Phagocytosis
Phagocytosis is the ability of cells to absorb foreign particles, microbes or damaged cells.[1] Phagocytoses are capable of cells involved in non-specific immunity of organism - antigen presenting cells, monocytes, from which individual species macrophages (Kupffer cells, histiocytes, microglia and others), and white blood cells (neutrophilic leukocytes, eosinophilic leukocytes). These cells are capable of diapedesis and transition to damaged tissue, where they form shells and absorb unwanted particles and cells.
General basis[edit | edit source]
Cells[edit | edit source]
Cells primarily intended for phagocytosis are referred to as professional phagocytes. These include neutrophils, eosinophils, monocytes → macrophages. They form the basis of cellular non-specific immunity and play a central role in inflammatory response.
- However, neutrophils do not express MHC II. classes, so they cannot present antigen to specific immunity components and therefore do not belong to APC - antigen presenting cells. However, they are important in the defense against extracellular bacteria.
- Macrophages specialize in "cleaning up" the remains of their own cells that have died apoptosis. Thus, they are mainly used in defense against intracellular bacteria.
The rate difference in intervention is that granulocytes act immediately and macrophages only after signal activation, for example: (cytokines, T-lymphocytes, interferon- gamma; TNF). Neutrophils live short (6–12 hours), macrophages long at various stages - in the circulation or in tissues. The fraction of circulating neutrophils corresponds to the fraction of neutrophils adhered to the vascular wall. Of the total number of neutrophils, only about 7% are peripheral and the rest can be found in the bone marrow, where they can be gradually washed out as needed by the body. The ratio of circulating and medullary neutrophils is altered by inflammatory cytokines and bacterial products.
Mechanism of passage into damaged tissue[edit | edit source]
The phagocyte is trapped on the surface of endothelial cells of inflamed tissues thanks to adhesive molecules that are expressed under the influence of inflammatory cytokines → penetrates the tissue (diapedesis = extravasation) → active movement to the site of damage. Movement is controlled by chemotactic, substances released at the site of inflammation.
- 1st phase: extravasation / diapedesis involves interactions between endothelial adhesive proteins (selectins) and carbohydrate structures on the surface of neutrophils = rolling; reversible adhesive interactions; slows down the movement of neutrophils.
- 2nd phase: binding of neutrophil surface adhesion molecules (leukocyte Integrins) to endothelial cell surface glycoprotein (ICAM-1, CD54); monocytes and eosinophils adhere to endothelium (VCAM-1) via β1-integrins.
- 3rd phase: after firm capture, phagocytes stretch between endothelial cells, leaving the vessel → into the tissue.
Chemotactic factors[edit | edit source]
Phagocytes target the site of inflammation according to a chemotactic gradient.
- main chemotactic substances for neutrophils: cytokine (chemokine), interleukin-8 (IL-8),
- for monocytes, eosinophils: MIP-1α, MIP-1β, MCP-1, RANTES,
- common: C3a, C5a, leukotriene B4 (LTB 4), PAF, fMLP (formylmethionylleucinphenylalanine; bacterial protein peptide).
For all these substances, there are relevant receptors on the surface of phagocytes; stimulation of the receptors causes chemotaxis and subsequent activation of phagocytosis. Phagocytes in the tissue actively move towards the site of inflammation (they secrete hydrolytic enzymes → they break down the components of the intercellular mass). This shift occurs through reversible adhesive interactions - the contractile fiber system (actin, tubulin). The neutrophils that completed the task soon die and the remains are removed by other phagocytic cells (macrophages). Dead neutrophils form a pus. Macrophages repeat phagocytosis several times.
Phagocyte recognition mechanisms[edit | edit source]
Phagocytes recognize structures on the surface of the microorganism, but not on the damaged cells themselves. These recognition structures include, for example: lipopolysaccharides, teichoic acids (in all G + and G- bacteria), mannans (in yeast). Non-immunological phagocytosis
- Interactions between surface lectins (proteins carbohydrates) phagocytes and carbohydrates (in microbial glycoprotein and polysaccharide e).
- Mannose receptor recognizes D-mannose.
- The galactose receptor recognizes galactosyl residues on the surface of senescent erythrocytes. Bacterial lipopolysaccharides bind CD14 and others.
- Scavenger receptors recognize polyanionic structures (teichoic acid, negatively charged phospholipids on apoptotic cells).
Opsonization
- Interaction of antibodies, complement, serum proteins.
 For more information see Opsonization.
For more information see Opsonization.
Fc receptors
- Antibodies bound to the microorganism recognized.
- Activation of complement on the surface of microorganisms
- Deposition of fragments of complement proteins (especially C3). Complement is recognized. receptors. Antibodies and complement fragments act as opsonins - they refer to the particle as foreign. Mannose-binding lectin (MBL), fibronectin, fibrinogen, CRP, amyloid P,… also act as such.
Immunological phagocytosis
- Induced by Fc-receptors and complement receptors.
Acute phase proteins
- Produced liver due to inflammatory cytokines: MBL, fibronectin, fibrinogen, CRP, serum amyloid P.
 For more information see Acute phase proteins.
For more information see Acute phase proteins.
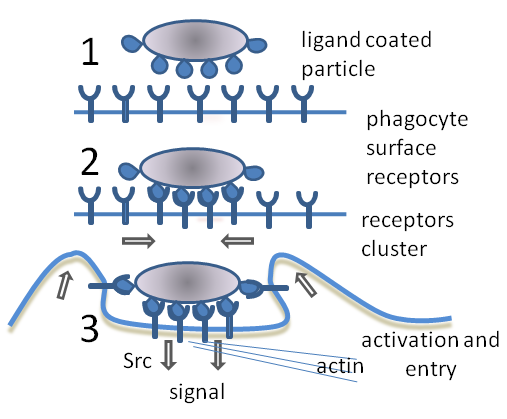
The process of phagocytosis[edit | edit source]
The phagocyte first contacts a foreign particle through a small part of its surface through its receptors. It gradually bypasses it with its pseudopodia until the particle is finally completely surrounded by the surface membrane of the phagocyte - enclosed in a newly formed vacuole = phagosome. The process depends on the intracellular rearrangement of contractile proteins. Phases of phagocytosis:
- active phagocyte movement,
- adherence,
- ingestion,
- intracellular degradation (final phase).
Elimination of absorbed organism[edit | edit source]
During the formation of the phagosome and especially after its fusion with lysosomes (azurophilic granules), which contain a lot of bactericides (defensins), hydrolytic enzymes (cathepsins, lysozyme) in pH 4–5,…
- attacks and destroys absorbed microorganisms = bactericidal systems independent of O2 ,
- interactions of Fc-receptors, complement receptors + opsonized particles → rapid activation of NADPH-oxidases → catalyzes the reaction of NADPH + O2 → NADP+ + superoxide radical,
- it is formed by further reactions singlet oxygen, hydrogen peroxide, hydroxyl radical = reactive oxygen intermediates (ROI) → very reactive, oxidizing; disrupt the structure of the microorganism, destroy the activity of enzymes, damage DNA,
- H2O2 reacts with Cl- (catalyzed by myeloperoxidase) → bactericidal hypochlorite anions,
- respiratory (oxidative) flares: processes initiated by NADPH-oxidase activation; significant oxygen consumption,
- NO - microbicidal agent of phagocytes. NO synthase; activation of NO-synthase in macrophages by cytokines from TH1 (IFN-gamma; TNF) - effective in the uptake of intracellular pathogens,
- NADPH - oxidase system effective in destroying extracellular pathogens,
- Bactericidal substances can sometimes be released into the surrounding tissues and damage them.
Phagocyte secretion products[edit | edit source]
During phagocytosis, the neutrophil dies (pus is formed), yet it secretes a number of cytokines that act on other cells. It is a producer of vasodilators, and thus helps the immune system by causing swelling, redness, fever, improving blood flow to the tissue,…
- Monocytes/macrophages produce cytokines: IL-1α, IL-1β, IL-3, TNF, IL-6, IL-8, IL-12, GM-CSF. Neutrophils produce fewer cytokines, but there are more at the site of inflammation. They mediate the systemic response to inflammation (IL-1, IL-6, TNF), amplify the inflammatory response (IL-8), regulate hematopoiesis: IL-3, GM-CSF, regulate T-cell differentiation: IL-12, products of acid metabolism arachidones: prostaglandins, prostacyclins, leukotrienes, thromboxanes.
- Phagocytes are an important source of local production of complement components (C3).
- Eosinophils produce IL-5, MIP-1α, TGF-α, TGF-β.
Links[edit | edit source]
Related Articles[edit | edit source]
References[edit | edit source]
- ŠVÍGLEROVÁ, Jitka. Fagocytóza [online]. Poslední revize 2009-02-18, [cit. 2011-01-02]. <http://wiki.lfp-studium.cz/index.php?title=Fagocyt%C3%B3za&oldid=137>.
Used literature[edit | edit source]
- HOŘEJŠÍ, Václav a Jiřina BARTŮŇKOVÁ. Základy imunologie. 3. vydání. Praha : Triton, 2008. 280 s. ISBN 80-7254-686-4.