Prostate cancer
Prostate cancer is the third most common malignancy in men in the Czech Republic (after lung and colon cancer). They make up about 4% of all tumors. There are significant geographical and racial differences. The risk of the disease is 70% higher in blacks in the USA than the risk of the disease in whites. In contrast, the risk of disease in Asians is 3 times lower than the risk of disease in Caucasians (lower 5-alpha reductase activity). In the Czech Republic, the incidence is approximately 100 / 100,000 and increases with age - most often in the 7th and 8th decade. Autopsy findings show that only about 10% of cases manifest during life.
Risk factors for the development of the disease include:
- Age - sections show that 70% of men over the age of 90 have at least one prostate cancer.
- Genetic factors - it is assumed that up to 9% have AD heredity, direct relatives of the first degree of the affected person have a higher risk.
- Hormonal - action of DHA (dihydroandrosterone), testosterone is not directly related to carcinogenesis, but may be involved in the manifestation (incidence is very low in eunuchs).
- Diet - high intake of animal fats, red meat.
- Sexual activity - promiscuity and STD .
- Professional - exposure to X-rays, pesticides, some heavy metals (eg cadmium).
Clinical picture[edit | edit source]
Prostate cancer is initially asymptomatic . Mainly because prostate cancer comes from 80% of the peripheral zone of the prostate, less often from the transitional zone (10% - 20%) and rarely from the central zone (less than 5%). Significant clinical manifestations are a sign of advanced cancer .
Symptoms of local progression include urinary tract irritation or ingrowth and may manifest as
- dysuria ,
- nocturia ,
- polakisuria ,
- acute urinary retention (up to 25% of patients),
- less often hematuria .
Signs of generalized disease include :
- pain from bone metastases (back, hips, limbs),
- lower limb paresis (mainly due to extradural spinal cord compression by metastasis in the spine),
- anorexia,
- weight loss,
- general weakness.
Metastasis[edit | edit source]
The tumor spreads mainly lymphogenically and establishes metastases in the lymph nodes of the pelvis, aorta and above the left germ. If the cancer grows into a blood vessel, then metastases occur mainly in the bones (typically osteoplastic metastases), lungs, liver, CNS, adrenal glands, and kidneys. The tumor can also spread per continuity , ie. it can spread locally to the surrounding soft tissues, bladder and seminal vesicles.
The risk of metastasis increases if the tumor grows through the wall (T3 already has 50% metastases).
Diagnostics[edit | edit source]
The cheapest and most used is the rectal examination . Although this examination covers only a third of the prostate surface, it serves as a method of first detection . As a precautionary measure, every man over the age of 40 should undergo the examination at least once a year.
Serum PSA levels are determined next . Its values vary with age (5th decade 4.1 ng / ml, 6th decade 5.6 ng / ml), and correspond to prostate size (PSA increases by 4% for each gram of prostate). PSA is sensitive but non-specific. An artificially high PSA can be, for example, after rectal examination, cycling, riding (whenever the prostate can be traumatized). It takes several weeks to return to the norm.
The determination of PSA levels does not yet function as a nationwide screening, it is considered for risk groups of the population.
In practice, the level of the prostate fraction of acid phosphatase in the blood is determined. Its values increase mainly during metastases.
Tissue biopsy and histological classification are required to definitively confirm the diagnosis .
Imaging methods:
- TRUS - transrectal US , which assesses the volume of the lesion and its relationship to the environment, helps with targeted biopsy. The assessment is often complicated, an assessment computer program has been developed for this.
- CT - does not help much in the description of the primary site, but is important for nodal metastases.
- MRI - specifies the size of the bearing and the relationship to the surrounding structures.
- SPECT and PET
- Other methods: excretory urography (in diff. Dg. Hematuria), skeletal scintigraphy.
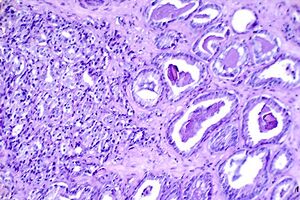
Histopathology[edit | edit source]
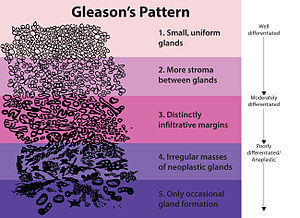
Gleason's score In practice, the so-called Gleason score is used , which evaluates the architecture of the glands at 5 degrees . In the scale, G1 is well differentiated and G5 is very poorly differentiated.
The score is read by the pathologist and its value is based on the sum of two degrees of cell differentiation, the most represented degree and the least differentiated. The result is a value of 2-10, where over 7 is already high risk .
Histologically, we recognize several types of malignancies:
- adenocarcinoma, which is most commonly acinar (up to 95%) and typically occurs in the peripheral region of the gland;
- small cell carcinoma that does not produce PSA;
- urothelial cancer;
- squamous cell carcinoma;
- sarcoma, which is rare.
Therapy and prevention[edit | edit source]
The extent, grade, age and general condition of the patient must be taken into account. In old men with a well-differentiated, localized, small tumor, a follow-up can be chosen (watchful waiting) (Gleason score up to 4, volume up to 1 cm 3 )
Surgery[edit | edit source]
It is the main treatment method for localized forms (T1, 2). Radical prostatectomy is performed (removal with a capsule).
Radical prostatectomy is the removal of the prostate, along with a surgical sheath and seminal vesicles! Thus, there is a difference compared to surgery for benign prostatic hyperplasia, in which it removes only the benign transient zone of the prostate without a surgical sheath. (Note. Essential for the exam.)
There are several ways to use this:
- retropubic (better overview of the operating field, possible preservation of potency);
- perineal (in the elderly, less surgical burden);
- laparoscopy;
- TURP (transurethral resection of the prostate);
Radiotherapy[edit | edit source]
- Teleradiotherapy - a useful method, but it has a lot of side effects (ADR).
- Conformal therapy - increases efficiency and minimizes NU in three-dimensional planning. In localized tumors where there is KI surgery, radiotherapy may produce the same results as surgery.
- Brachyradiotherapy is a transrectal or transperineal application of radionuclide grains, there is a problem with ensuring homogeneous irradiation, it is rarely used.
- Adjuvant radiotherapy is recommended for locally advanced disease, as well as for the prevention of recurrence and eradication of metastases in the nodes.
- Palliative radiotherapy has an irreplaceable place in the comprehensive treatment of prostate cancer, especially as analgesia in bone metastases.
Hormone therapy[edit | edit source]
- Neoadjuvant - in locally advanced disease, androgen deprivation can cause a reduction in prostate volume of up to 36% (down staging). Even so, it is not used very often - periprostatic fibrosis can occur, complicating surgery or additional costs;
- Adjuvant - after surgery or RT, when high PSA levels persist, otherwise it is not used;
- Treatment of metastases - here, on the contrary, is the method of choice. The basis is orchiectomy, which leads to a decrease in androgens or pharmacological castration (LHRH agonists and antagonists - is much more expensive). Flare phenomenon - after the use of LHRH analogue , testosterone temporarily rises , which leads to worsening of the problem, the decrease occurs after about 3 weeks. Even after castration, the production of DHEA and androstenedione persists in the adrenal glands, so castration is combined with the administration of antiandrogens. The administration of antiandrogens alone is inappropriate.
- Chemotherapy - is indicated in case of loss of sensitivity to hormonal treatment. The sensitivity of the prostate to CHT is relatively limited. Patients are usually old, in poor condition, and there are many adhesions in the tumor area after surgery, and this limits the access of the cytostatic. Alkylating agents and interalkylating agents (doxorubicin, epirubicin) appear to be the most effective.
- Immunotherapy - is starting to be used in recent years, Ig is tested against the membrane epitope PSA, Ig against EGF or against VEGF ...
See the Hormone Therapy page for more information .
Treatment algorithm a (five-year survival)[edit | edit source]
- Stage 0 - watch and wait, in younger as I (90%)
- Stage I and II - radical surgery + adj. RT (60-80%)
- Stage III - primary RT + hormonal treatment (15-50%)
- Stage IV - locoregional - RT, hormone. therapy, or palliative surgery
- Metastases - hormonal treatment, palliative RT, ev. surgery or CHT (5-30%)
Links[edit | edit source]
[edit | edit source]
External links[edit | edit source]
- MEFANET Urolithiasis, urooncology, retroperitoneal diseases, lower urinary tract diseases
Reference[edit | edit source]
- ↑ POVÝŠIL, Ctibor, Ivo ŠTEINER and Jan BARTONÍČEK, et al. Special pathology. 2nd edition. Prague: Galén, 2007. 430 pp. ISBN 978-807262-494-2 .
- ↑ KRÁL, Milan, Vladimír ŠTUDENT and Vladimíra KURFÜRSTOVÁ. Gleason score in biopsy and after radical prostatectomy - changes after the ISUP 2005 conference and significance for the urologist. Urology for practice [online] . 2007, vol. 8, vol. 4, pp. 173 to 178, also available from < https://www.urologiepropraxi.cz/pdfs/uro/2007/04/07.pdf >. ISSN 1803-5299.
Source[edit | edit source]
- KOCAK, Ivo. Prostate cancer [online]. © 2006. [feeling. 2013-11-26]. <www.mou.cz/4-3-karcinom-prostaty/f86>.
- BENEŠ, Jiří. Study materials [online]. © 2010. [feeling. 2009]. < http://jirben.wz.cz >.
References[edit | edit source]
- ZEMAN, Miroslav, et al. Special surgery. 2nd edition. Prague: Galén, 2004. 575 pp. ISBN 80-7262-260-9 .
- SAMEŠ, Martin, et al. Neurosurgery: Textbooks for medical faculties and postgraduate studies in related fields. 1st edition. Prague: Maxdorf, 2005. 127 pp. 79. ISBN 80-7345-072-0 .