Breast tumours
From WikiLectures
It is one of the most common tumors in general. They form two basic groups:
- benign tumors;
- malignant tumors.
Benign breast tumors[edit | edit source]
Malignant breast tumors[edit | edit source]
They are the most common malignant tumors of women in the Czech Republic, their incidence is still increasing.
Epidemiology[edit | edit source]
- Incidence is rising, but mortality is not rising because they are diagnosed at earlier stages;
- peak incidence is around age 57;
- In men, it occurs at a ratio of 1:140.
Etiology[edit | edit source]
- Age is the most serious risk (incidence rises from 30 years of age, with 85% of tumors above 45 years of age);
- Sporadic carcinomas - dysplastic changes of epithelial cells (carcinoma in situ) occur until cancer develops;
- but also involves the activity of stromal cells, which produce proteolytic enzymes and angiogenic factors-facilitating growth and metastasis;
- hormonal effects - long-term effects of estrogens;
- genetic carcinomas - occurrence in direct relatives (mother, sister, daughter) or accumulation of tumors within syndromes (Li-Fraumeni syndrome - mutation of one p53 allele, Cowden syndrome - rare, associated with hamartomas);
- the gene BRCA 1 and 2 is of greatest importance for the detection of genetic susceptibility;
- a woman with a BRCA 1 mutation has a lifetime risk of 55-85% for cancer (15-45% for ovarian cancer);
- common in the Jewish population;
- male BRCA carriers are in turn at risk for prostate cancer and colorectal cancer;
- hereditary cancer is often bilateral;
- BRCA 2 positive carcinoma is usually very poorly differentiated, aggressive.
Risk factors: =[edit | edit source]
- length of exposure to estrogens - early menarche, late menopause, nulliparity;
- other breast disease - cystic adenomas, ductal papillomas (risk of missed carcinoma);
- effects of ionizing radiation - also mammography;
- obesity, increased fat intake and lack of exercise;
- the effect of smoking, chemicals, hormonal contraceptives has not been clearly documented.
Clinical manifestations[edit | edit source]
- Most commonly, it is a palpable, painless lump in the breast (in 75% it is the first manifestation of the disease);
- Optimally, however, a non-palpable lesion should be found on mammography;
- other symptoms (less common) - breast pain (5%), breast enlargement (1%), skin or nipple retraction (5%), discharge (2%), superficial changes on the nipple (1%);
- enlargement of axillary nodes - regional spread;
- at advanced stage - bone pain, weight loss,...
- paraneoplasia - dermatomyositis, neuromuscular syndrome, acanthosis nigrans, hypercalcemia in bone metastases.
Diagnostics[edit | edit source]
Clinical examination:[edit | edit source]
- Careful personal, family and gynecological medical history;
- appearance - symmetry of the breasts, symmetry with breathing, nipple regularity, skin color, vein enlargement may indicate tumor activity;
- palpation - systematically all quadrants, size of resistance, mobility, border, consistency;
- frequency of findings of carcinomas in each quadrant - most often HZK (47%), nipple (22%) and HVK (14%), lower quadrants few;
- palpation of nodes axillary, above the germ.
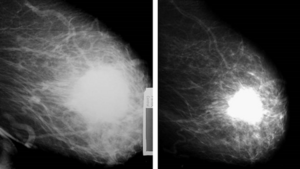
Imaging methods:[edit | edit source]
- mammography is dominant - the yield is up to 90%;
- finding - microcalcifications are usually visible, solid lesion with serrated edges;
- ultrasound - usually complementary to mammography, has high sensitivity (95%) but limited specificity, preferred in women under 40 years of age;
- CT, MRI, less so ductography, PET.
Biochemical testing:[edit | edit source]
- standard - liver tests, urea, creatinine, electrolytes,
- tumor markers - CEA, CA 15-3, TPA;
- of particular importance is the determination of hormone receptors - by immunohistochemistry in tissue sections; the influence of estrogen and progesterone on tumor growth is assumed
- molecular biology - especially determination of HER-2/neu - causes increased proliferative activity (prognostic and predictive significance);
- biopsy - fine needle aspiration (FNA) - more important to differentiate between cystic and solid masses;
- histology is only possible with a self-cutting needle (core biopsy) under anaesthesia (local or general).
Screening:[edit | edit source]
- early diagnosis is the basis for successful treatment;
- mammography screening for women 45 and older (once every two years)[1].
Histopathology[edit | edit source]
- Carcinoma most commonly arises from the terminal ductal lobular unit (TDLU);
- It is usually preceded by a non-invasive form - carcinoma in situ.
Carcinoma in situ[edit | edit source]
- Lobular carcinoma in situ' - from mammary lobule cells, proliferation of cells in lobules that dilate;
- not detectable mammographically (unlike the previous one);
- often arises multicentrically, even in the contralateral breast;
- more common in premenopausal women.
- Ductal carcinoma in situ' - proliferation of ductal epithelium without crossing the basement membrane, may form microcalcifications (detectable mammographically), may progress to invasive ductal carcinoma;
- a special form is Paget's carcinoma of the nipple - when tumor cells from the ducts invade the nipple, more often in postmenopausal women.
Invasive forms of carcinoma[edit | edit source]
- There are different forms, infiltrating is divided into 2 forms - lobular and ductal.
- Lobular
- about 10%, often in the HZK (upper outer quadrant);
- often metastasizes to serous membranes, meninges, ovaries, retroperitoneally.
- Ductal
- the most common (75%), often tubular, accompanied by reactive fibrosis - the tumor has a form where it is hard as a stone;
- metastasizes to bone, liver and lungs;
- Inflammatory (erysipeloid) carcinoma
- rare (1-3%), the most aggressive form;
- infiltration of the entire breast, diffuse erythema, skin induction (typical orange peel appearance);
- 50-70% of tumors have nodal metastases at the time of diagnosis.
Treatment[edit | edit source]
The final treatment is the result of a joint decision by a multidisciplinary team.
Surgical treatment[edit | edit source]
- Since 1882, radical mastectomy with exenteration of the axilla (pectoral muscles, nerves, ...) has been performed;
- Nowadays, modified radical mastectomy is more commonly performed - the breast is separated from the pectoralis fascia, the nodes are removed from the superficial stages, the nodes below the m. pectoralis minor are usually not removed;
- another variant - sentinel node;
- salvage procedures - quadrantectomy, tumorectomy;
- necessary to complement radiotherapy, reconstructive surgery is performed;
- also as a modality of hormonal treatment - ovarectomy;
- for BRCA, surgery can also be used as prophylaxis.
Radiotherapy[edit | edit source]
- Carcinoma has limited radiosensitivity;
- it is indicated after salvage surgery, the result is then identical to ablation;
- it is therefore given adjuvantly;
- brachyradiotherapy - application of iridium wires;
- palliative treatment - for bone metastases.
Chemotherapy[edit | edit source]
- Breast cancer is relatively sensitive to a range of cytostatics, and combinations are mainly used;
- the basic combination is CFM - cyclophosphamide, methotrexate, 5-FU, or combination with anthracyclines;
- monotherapy - in older women with limited marrow reserve;
- adjuvantly - before menopause always when lymph nodes are involved, not given for carcinoma in situ or for tumors under 1 cm;
- neoadjuvant - for large tumors;
- palliation - the main treatment method for disseminated disease, can significantly prolong survival.
Hormone Therapy[edit | edit source]
- Adjuvant, neoadjuvant and palliative treatment;
- in premenopausal - castration - surgical or pharmacological.
- SERM - Tamoxifen
- Aromatase inhibitors - reduction of female sex hormone synthesis
Biological treatments[edit | edit source]
Links[edit | edit source]
Related articles[edit | edit source]
- Breast
- Hereditary cancer syndromes
- Benign breast disease
- Tabar classification of breast cancer
- Breast Cancer Classification BI-RADS
- Diagnostic Imaging in Senology
- Infiltrating Mammary Carcinoma (slide)
External links[edit | edit source]
Reference[edit | edit source]
- ↑ Česká republika. Vyhláška 3/2010 Sb. o stanovení obsahu a časového rozmezí preventivních prohlídek. 2010. pp. 10 §4 písm. i. Available from <http://www.mamo.cz/res/file/legislativa/vyhlaska-3-2010.pdf>.