Arteriovenous malformations
Arteriovenous malformation (AVM) is a congenital convolute (bundle) of dilated vessels in which arterial blood flows directly into the drains, which lack a normally developed capillary system. They can be congenital (98%) or acquired (2%). These malformations can occur anywhere in the body, but they are the most common in the brain and cause even the most significant problems [1]. This article, therefore, focuses on AVM in the CNS.
AVM classification[edit | edit source]
Based on the morphological arrangement, we divide:
- AVM with compact (glomerular) nid – typically these are abnormal vessels without the presence of brain tissue, they occur more often than the diffuse type.
- AVM with diffuse (proliferative) nid – there is no well-formed nidus with functional neuronal tissue that would be scattered between anomalous vessels.
S-M grading[edit | edit source]
In the clinic, we encounter a classification known asS-M grading according to the authors R. Spetzler and N. Martin. By scoring, the size of the malformation, the type of venous drainage, and whether the AVM is located in a functionally important area of the brain are assessed. According to this classification, we divide AVM into five levels: [2]
- Low-grade – grade I, II a III (1–3 points),
- High-grade – grade IV a V (4–5 points).
| Parametr | Points | |
|---|---|---|
| AVM nide size | ||
| <3 cm | 1 | |
| 3–6 cm | 2 | |
| >6 cm | 3 | |
| Deep venous drainage | ||
| No | 0 | |
| Yes | 1 | |
| Functionally important area | ||
| No | 0 | |
| Yes | 1 |
Angioarchitecture[edit | edit source]
The AVM usually has a confined center (nidus – Latin "nest") and dilated supply arteries along with wide drainage veins that are filled with arterialized blood. This type of vascular malformation lacks capillary flow resistance, so the flow is quite high.
Epidemiology[edit | edit source]
The incidence in the population is relatively low, newly diagnosed cases reach the value of 1-1.5 cases per 100,000 inhabitants. AVM most often manifests itself at a younger age, typically between the ages of 15 and 20. year of life. [7]
Localization[edit | edit source]
CNS[edit | edit source]
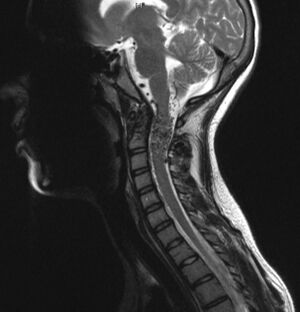
In the brain, AVMs are localized, AVMs are localized (86 %), of which those in the neocortex, the deeply deposited AVM's (diencephalon, basal ganglia, capsula interna etc.) and combined AVM's archi- and paleocortex lead in incidence. Infratentorial AVMs are uncommon, affecting mainly the neocerebellum and brainstem, and cases of intraventricular AVMs. 80% of spinal AVMs are intramedullary or extramedullary. [8]
Hemorrhage from AVM is approximately 30% subarachnoid, 23 % intraparenchymal,16% intraventricular, and 31% is a combination of these. [9]
Other locations[edit | edit source]
Other areas of AVM include:
For more details related to AVM in these localizations, see the external links at the end of this article.
Diagnostics[edit | edit source]
CT[edit | edit source]
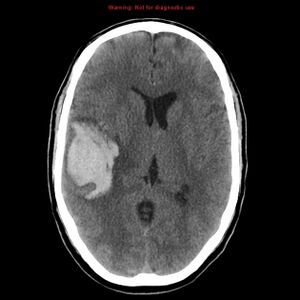
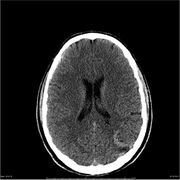
It is often performed as the first imaging method in patients with acute neurological deficits, but without the use of contrast, the accurate diagnosis of AVM is relatively complicated. Nidus AVM without previous bleeding is hyperdense to the surrounding brain tissue. After administration of a contrast agent (especially in CTA), the diagnosis is clearer, but angiography is recommended for more detailed imaging of the arteries. In the case of an AVM rupture, the CT is sensitive enough to image an acute hematoma.
- CT - difference in AVM diagnosis when contrast was administered / not
MRI[edit | edit source]
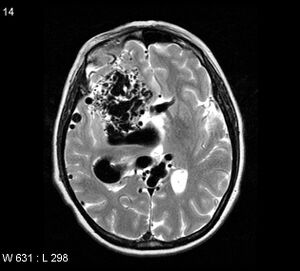
MRI is especially important for a clear view of the surrounding structures and their possible damage, and any adjacent edema is well recognizable. Compared to CT, MRI better determines the exact anatomical location of the nid as well as any previous hemorrhage. [10]
MRA[edit | edit source]
MRA sequences play an important role in displaying three-dimensional angiographic images of AVM. The TOF MRA method is typically one of the first examinations of a given malformation, showing very well most supply arteries and nidus lesions. However, it is often complicated to distinguish supply arteries from venous drainage, especially in AVMs with a more complex arrangement. In addition, it is not very sensitive to smaller AVMs and associated aneurysms. [11][12]
Angiography – DSA[edit | edit source]
Digital subtraction angiography (DSA) is the gold standard for detailed AVM diagnostics. This malformation appears on angiography as tightly packed masses of enlarged surrounding arteries that supply the nidus of the malformation. The DSA will provide a detailed description of the supply arteries and associated angiopathic changes, an accurate evaluation of the nid (its size, hemodynamic properties, anatomical characteristics), and the definition of venous drainage (deep or superficial), as well as any signs of stenotic changes or ectasia. If hemorrhage is noted in the malformation, the hematoma typically compresses the nidus, increasing intranidal vascular resistance. The result can be a "delay" in venous outflow and AVM can become angiographically occult – the malformation is anatomically present but does not appear on the angiography. [13]
Associated abnormalities[edit | edit source]
The most commonly observed abnormality associated with AVM is aneurysms, which typically result from increased blood flow through malformations. They can occur outside the nid (intranid - present in up to 41-100% of patients with AVM) or on the supply vessels (intrapedicular). Alternatively, non-AVM aneurysms may appear as part of the diagnostic test. appear as part of the diagnostic test.
Furthermore, flow angiopathy is relatively common secondary to endothelial hyperplasia.
Symptomatology[edit | edit source]
The presentation of these vascular malformations is very diverse. Some AVMs may be asymptomatic for a long time , and some patients may have posthemorrhagic neurological deficits, headaches or seizures. Heart murmurs have been reported in some patients.
We often encounter the so-called steal syndrome – - the arteries supplying the AVM "steal" around the vessel, which can result in ischemia of areas whose supply has been redirected to the AVM.
Therapy[edit | edit source]
AVM therapy is a prime example of multimodal cooperation in several branches of medicine. AVM can be surgically resected, irradiated radiosurgically, or embolized endovascularly. Often, multiple treatment alternatives can be applied to a single patient to achieve the most appropriate outcome with the lowest possible morbidity. Of course, observation is a legitimate procedure if the risk of rupture is not very high and the malformation itself does not cause serious problems for the patient.
- Surgical resection – especially for smaller and superficially stored malformations, the advantage is the immediate elimination of the circulation and thus definitive treatment, complete resection is necessary, and thanks to resection, possible elimination of epileptic focus.
- gamma knife radiosurgery – usable for AVM nidus up to 2.5–3 cm in diameter, for deep-seated lesions, the advantage is a non-invasive technique, the disadvantage is the gradual closure of the malformation for 1–3 years (during this time the patient is at risk of bleeding from AVM).
- AVM endovascular embolization – rarely used alone, the goal is usually to close the superficial part of the nid and the main supply arteries.
Complications[edit | edit source]
In the case of observation, the biggest complication is bleeding. The risk of haemorrhage in patients without previous bleeding is approximately 2-3% % [14]. Hemorrhage from AVM (unlike cavernous malformations ), can have fatal consequences due to its morphological arrangement - a post-hemorrhagic 30% mortality and a 10–20% probability of persistent neurological deficits are reported in the literature [15]. V In some cases, cerebral ischemia, can occur, with AVM ruptures representing approximately 1-2% of all cerebral ischemias. The presence of aneurysms is also common in the area of the nidum (or on the supply vessels), which tend to rupture due to the rate of blood flow through the malformations.
Surgical resection is difficult, often several hours, but has very good results (with radical resection) with regard to the long-term prognosis of the patients. The goal of resection is to achieve a complete resection that automatically provides the patient with zero risk of future bleeding from a given AVM. Some morbidity may occur postoperatively, but in most patients it resolves over time - only a fraction (approximately 7% on average) of patients have persistent morbidity [15].
Patients suitable for radiosurgery should not be at high risk of hemorrhage - the effect of treatment does not appear immediately after irradiation, so the patient is still at risk of bleeding from AVM for a relatively long time. It is possible to use the AVM first and then operate - experience with this procedure varies, some workplaces operate after radiosurgery only if the irradiation was not effective enough, and others help radiosurgery before surgical resections because malformations usually do not bleed so much after irradiation, etc.
The most common complication of endovascular embolization is again hemorrhage (arterial perforation may occur during microcatheter insertion or AVM rupture, etc.). Furthermore, there is a risk of thrombus formation and migration to the surrounding cerebral areas, which can result in ischemia.
Video library[edit | edit source]
Links[edit | edit source]
Related articles[edit | edit source]
- Hemorrhagic strokes
- Cavernous malformation
- Bleeding into the internal capsule
- Treatment of intracranial aneurysm
- Subarachnoid hemorrhage
- Intracerebral hemorrhage
- Intracranial hypertension
- Brain ischemia
- Bleeding
- Gamma knife
External links[edit | edit source]
- Cerebral AVM
- Classification of spinal AVM
- Spinal AVM
- Pulmonary AVM
- Renal AVM
- Michael T. Lawton - Lecture on AVM surgical treatment
References[edit | edit source]
- SAMEŠ, M, et al. Neurochirurgie. 1. edition. Praha : Jessenius Maxdorf, 2005. ISBN 80-7345-072-0.
- SMITH, Frank. Neurology and Neurosurgery : Basic Principles. - edition. University Rochester Press, 2002. 528 pp. ISBN 9781580460842.
- BENEŠ, Vladimír – BRADÁČ, Ondřej. Brain Arteriovenous Malformations : Pathogenesis, Epidemiology, Diagnosis, Treatment and Outcome. - edition. Springer International Publishing, 2017. 241 pp. ISBN 9783319639635.
References[edit | edit source]
- ↑ COX, Joshua – BARTLETT, Erica – LEE, Edward. Vascular Malformations: A Review. Seminars in Plastic Surgery. 2014, y. 02, no. 28, p. 058-063, ISSN 1535-2188. DOI: 10.1055/s-0034-1376263.
- ↑ SPETZLER, Robert F. – MARTIN, Neil A.. A proposed grading system for arteriovenous malformations. Journal of Neurosurgery. 1986, y. 4, no. 65, p. 476-483, ISSN 0022-3085. DOI: 10.3171/jns.1986.65.4.0476.
- ↑ STARKE, Robert M. – YEN, Chun-Po – DING, Dale. A practical grading scale for predicting outcome after radiosurgery for arteriovenous malformations: analysis of 1012 treated patients. Journal of Neurosurgery. 2013, y. 4, no. 119, p. 981-987, ISSN 0022-3085. DOI: 10.3171/2013.5.jns1311.
- ↑ POLLOCK, Bruce E. – FLICKINGER, John C.. A proposed radiosurgery-based grading system for arteriovenous malformations. Journal of Neurosurgery. 2002, y. 1, no. 96, p. 79-85, ISSN 0022-3085. DOI: 10.3171/jns.2002.96.1.0079.
- ↑ FELICIANO, Caleb E – DE LEÓN-BERRA, Ramón – HERNÁNDEZ-GAITÁN, Manuel S. , et al. A proposal for a new arteriovenous malformation grading scale for neuroendovascular procedures and literature review. P R Health Sci J [online]. 2010, vol. 29, no. 2, p. 117-20, Available from <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3101505/?tool=pubmed>. ISSN 0738-0658.
- ↑ LEVY, EladI – DUMONT, TravisM – KAN, Peter. A proposed grading system for endovascular treatment of cerebral arteriovenous malformations: Buffalo score. Surgical Neurology International. 2015, y. 1, no. 6, p. 3, ISSN 2152-7806. DOI: 10.4103/2152-7806.148847.
- ↑ BERMAN, Mitchell F. – SCIACCA, Robert R. – PILE-SPELLMAN, John. The Epidemiology of Brain Arteriovenous Malformations. Neurosurgery. 2000, y. 2, no. 47, p. 389-397, ISSN 0148-396X. DOI: 10.1097/00006123-200008000-00023.
- ↑ MINAMI, S – SAGOH, T – NISHIMURA, K. Spinal arteriovenous malformation: MR imaging.. Radiology. 1988, y. 1, no. 169, p. 109-115, ISSN 0033-8419. DOI: 10.1148/radiology.169.1.3420244.
- ↑ HARTMANN, Andreas – MAST, Henning – MOHR, J. P. Morbidity of Intracranial Hemorrhage in Patients With Cerebral Arteriovenous Malformation. Stroke. 1998, y. 5, no. 29, p. 931-934, ISSN 0039-2499. DOI: 10.1161/01.str.29.5.931.
- ↑ JHAVERI, Miral. Diagnostic Imaging: Brain. - edition. Elsevier Health Sciences, 2020. 1300 pp. ISBN 9780323756204.
- ↑
- ↑
- ↑ WILLINSKY, R – LASJAUNIAS, P – TERBRUGGE, K. , et al. Brain arteriovenous malformations: analysis of the angio-architecture in relationship to hemorrhage (based on 152 patients explored and/or treated at the hopital de Bicêtre between 1981 and 1986). J Neuroradiol [online]. 1988, y. 3, no. 15, p. 225-37, Available from <https://www.ncbi.nlm.nih.gov/pubmed/3246600>. ISSN 0150-9861.
- ↑ SMITH, Frank. Neurology and Neurosurgery : Basic Principles. - edition. University Rochester Press, 2002. 528 pp. ISBN 9781580460842.
- ↑ a b VAN BEIJNUM, Janneke – VAN DER WORP, H. Bart – BUIS, Dennis R.. Treatment of Brain Arteriovenous Malformations. JAMA. 2011, y. 18, no. 306, p. 2011, ISSN 0098-7484. DOI: 10.1001/jama.2011.1632.