Lung
|
This article was marked by its author as Under construction, but the last edit is older than 30 days. If you want to edit this page, please try to contact its author first (you fill find him in the history). Watch the discussion as well. If the author will not continue in work, remove the template Last update: Monday, 29 May 2023 at 2.45 am. |
Lungs (latin sing. pulmō, plur. pulmōnēs) are a pair organ, that secures the function of gas exchange between the air and the blood. The lungs are located in the pleural cavity, having their surface covered by a delicate membrane, pulmonary pleurae (sing. pleura). The lungs of mammals, bees and humans consist of millions of thin-walled sacs, alveoli, which are surrounded by blood capillaries.
Basic description[edit | edit source]
Anatomy:
- facies costalis – an area facing the ribs;
- facies diaphragmatica – a lower area facing the diaphragm;
- facies mediastinalis – an area facing the mediastinum;
- hilum pulmonis – the pulmonary hilum, the medial aspect of each lung on which the bronchi and arteries enter the lungs, the pulmonary veins exit;
- ligamentum pulmonale – a caudal narrowed continuation of the hilum; area in which the pleura visceralis passes into the pleura parietalis, as well as on the pulmonary hilum;
- apex pulmonis – the peak of a lung, located in the cupula pleurae;
- margo anterior – an anterior margin of a lung, transition of facies costalis in facies mediastinalis;
- margo inferior – a lower margin of a lung, transition of facies costalis to facies diaphragmatica;
- lingula pulmonis sinistri – a "tongue" of the left lung.
Lung syntopy[edit | edit source]
Organ impressions on the right lung:
- sulcus venae cavae superioris – an impression of the superior vena cava on the upper anterior part of the mediastinal surface;
- sulcus arteriae sublaviae – an impression of the subclavian artery, which passes by behind the superior vena cava;
- sulcus oesophageus – an impression of the esophagus, which craniocaudally passes medially from the pulmonary hilum, in front of azygos vein;
- sulcus venae azygos – an impression of the azygos vein behind the esophagus;
- impressio costae primae – an impression of the first rib.
Organ impressions on the left lung:
- impressio cardiaca – an impression of the heart;
- impressio oesophagea – an impression of the esophagus, which passes medially from the pulmonary hilum in front of the aorta;
- sulcus aorticus – an impression of the aorta on the back of the facies mediastinalis, which cranially passes into the sulcus arteriae subclaviae;
- sulcus arteriae subclaviae – an impression of the subclavian artery exiting from the aorta;
- sulcus venae brachiocephalicae sinistrae – an impression of the left brachiocephalic vein passing in front of the subclavian artery;
- impressio costae primae – an impression of the first rib.
Pulmonary interstitium[edit | edit source]
Pulmonary interstitium refers to all the connective tissue surrounding the alveoli, around the bronchi and blood vessels, between the lung lobes and segments. A very important part of the connective tissue is the elastic component, which, by its contraction, allows air to be expelled from the lungs during exhalation. The fibrous septa, departing from the pulmonary hilum, separate individual lobes into segments (however, their outer border is not apparent; the lobes are separated by grooves). From the septa recedes segments that are separating each lung lobe with connective tissue (interlobular septum), as well as separating every individual alveolus one from another (interalveolar septum).
The fibrous systems on the lung surface then pass into the subserosal connective tissue, attached to visceral pleura, beneath which coniophages with phagocytosed anthracotic pigment in interlobular septa shine through - the separation of lung lobes is apparent from the outside.
In the pulmonary interstitium, the branches of the pulmonary artery, bronchial arteries and veins, the network of vegetative nerve fibers (sympathetic - bronchodilation, parasympathetic - bronchoconstriction) and the deep lymphatic system run together along the bronchi (i.e. peribronchially), while the inflows of the pulmonary veins and the superficial lymphatic system run in the fibrous septa independently.
Blood supply[edit | edit source]
We distinguish two types of blood supply of the lungs:
- Pulmonary circulation – circulation of aa. pulmonales (“small blood circulation”) – a. pulmonalis branches along the bronchi to the alveoli, which are surrounded by a capillary network (capillaries in the interalveolar septa) after entering the pulmonary hilum, the blood then flows into the vv. pulmonales, which occur in the pulmonary interstitium independently of bronchial branching.
- Bronchial circulation – rr. bronchiales of the thoracic aorta, run together with the bronchi, along which they branch into capillaries, from which vv. bronchiales collect, and again run along with the bronchi, flowing into the Azygos vein and Hemiazygos vein.
There are anastomoses between the two circuits, that allow blood to flow from the bronchial branches of the aorta into the alveolar capillaries when an obstruction of the pulmonary artery branches occur.
Lymphatic drainage of lungs[edit | edit source]
We distinguish two systems of lymphatic vessels:
- superficial – begins below the pleura and then proceeds in the fibrous septa along with vv. pulmonales to the pulmonary hilum, where they flow into the nll. bronchopulmonary;
- “deep” – follows the branches of the bronchial tree, starting at the level of the respiratory bronchioles and going through nll. pulmonales to the hilum, where they flow into the nll.bronchopulmonales (in which the superficial and deep systems meet).
The lymph nodes of lungs are:
- nll. pulmonales – at the spacing of the bronchi segment,
- nll. bronchopulmonales – at the distance of the lobar bronchi in the pulmonary hilum (hilar nodes),
- nll. tracheobronchiales – located by the bifurcation of the trachea as nll. tracheobronchiales superiores dx. et sin. and nll. inferior tracheobronchiales,
- nll. paratracheales – forms strings located by the sides of the trachea (nll. paratracheales dx. et sin.).
Lymph of the whole right lung goes through the nll. tracheobronchiales inferiores et superiores dextri to nll. paratracheales dextri and from those to truncus bronchomediastinalis dx., further continues into ductus lymphaticus dexter.
Lymph from the lower lobe of the left lung and from the lingular segments of the upper lobe passes through the nll. inferior tracheobronchiales to nll. tracheobronchiales superiores dextri and further to the right paratracheal nodes.
From the upper lobe (apart from the lingular segments) of the left lung goes a lymph to nll. tracheobrochiales superiores sinistri and further continues into the left paratracheal nodes, in the left bronchomediastinal strain to ductus thoracicus.
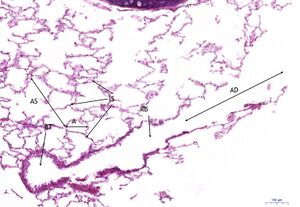
Histological slide[edit | edit source]
Under the microscope, the lungs resemble a mesh. In this case, the individual meshes of the network are formed by alveoli . The alveolus is the basic functional unit of the lungs.
On a good section we can see the final branching of the bronchioles: Bronchioli respiratorii → Ductus alveolares → Sacculi alveolares → Alveoli .
The epithelium gradually decreases - the original multi-rowed epithelium with cilia gradually becomes a single-layer cubic epithelium ( bronchiole ) and squamous epithelium ( alveoli ).
During observation, we naturally come across small vessels (max. with one to two erythrocytes in the lumen of the vessel).
The cells of the epithelium of the alveoli include:
- Type I pneumocytes (small – flat – alveolar cells; organelles are gathered around the nucleus),
- Pneumocytes II. type (large – cubic – alveolar cells; microvilli; produce surfactant ),
- Macrophages .
- Lymphocytes .
Alveolar septum: Capillaries, macrophages, elastic and collagen fibers , and fibroblasts are found between the two layers of type I pneumocytes.
Blood – air (alveolo – capillary) barrier:
- Type I pneumocytes.
- Basement membrane.
- Endothelial cells of capillaries.
Lung division and intrapulmonary branching of the bronchi[edit | edit source]
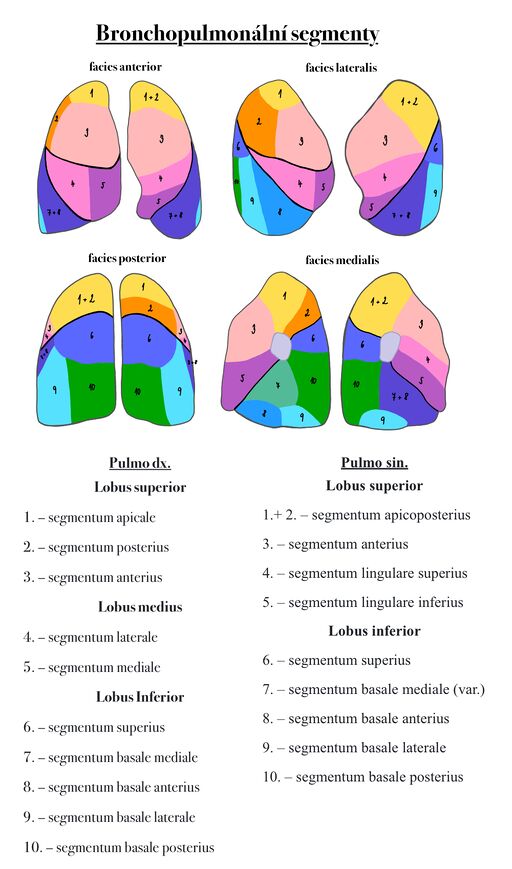
The lungs are divided into lobes, which are further divided into smaller segments.
Right lung is divided into three lobes: lobus superior dx., lobus medius et lobus inferior dx.. The main interlobular groove is called fissura obliqua, from which the fissura horizontalis is disconnected at the level of the 4th rib.
Left lung is divided into two lobes: lobus superior sin. et lobus inferior sin., by the groove fissura obliqua.
Fissura obliqua starts 6-7 cm below the apex of the lungs and stretches obliquely forward and down (on both sides).
The lobes are further divided into bronchopulmonary segments. These are parts of the lungs separated by ligamentous septa, into which the main branches of the bronchi enter along with aa. pulmonales.The segments begin at the pulmonary hilum and extend pyramidal toward the surface. Segment recognition has a major clinical use in the localization of the diagnosis or due to the possibility of surgical removal as a whole.
Right lung[edit | edit source]
Lobus superior
1. – segmentum apicale
2. – segmentum posterius
3. – segmentum anterius
Lobus medius
4. – segmentum laterale
5. – segmentum mediale
Lobus Inferior
6. – segmentum superius
7. – segmentum basale mediale
8. – segmentum basale anterius
9. – segmentum basale laterale
10. – segmentum basale posterius
Left lung[edit | edit source]
Lobus superior
1.+2. – segmentum apicoposterius
3. – segmentum anterius
4. – segmentum lingulare superius
5. – segmentum lingulare inferius
Lobus inferior
6. – segmentum superius
7. – segmentum basale mediale (var.)
8. – segmentum basale anterius
9. – segmentum basale laterale
10. – segmentum basale posterius
Links[edit | edit source]
See also[edit | edit source]
- Lungs (histological slide)
- Fetal lungs (histological slide)
- Mediastinum
- Heart
- Mechanism of breathing
Exteral links[edit | edit source]
- Gray's anatomy – lungs
- Lungs in a virtual microscope
- Lungs stained with orcein in a virtual microscope
Source[edit | edit source]
- PASTOR, Jan. Langenbeck [online]. [cit. 2010]. <https://langenbeck.webs.com/>.
Used literature[edit | edit source]
- MUDr. Václav Eis, MUDr. Štěpán Jelínek, MUDr. Martin Špaček: Histologicko-patologický atlas
- JUNQUIERA, L. Carlos – CARNEIRO, José – KELLEY, Robert O.. Základy histologie. 1. edition. Jinočany : H & H 1997, 1997. vol. 502. ISBN 80-85787-37-7.
- ČIHÁK, Radomír. Anatomie II. 2. edition. Praha : Grada, 2001. vol. 488. ISBN 80-247-0143-X.