcoidosis - epithelioid cells form an enzyme that converts vitamin D into its active form), excessive drinking of milk in gastric ulcer, etc. Affects:
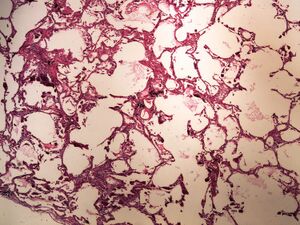
- Lung - calcification of the vessel wall in the interalveolar septa - the appearance of the lung is normal, but palpation gives the impression of pumice (pumice lung).
- Stomach - deposition of calcium salts in capillaries in the middle zone of the mucosa.
- Kidneys - presence of calcium cylinders in tubules, calcification of interstitium, but also intracellularly, in the lining of tubules (disruption of the process of resorption and transport of Ca2+ by tubular cells in hypercalcemia). In parallel, calcium phosphate nephrolithiasis develops - the resulting nephrocalcinosis can lead to renal failure.
Calcinosis cutis (calcification of skin)[edit | edit source]
In the subcutaneous tissue, mushy masses of calcium phosphate appear, and the masses may ulcerate and roll outwards (calcium fistula). Calcinosis of the skin takes the form of circumscribed (affecting mainly the bellies of the fingers and the skin over the extensors) or generalized (generalized appearance of calcified nodules or widespread calcification of the skin - the affected person becomes completely immobile, the disease is always fatal).
Calciphylaxis[edit | edit source]
Tissue rapidly calcifies if it has been previously infiltrated by a "pickling agent" (especially iron compounds).
Calcium gout (pseudogout, arthritis calcinosa, chondrocalcinosis)[edit | edit source]
- Deposition of calcium phosphate in and around joints. It resembles gout (in which, however, urate crystals are deposited).
- Manifestation in middle age.
- Hereditary type - manifestations in the first years of life.
- Secondary type - associated with hyperparathyroidism, haemochromatosis and hypothyroidism.
Links[edit | edit source]
Related articles[edit | edit source]
Source[edit | edit source]
- PASTOR, Jan. Langenbeck's medical web page [online]. ©2005. [cit. 2011-10-26]. <http://langenbeck.webs.com>.
References[edit | edit source]
- ↑ a b POVÝŠIL, Ctibor a Ivo ŠTEINER, et al. Obecná patologie. 1. vydání. Praha : Galén, 2011. 290 s. s. 58. ISBN 978-80-7262-773-
Used literature[edit | edit source]
- MIŘEJOVSKÝ, Pavel a Blahoslav BEDNÁŘ. Obecná patologie. 1. vydání. Praha : Karolinum, 1994. 84 s. ISBN 80-7066-950-0.
- MAČÁK, Jiří. Obecná patologie. 1. vydání. Olomouc : Univerzita Palackého, Lékařská fakulta, 2002. 189 s. ISBN 80-244-0436-2.
- POVÝŠIL, Ctibor a Ivo ŠTEINER, et al. Obecná patologie. 1. vydání. Praha : Galén, 2011. 290 s. s. 58. ISBN 978-80-7262-773-8.