BRCA
BRCA (BR east CA ncer) are tumor suppressor genes. It is found in the body in two types, BRCA1 and BRCA2. The products of these genes are involved in cell cycle control and repair of damaged DNA. The mutation increases the risk of cancer, especially of the breast and ovaries.
| BRCA1, BRCA2 | |
| BRCA1 17q21.31, BRCA2 13q3.1 | |
| Associated diseases | HBC (hereditary breast cancer syndrome) and HBOC (hereditary breast/ovarian cancer syndrome) |
|---|---|
| Function | tumor suppressor genes |
| OMIM | BRCA1 113705
BRCA2 600185 |
| HGNC | BRCA1 1100
BRCA2 1101 |
Genetic background[edit | edit source]
BRCA1 is located on the long arm of chromosome 17 and has 22 exons. The product is a large pBRCA1 protein (220 kDa). BRCA2 is located on chromosome 13q. The product is a 384 kDa pBRCA2 polypeptide.[1] The pBRCA1 and pBRCA2 proteins are found in the nucleus. They contain binding domains that allow them to interact with other proteins. A proven interaction is binding with the product of the RAD51 gene.
Principle of action[edit | edit source]
Functions of BRCA gene products.
The product of the AT gene reacts to DNA damage. The protein kinase ATM initiates a phosphorylation cascade during which the pBRCA1 protein is phosphorylated. The latter subsequently interacts with the protein pRAD51, which participates in the repair of DNA double-strand breaks through the process of homologous recombination. The pBRCA2 protein also interacts with this complex. Its role is to transport pRAD51 to the site of damage.
Mutation[edit | edit source]
Mutations in the BRCA1 and BRCA2 genes are inherited in families in an autosomal dominant manner with high penetrance. The frequency in the population is approximately 1:800.[2] Inherited mutations in these genes are responsible for HBC (hereditary breast cancer syndrome) and HBOC (hereditary breast/ovarian cancer syndrome). In the population, 3-5% of breast malignancies are caused by gene abnormalities. Mutations in the BRCA genes are involved in the development of approximately 2/3 of hereditary tumors.[3] Detected mutations have multiple consequences.[1]
- Deletion of 11bp in exon 2 or insertion of 1bp in exon 20 leads to frameshift.
- A mutation in exon 11 leads to the inclusion of a stop codon (nonsense mutation).
- A missense mutation in exon 21 replaces methionine with arginine in the finished polypeptide.
- The regulatory region can also be affected by the mutation, which means that these genes may not be transcribed at all.
Prognosis[edit | edit source]
The lifetime risk of developing life-threatening tumors is very high in women who carry mutations. DCIS (ductal carcinoma in situ) develops 10-15 years earlier in female patients. Invasive tumors appear 15-20 years earlier compared to sporadic ones. A relatively characteristic feature of tumors is that they do not express hormone receptors.[3]
| Gene | Breast cancer risk | Risk of ovarian cancer |
|---|---|---|
| BRCA 1 | 87% | 40-60% |
| BRCA 2 | 87% | 23% |
Cancers associated with BRCA gene dysfunction also include cancer of the uterus, pancreas, prostate, colon, rectum and skin (malignant melanoma).
Indications for examination[edit | edit source]
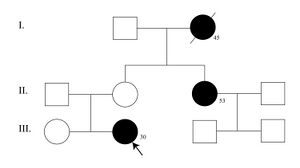
Family tree diagram with BRCA mutation
The examination can be performed on the basis of an already diagnosed tumor in patients according to the following criteria[2]:
- breast or ovarian cancer diagnosed before the age of 35;
- breast cancer in a man at any time during life (other possible causes must be excluded);
- breast and ovarian cancer in one patient at the same time (tumor duplication);
- bilateral breast cancer (first lesion diagnosed before age 40).
Patients with a burdensome family history can also be tested[2]:
- two first-degree relatives (through the second-degree father) with breast or ovarian cancer (at least one diagnosed before the age of 50);
- three or more breast or ovarian cancers in first and second degree relatives in one line regardless of age.
Testing of healthy family members of people who have tested positive is subject to a code of ethics. A daughter from a positively tested woman can be offered an examination from the age of 18.
Diagnostics[edit | edit source]
The initial selection of persons with a probable mutation in genes is usually carried out on the basis of family anamnesis. During the consultation with the geneticist, a family tree should be drawn up, which includes the occurrence of tumors (especially of the breast or gynecological area) in previous generations in the younger age category. Individual workplaces have slightly different criteria for subsequent testing of the presence of mutations using molecular genetic methods. If a patient has a confirmed specific mutation in previous generations, he is usually tested for it. A negative test result therefore means that the patient does not have the given tested mutation (or several of the most frequently tested). However, this does not exclude the possibility of a private mutation, i.e. one that has not yet been detected in the population. More than 300 mutations of the BRCA1 gene are currently identified, of which 50% are private.[1]
Therapy[edit | edit source]
For healthy carriers of the mutation, monitoring is recommended from the age of 20. Male carriers are monitored from the age of 30. In women, it is possible to propose preventive mastectomy and adnexectomy. The risk of breast cancer is reduced to 1-5% after the procedure. Patients are monitored according to the recommended scheme.[4]
| Age | Examination | Frequency |
|---|---|---|
| 20 years | breast self-examination | 1x per month |
| clinical breast examination | 1x in 6 months | |
| breast ultrasound | 1x in 6 months | |
| tumor markers CA 125, CEA, CA 15.3 | 1x per year | |
| skin examination | 1x per year | |
| 21 years | transvaginal ultrasound | 1x in 6 months |
| 25 years | magnetic resonance imaging of the breast | 1x per year |
| 30 years | mammography | 1x per year |
| transcutaneous ultrasound of the abdomen | 1x per year | |
| 40 years | blood culture test | 1x per year |
| 45 years | colonoscopy | 1x 3 years |
Links[edit | edit source]
[edit | edit source]
- Repair mechanisms of the organism and their genetic control
- Tumors with a familial occurrence
- Breast tumors
- Disorders of DNA repair mechanisms in tumor cells
External links[edit | edit source]
- Homologous recombination - https://www.youtube.com/watch?v=raXCU1dFYiw
Reference[edit | edit source]
- ↑ a b c SNUSTAD, D. Peter – SIMMONS, Michael J.. Genetika. 1. edition. Masarykova univerzita, 2009. 871 pp. pp. 681–685. ISBN 978-80-210-4852-2.
- ↑ a b c KUCHYŇKA, Petr. Onkogyn.cz [online]. [cit. 2017-04-01]. <http://onkogyn.cz/informace-pro-lekare/dedicne-syndromy-26/proc-testovat-prave-geny-brca-a-brca-89/>.
- ↑ a b PAVLIŠTA, David. Neinvazivní karcinomy prsu. 1. edition. Maxdorf s.r.o, 2008. 181 pp. pp. 34–41. ISBN 9788073451738.
- ↑ ADAM, Zdeněk – KREJČÍ, Marta. Obecná onkologie. 1. edition. Galén, 2011. 394 pp. pp. 29–31. ISBN 978-80-7262-715-8.
Used literature[edit | edit source]
- SNUSTAD, D. Peter – SIMMONS, Michael J. Genetika. 1. edition. Masarykova univerzita, 2009. 871 pp. ISBN 9788021048522.
- PAVLIŠTA, David. Neinvazivní karcinomy prsu. 1. edition. Maxdorf s.r.o, 2008. 181 pp. ISBN 9788073451738.
- NEČAS, E. Obecná patologická fyziologie. 1. edition. Karolinum, 2007. 377 pp. ISBN 80-246-0051-X.
- ADAM, Zdeněk – KREJČÍ, Marta. Obecná onkologie. 1. edition. Galén, 2011. 394 pp. ISBN 978-80-7262-715-8.