Tuberculosis (pathology)
Tuberculosis is a specific (granulomatous) inflammation, the causative agent of which is Mycobacterium tuberculosis (Koch's bacillus - acid-resistant rod, confirmed by staining according to Ziehl-Neelsen) – type humanus or bovinus.
Gateways of infection[edit | edit source]
The entry gate of the infection into the body can be the respiratory tract, through which droplets containing bacteria from a sick person or animal with open tuberculosis are inhaled. Furthermore, the GIT, through which the infection is transmitted by ingesting contaminated food or e.g. milk from infected cows. Direct contact, kwhen it is mainly about professional infections, e.g. with pathologists or veterinarians. And also transplacentally.
Morphological manifestations[edit | edit source]
Tuberculosis is characterized by a tendency to sulphuretization (caseification, caseous Necrosis) and subsequent colicization (after the penetration of polynuclear cells, which release their proteolytic enzymes) or calcification.
Tuberculosis nodule (tuberculosis)[edit | edit source]
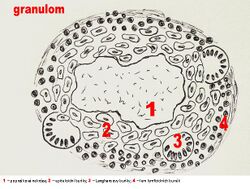
A spherical deposit with a diameter of 1-2 mm (resembles a mole (lat. milium - miliary nodule), can be gray and hard (hard tubercle) or yellow and soft (with central caseification - soft tubercle). Microscopically, it consists of:
- Epithelioid cells – larger elements with abundant, pale cytoplasm and irregular, often elongated nuclei with little chromatin. They are arranged in an irregular mosaic (their borders are difficult to see), they are arranged radially at the edges of the central caseification.
- Langhans cells – large, round, multinucleated elements. They are formed by the fusion of multiple histiocytes. Their nuclei are smaller and darker than the nuclei of epithelioid cells and are arranged at the periphery of the cell in a circle or horseshoe shape (mostly open towards the center of necrosis).
- Reticulin fibers – a number of fibers passing through the nodule between the epithelioid cells.v
- Central caseification – caseous necrosis. Type of coagulation necrosis. Characterized by a slower course due to the inhibition of proteases by mycobacteria. Nuclei are preserved longer, which is manifested by a basophilic dusting of their fragments in an otherwise eosinophilic mass.
- A rim of lymphoid cells – mainly lymphocytes and plasma cells (mostly with abundant Russel bodies). The demarcation is not sharp, and lymphocytes can thus also be found in the nodule between the epithelioid cells.
It disappears completely after effective treatment. It heals with a scar (reticulin fibers thicken, take on the character of hyaline beams, epithelioid cells shrink and approach fibrocytes). It undergoes caseification with subsequent colic and emptying – the formation of an acute cavern. Caseification subsequently calcifies
Tuberculous exudate[edit | edit source]
Similar to serofibrinous exudate of non-specific inflammations. It contains a small number of cells, mainly macrophages (they contain phagocytosed bacteria, have a circular vacuolated cytoplasm harboring lipids - they are also referred to as Orth cells), lymphocytes and a small amount of polynuclear cells.
The exudate undergoes caseification in places or in its entirety, which also affects the surrounding tissue structures. Specific granulation tissue often develops on the periphery of caseous masses (in the form of typical nodules or a continuous border of epithelioid cells). This can organize and encapsulate the caseified deposit. Bacteria and especially their products can penetrate through the capsule into its surroundings, where caseification takes place. Another rim of specific granulation tissue is formed. Later encapsulation takes place and the whole process is repeated. The deposits ( tuberculomas ) formed in this way resemble tree rings in cross-section. In a favorable case, the content of the deposit thickens and calcification occurs.
During colic, liquefied substances (so-called tuberculous pus) can spill into the adjacent cavity (bronchus, pleural cavity, etc.), creating an acute cavity (liquefaction does not concern the entire necrosis, there are remnants of cheesy substances on the walls of the cavity). An acute cavern can be encapsulated by an organizational process that turns into a ligament – the inner wall is smoothed out and a chronic cavern. is formed . However, mycobacteria are maintained on its surface, often in the form of macroscopically visible colonies of the so-called Koch lens. If the connection between the chronic cavern and the bronchus is preserved, bacteria enter the sputum and are coughed out (so-called open tuberculosis).
Distribution of tuberculosis[edit | edit source]
Primary tuberculosis (childhood type)[edit | edit source]
Characteristic for the organism's first encounter with an infection (most often in childhood, rarely in adults). It consists in the emergence and development of the primary complex (i.e. a deposit at the point of entry of bacteria – primary infection + a deposit in a regional lymph node – lymphadenitis + lymphangiitis).
When the infection enters by inhalation, mycobacteria multiply in the lungs for non-specific alveolitis (serofibrinous inflammation). during the development of cellular immunity. Then a primary infection (Ghon's infection) occurs - it is most often in the lower lobes of the lungs. Alveolar macrophages that have engulfed the mycobacteria return to the alveolar septa and lymphatics reach the hilar nodes, where lymphadenitis occurs.
With oral infection the primary infection can be in the lymphadenoid tissue of the terminal part of the ileum, cecum or appendix (relevant nodes - mesenteric) or in the tonsilla pharyngea (relevant nodes - submandibular, deep neck). In DÚ, the primary complex is called Bruusgaard's.
Further fate of the primary infection:
Healing (in 90 %) – fibrous encapsulation, hyalinization, deposition of anthracotic pigment, thickening and dystrophic calcification (infection may still persist and be a source of reinfection in adulthood). Progression – further development (mainly in people with reduced resistance).
Spreading directly from the primary complex – per continuitatem or breaking through of cheesy masses from the primary infection or node into the bronchi and further porogenic spread.
- Lymphogenic propagation - it spreads to other nodes, which enlarge and form packets (so-called scrofulosis), and more than once their liquefied contents break through fistulas.
- Hematogenous propagation - either follows lymphogenic spread (via ductus thoracicus), or by penetrating into a vein - thus either generalization (miliary or large nodular) or the formation of isolated metastases occurs.
Miliary generalization: lungs, liver, spleen.
Large nodular form: spleen.
Isolated metastases: leptomeninges (basilarmeningitis), lung apex (Simon's focus), adrenal glands, bones, kidneys, genitals.
Secondary tuberculosis (adult type)[edit | edit source]
It occurs in persons (usually adults) who have already experienced a primary infection. It is characterized by an already formed (and healed – scarred, calcified) primary complex and organ tuberculosis (i.e. involvement of individual organs – lungs, kidneys, bones and joints, brain membranes – most often only a single organ is affected).
t spreads mainly porogenically. Therefore, hematogenous spread and generalization do not occur, but it can nevertheless lead to very serious and even fatal damage to organs (breathing disorders, urinary excretion, bleeding with rupture of large vessels - e.g. so-called Rassmussen's aneurysm). Secondary (AA) amyloidosis infertility, basilar meningitis can occur when the branches of the lung are affected by the tubercular process, compression of the vertebrae with deformation of the spine and chest, and with consequences for the respiratory system and heart .
The cause is either repeated exogenous infection or reactivation of infection from the primary complex or other foci arising from it. Its course differs from the course of childhood tuberculosis in that the healed primary complex has left a certain resistance (resistance, but not immunity), which, however, can be reduced in old age (formation of senile tuberculosis), physical and mental hardships, malnutrition, poor hygiene, infectious and metabolic (diabetes mellitus) diseases. It easily affects asthenics.
In the affected organ, tuberculous foci develop (e.g. in the lung, typically apically, in contrast to a primary infection that affects the lower lung lobes), caseous foci (can become encapsulated and calcified) or, after colicization and sequestration, cavernous foci - liquefied masses can spill over and porogenically spread (in the case of the lungs to the bronchi, upper respiratory tract or intestine).
Overview of extrapulmonary spread of tuberculosis[edit | edit source]
- Per continuitatem – from the lungs to the pericardial and pleural cavity.
- Porogenically – from the lungs to the larynx (catch on the vocal cords), to the small intestine (swallowing sputum), from the kidney to the urinary tract, ascending to the second kidney, prostate, epididymis.
- Lymphogenically – to other nodes (e.g. neck).
- Hematogenously – to the kidneys, spleen, liver, meninges, skin, bones and joints, genitals, etc.
Links[edit | edit source]
Related Articles[edit | edit source]
External links[edit | edit source]
- Tuberculosis (youtube.com video)
Source[edit | edit source]
- PASTOR, Jan. Langenbeck's medical web page [online]. [cit. 17. 8. 2009]. <https://langenbeck.webs.com/>.