Nuclear magnetic resonance
Introduction[edit | edit source]
Magnetic resonance imaging (MRI) uses a physical phenomenon called nuclear magnetic resonance (NMR), which has been described in the literature since 1940 (Bloch 1940, Purcell 1946, both 1952 Nobel Prize in Physics). From the beginning, applications appeared mainly in chemistry using MR spectroscopy (MRS). NMR imaging appears after 1970, and for better public acceptance, the word nuclear (or nuclear) has been deleted from the title and MRI has been adopted.
The image is created by non-trivial processing of measured responses to radiofrequency pulses, but because the result depends on unknown parameters, the resulting grayscale in the image cannot be considered as an absolute number (similar to Hounsfield's CT unit), but only relative to grayscale from surrounding tissues. MRI displays soft tissues well. MRI does not use ionizing radiation, so it is considered safer and less stressful than CT.
Magnetic dipole moment[edit | edit source]
The atomic nucleus consists of neutrons and protons that constantly rotate around their own axis in a motion called spin. Protons are positively charged particles, and each moving charged particle creates a magnetic field and exhibits a magnetic moment. The magnetic moment, or magnetic dipole moment, is a vector physical quantity characterizing a magnetic dipole. The magnetic dipole moment is denoted by m and its unit is the ampere square meter A.m2. The magnetic dipole moment is determined by the relation m = IS, where I is the electric current passing through the dipole loop and S is the oriented area bounded by the dipole loop. For a specific basic idea of magnetic moment, consider only an electron. Its magnetic moment can be illustrated in this way: We will consider the simplest atom - a hydrogen atom that is at rest.
In the electrostatic field of a positively charged nucleus, a negatively charged electron will move along closed trajectories (orbits). The electron is electrically charged and therefore forms a current loop equivalent to a magnetic dipole when considered to move along a closed trajectory. This creates a magnetic field that is very weak, but will still interacts with the electron. This way, the magnetic moment of the electron can be intuitively understood. For other objects (protons, nuclei, atoms), the basic idea of the interpretation of a magnetic moment is similar.
The quantity is called the magnetic moment. If we compare this concept with mechanics, we must necessarily conclude that this quantity will describe a rotating object. Given that there is a quantity of spin, which is also related to rotation in the basic approximation, we can conclude that the magnetic moment (of an electron, nucleus, atom) is also related to spin (of the electron, nucleus, atom).
Atomic nuclei with an even nucleon number do not behinteract magnetically with their surroundings (they do not have spin), because their magnetic moments are canceled out and cannot be used for MR imaging. Atomic nuclei with an odd nucleon number retain their magnetic moment. A common and well-known representative of this group is the hydrogen atom 1H, which has one proton and a relatively large magnetic moment. There is more than 60% of water in the body and 1H is therefore the most suitable object for MR imaging. Other representatives are 13C, 19F, 23Na, 31P.
Atomic nucleus in a magnetic field[edit | edit source]
If we insert the nucleus into a strong magnetic field, the rotational axes of the protons are arranged parallel to the lines of force of the external magnetic field. A larger number of them are in a position where their magnetic moment is oriented in agreement (in parallel) with the vector of the external magnetic field and a smaller number of protons are oriented in the opposite way (by 180 °, antiparallel). The antiparallel arrangement of protons is more energy-intensive and therefore less than half of them is oriented in this direction.
NMR principle[edit | edit source]
The principle of NMR is that if the rotating core is placed in a constant magnetic field B0, the magnetic moments (axes of rotation) are compared with the external magnetic field and the axis of the core will rotate slightly around the direction of the applied field B0. This movement occurs with each change in the applied magnetic field, until the core stabilizes in a given position. If the external field ceases to act, the core returns to its original rest position. If a second perpendicular (transverse) BT field is added, the nucleus will start rotating again. To keep the nuclei in constant motion, a high-frequency magnetic field is used, which simultaneously rotates in the XY plane. By choosing the size of the first static magnetic field B0 and choosing the size for the transverse magnetic field BT, it is possible to determine very precisely which nuclei will resonate. By resonance, the magnetic moment m of the nucleus is tilted by 90° into the XY plane and the axis then rotates according to the transverse field. If the transverse field is disconnected, the nucleus still rotates in the XY plane. By bringing a coil close to the rotating magnetic moment, a voltage is induced in it, which is then measured. Simply put, the magnitude of the measured tension depends on the position and type of tissue.
Larmor frequency[edit | edit source]
As already mentioned, protons perform a rotational motion around their axis, or spin. This creates a magnetic field in their surroundings and exhibits a magnetic moment. In addition, protons placed in a magnetic field also show precessional motion. This can be imagined as a movement on the mantle of an imaginary cone (an even more illustrative example can be the movement of a spinning top). The frequency of this movement is called the Larmor frequency. It depends on two factors:
- the intensity of the external magnetic field
- the type of atomic nucleus, expressed by the gyromagnetic ratio (a constant dependent only on the properties of the nucleus).
Example[edit | edit source]
For hydrogen 1H, the gyromatic ratio is = 42.58MHz / T (269.2T-1), ie. in the field B0 = 1.5T the hydrogen nuclei will have a precession motion frequency f0 = about 64MHz.
Resonance[edit | edit source]
On the one hand, the direction of the magnetic moment of each individual preceded proton changes over time, on the other hand, the protons move in different phases, ie they are tilted in different directions in a given time. This interrupts their effect on the total vector of magnetization of the tissue in a plane perpendicular to the direction of the magnetic field. The vector of the resulting tissue magnetization thus has a direction identical to the direction of the lines of force of the outer magnet and cannot be measured in this state. We can say that it is in eclipse by the external magnetic field.
In order to be able to measure the resonant frequency of protons, ie their spectrum, it is necessary to deviate the total magnetization vector from its equilibrium position and thus achieve the formation of a transverse tissue magnetization vector. As mentioned above, the size of the transverse vector is zero due to the chaotic motion of the particles. Changes can be achieved by supplying energy in the form of an electromagnetic pulse. In order for the electromagnetic waves to be absorbed by protons, it is necessary that the Larmor frequency of the particles be equal to the frequency of the transmitted pulse.
If this is the case, there is a magnetic resonance phenomenon, which has several consequences:
- protons begin to perform their precessional motion in phase,
- the difference between parallel and antiparallel (more energy-intensive) protons is reduced and thus the vector of longitudinal magnetization is reduced.
The result is the already mentioned transverse magnetization vector.
"The situation is aptly compared to a cruise ship with many passengers on board: as long as the passengers are distributed and randomly and fairly evenly on board, the ship sails straight. However, as soon as the passengers gather together and begin to walk around the deck railing, the ship will periodically tilt gradually in all directions. "
Relaxation times T1 and T2[edit | edit source]
After the end of the electromagnetic pulse, the protons are no longer supplied with energy and therefore return to their original, more energy-efficient, parallel position and their synchronous motion disappears. This process is called relaxation.
There is a gradual increase in the longitudinal magnetization vector, and the time taken for this vector to recover to 63% is called T1 (longitudinal relaxation, or spin-lattice relaxation). At the same time, however, the transverse magnetization vector is lost by the disappearance of the synchronous motion of the protons, which is a consequence of the interaction of the magnetic fields of the individual particles. The time taken for the transverse magnetization vector to fall to 37% of its value is called T2 (transverse relaxation, or spin-spin relaxation).
In absolute terms, relaxation times T1 are 2-10 times longer than relaxation times T2. In biological tissue, T1 values range from 300–2000 ms, T2 30–150 ms. In practice, the decrease in the transverse component of tissue magnetization is influenced by even small changes in the inhomogeneity of the external magnetic field. The decline is thus much steeper.
Types of electromagnetic pulses used for MR[edit | edit source]
90 ° pulse - rotating the vector of tissue magnetization by 90 ° and the transverse vector is created. The time between pulses is called TR (time to repeat). The time TR between the individual pulses is shortened so that the tissues do not have time to regain the full value of the longitudinal magnetization vector. The received signal from the tissue then differs in how large the vector of their tissue magnetization is at the time of sending the new pulse.
the combination of 90 ° and 180 ° pulse - 90 ° causes an increase in the transverse magnetization vector and after its end the vector starts to decrease again. However, at the time denoted TE / 2, a 180 ° pulse is sent, which changes the orientation of the precessional motion of the protons by 180 °, and the originally faster preceded protons are slower behind the protons preceded and the decreasing transverse vector begins to increase. Over the next TE / 2 period, the proton motion is synchronized, resulting in re-maximization of the signal. After adding the TE / 2 times, we get the TE time - the echo time.
Magnetic fields[edit | edit source]
The external magnetic field of the MR magnet is homogeneous. Magnets used in medicine usually create fields in the range of 0.1–3 T. However, for research purposes, fields up to 9.4 T are also used, for animals up to 21 T. However, a single magnetic field does not allow us to get a spatial idea of individual protons. and create a patient scan with it. However, in order to be able to distinguish signals from different layers of the body, it is necessary that protons at different points reacted when struck by electromagnetic waves of the appropriate frequency reacted.
Spatial resolution and MRI image reconstruction
Therefore, additional fields are added to the homogeneous field of the main magnet. The field, the intensity of which increases with the axis of the body, creates a so-called magnetic gradient. The magnetic gradient with the longitudinal axis allows us to select the plane of the cut, and is therefore called the "slice selecting gradient". In practice, for example, a 0.45 T field (corresponding to f = 19.160 MHz) acts on the feet, while 0.55 T (f = 23.417 MHz) acts on the head. By sending the appropriate frequency, we select only the section we want.
For a section of the aortic arch, for example, the pulse will have a frequency of 22.566 MHz. We can regulate the thickness of the cut in two ways:
- different pulse frequency range, ie the larger the pulse range, the wider the cut and vice versa,
- the slope of the gradient, in other words the extent of the field in which the body is located. Here it is true that the steeper the gradient (the greater the difference between the field strength at the feet and the head), the narrower the section we get
Since one coordinate is not enough for spatial determination, another field is added. This time, however, the field is perpendicular to the long axis of the body, and the force therefore changes in the right-left direction. As a result, protons placed in different "columns" of the body will emit different frequencies. This gradient is called "frequency encoding gradient" or "readout gradient". The final determination of a point in space will provide a third gradient, which, however, works somewhat differently. It is again in the direction of the columns as a readout gradient, but it is only switched on for a very short time before the readout gradient itself is applied. This will affect the precession frequency of the individual protons in the column, but with respect to distance; thus, those that have been affected by the higher intensity field will have a higher frequency than the rest. Once this gradient disappears, the Larmor frequency of the protons in the column will be the same again, but they will no longer oscillate in a common phase, but in different ways depending on how much they were affected by the gradient. This gradient is therefore called the "phase encoding gradient". The procedure of individual phases in one spin-echo frequency is shown in the figure. After the echoes of the frequencies of the individual points in the section are obtained, a final image can be created from the k-space using the Fourier 2D transformation.
Unfortunately, even the knowledge of how to arrange the reaction of exactly the desired protons does not yet make it possible to obtain a scan that would correspond exactly to the ideas of the examining physician. All pulses that are applied must not only be applied, but must be applied at the right time. Based on the knowledge of the function of T1, T2, TR and TE times, it is possible to obtain a large number of different images. There are countless investigative methods that consist of a predetermined order of functions, but they are always based on three images:
- the PD image is named after the abbreviation Proton Density.
- the second image is called T1-weighted and is determined by the T1 time of the individual tissues,
- the last T2-weighted, as the name suggests, is determined by the T-2 tissue time.
Examples
For fields with a strength of 3T, for example, the values T1, T2 apply:
Gray matter: 1200 ms, 80 ms.
White matter: 800 ms, 70ms.
Cerebrospinal fluid: 4000 ms, 600 ms.
Arterial blood: 1700 ms, 120 ms.
Venous blood: 1500 ms, 40 ms.
MRI imaging[edit | edit source]
MRI can be achieved in two ways:
- We can work with an external magnetic field of constant magnetic induction B and look for the energy (frequency) of electromagnetic waves capable of inducing nuclear resonance.
- We can work with a constant energy (frequency) of electromagnetic waves and look for a value of magnetic induction B at which we achieve resonance - in this case we change the value of the Larmon precession
If the examined part of the body is located in a homogeneous magnetic field, then a radiofrequency pulse of appropriate energy will cause the generation of an NMR signal in the entire volume of the examined part of the body and information about local resonance values is lost. However, in an inhomogeneous magnetic field, we can create a certain gradient of magnetic induction B in a certain direction (for example in the direction of the body axis), thus obtaining a state in which the resonance condition is met only in a narrow section of the body perpendicular to the gradient direction.
These gradients are set in different pulse modes and are different for different MR variants as well as for different types of devices and special applications. In this way we can obtain spatially specific information about the magnitude of the resonant signal, which is proportional to the number of resonant nuclei in a given place in space, so using the Fourier transform we are able to obtain total spatial information about the distribution of resonant nuclei. The resolution capabilities of MRI depend on their design, when using superconducting magnets in a liquid helium environment, we are able to identify the structures of substances present in the area based on chemical shifts, but the operation of these devices is very expensive.
A great advantage of MRI over CT is that we are able to obtain sections in different planes - we are not limited to a cross section, but we can also get a sagittal or frontal section by setting the appropriate gradient of magnetic induction B, thus guaranteeing a certain non-invasiveness for cell tissue. MRI is also supported by the fact that no effects of exposure to strong magnets or radiofrequency pulses on biological tissue have been observed so far, so this method is also suitable for use in children and, if necessary, in pregnant women after the first trimester.
Benefits[edit | edit source]
Imaging accuracy - based on different soft tissue signal intensities (brain, heart, cartilaginous tissue ...)
It allows you to distinguish pathological conditions that are otherwise invisible
Non-invasive method - does not use harmful ionizing radiation (also suitable for pregnant and newborns)
Information on blood circulation, blood vessels
Some angiographic images can be displayed without the need to supply a contrast agent
Functional MRI allows the display of both active parts of the brain during individual activities
Contrast agents[edit | edit source]
They are used to improve the image - they make visible structures that are not distinguishable in the native image. The principle of their function is to facilitate the relaxation of protons, which shortens the relaxation time T1 and T2. Shortening the relaxation time T1 leads to an intensification of the T1 weighted image, on the contrary, to T2 it leads to its attenuation. Contrast agents can be divided into paramagnetic and superparamagnetic agents.
Paramagnetic substances amplify the magnetic field, which shortens the relaxation time of the environment. They often contain gadolinium, which is highly toxic to humans, so it is bound in the form of chelated complexes. They are widely used, often used in CNS examinations, because they can penetrate the damaged blood-brain barrier. These include Magnevist (gadopentetic acid), Omniscan (gadodiamide), Dotar (Gd-DOTA, gadoteric acid) and Mn-DPDP (mangafodipir, used to test the liver). Superparamagnetic substances are solids that are introduced into the body in the form of suspensions, they are extremely effective. Examples are SPIO (superparamagnetic iron oxide) and USPIO (ultrasmall superparamagnetic iron oxide).
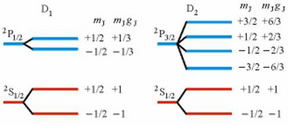
Zeeman effect[edit | edit source]
It is a split of the spectral lines of an atom which is affected by an external magnetic field. It is named after the Dutch physicist Pieter Zeeman. In 1897, he was the first to observe the splitting of a spectral line into a triplet in a weak magnetic field, which is referred to as the normal Zeeman effect. In most cases, however, there is a splitting into more lines, the so-called anomalous Zeeman effect.
The energy levels of atoms in an external magnetic field are, in addition to the dependence on the principal quantum number, also dependent on the orbital and magnetic quantum number, as well as on the magnetic induction of the B field.
Consider a hydrogen atom without hyperfine structures. The quantum number mj takes 2j + 1 possible values. In an external magnetic field, these states will have different energies due to the different orientation of the magnetic dipoles in the magnetic field. It follows that each energy level decays into 2j + 1 equally spaced levels, which are symmetrically distributed around the original level. Line splitting is greater for stronger fields.
Special MRI applications[edit | edit source]
Diffuse MRI[edit | edit source]
Diffuse MRI shows signal changes caused by the diffusion of water molecules in tissues. Such an image is relatively independent of the relaxation times T1, T2 and the density of the proton nuclei (PD). Diffuse imaging is used mainly in the evaluation of pathological conditions of the brain (age of ischemic brain injury, traumatic changes in the brain, assessment of the cell composition of brain tumors or changes due to Alzheimer's disease, autism, schizophrenia, etc.). The direction of diffusion can be completely random in all directions (eg in cerebrospinal fluid or gray matter of the brain) or limited to only some directions (eg in the white matter of the brain diffusion predominates in the direction of long axonal fibers), where omnidirectional diffusion is prevented by walls. The direction of diffusion can be determined by scanning the selected tissue layer multiple times in several directions. The individual directions of the image are obtained by changing the orientation of the magnetic gradients. Each gradient direction then shows a different diffusion direction. In practice, the direction of diffusion is calculated from at least 6 directions, but usually from 12 to 256 directions. The result of diffusion imaging can be a gray scale map of diffusion size (DWI method - Diffusion Weighted Imaging) or a color map of the brain (DTI method - Diffusion Tensor Imaging), where individual colors determine the individual directions of diffusion in a given area.
DWI method - Diffusion Weighted Imaging
In DWI, the intensity of each element of the image (voxel) reflects the diffusion rates of water in the area. since water movements are highly dependent on thermal conditions and the cellular environment itself, we should be able to observe changes in a given tissue thanks to DWI and therefore to observe early changes indicating pathological conditions. To illustrate, DWI is more sensitive to the early pathological changes accompanying stroke than traditional MRI. DWI is most suitable for the description of tissues in which the isotropic movement of water dominates, ie gray matter in the cerebral cortex, large brain nuclei or in the body, where the rate of water diffusion appears to be approximately the same in all directions.
DTI Method - Diffusion Tensor Imaging
Diffuse tensor imaging (DTI) is a magnetic resonance technique that allows you to measure the limited diffusion of water in tissues. It also provides useful information on the structure of various tissues, such as muscle (and heart) or prostate tissues.
In DTI, each voxel has one or more parameters: the diffusion rate and the preferred diffusion direction. The properties of each voxel are usually calculated thanks to the respective vectors or tensors, respectively, from at least 6 directions. In some methods, hundreds of images are put together and the resulting image is generated. Thanks to the larger volume of information obtained during DTI, this is a very sensitive method that allows us to observe even very subtle pathologies. In addition, we can use the obtained directional information
MR angiography (MRA)[edit | edit source]
The displayed parameter in the MRI can be, in addition to the core density and relaxation times T1 and T2, also the flow of excited nuclei. Nucleus movement is then used by MR angiography (MRA), a method showing the flow of blood through blood vessels or the flow of cerebrospinal fluid. To display the flow of nuclei in MR angiography it is possible to use :
MRA using contrast agents
- CE MRA (Contrast Enhanced)
MRA without contrast agents
- TOF MRA (Time of Flight)
- PC MRA (Phase Contrast)
- MRA using contrast agents
The CE MRA technique uses contrast agents to visualize the flow of nuclei. The method can distinguish the arterial phase (filling the arteries with blood) from the venous phase (filling the veins with blood). First, a comparative image is taken without contrast, then an image at the moment when the contrast agent is present in the arteries and finally image is taken after the transfer of contrast agent into the venous system. The MRA image is calculated as the difference between the non-contrast image and the contrast images in the arteries / veins. Contrast agents based on metal compounds are used.
MRA without contrast agents
Contrast-free MRA methods are based on changes in the phase of the precessional motion of particles and the size of the magnetization vector in the presence of a gradient magnetic field. The phase change ΔΦ precession is proportional to the velocity of the particles in, the square of the duration tG of the gradient field and the size of the gradient field G:
ΔΦ=vt2G
Phase changes in the MRA image are then manifested either by a loss of signal (decrease in brightness) or a gain in signal (increase in brightness). They therefore manifest themselves similarly to contrast agents. Signal loss is used by the PC MRA (Phase Contrast) method, signal gain is used by the TOF MRA (Time Of Flight) method.
Phase Contrast MRA[edit | edit source]
If the excited area is excited by an RF pulse, then the excited particles of stationary tissues provide a strong signal upon detection. However, the excited blood flow particles leave the scanned scene before the signal is recorded and do not appear in the image. Signal loss is typical only for high flow rates, no signal loss at low speeds. However, the disappearance of the signal can also occur during the phasing out of the precessional motion of the particles, eg during turbulent flow (opposite phases cancel each other out), which occurs at high flow velocities. The resulting MRA image is calculated from the differences between the images taken before and after the application of the magnetic gradient.
Functional MR[edit | edit source]
Functional magnetic resonance (fMR), along with the progressive development of statistical methods and computer technology, is developing as a means of visualizing the anatomical structures of the brain involved in the mechanisms of perception, motor control, and thinking. It therefore serves to functionally represent brain activity. The essence of the method is a change in blood flow and blood volume in the active area of the cerebral cortex (perfusion fMRI) and, unlike standard magnetic resonance imaging, it has the ability to detect dynamic signal changes caused by local fluctuations in oxyhemoglobin to deoxyhemoglobin ratio dependent on neuronal activity (BOLD - Blood Oxygenation Level Dependent). The non-oxygenated form of hemoglobin has paramagnetic properties and acts as a natural MR contrast agent, and thus in places with its higher concentration, magnetic inhomogeneities occur, due to the faster loss of energy of excited protons and thus greater local loss of radiofrequency signal. The active area of the brain, which consumes more oxygen, then provides a stronger signal than the surroundings.
During fMRI examinations with repeated scanning, images of the entire volume of the brain are acquired at rest, even during the active solution of tasks (response to a stimulus, movement of limbs, word formation, etc.). Changes in brain activity are measured from the difference between pairs of images taken at rest and during brain activity.
The Echo Planar Imagining (EPI) method is used for detection. This makes it possible to record the signal from the entire section (volume) after one or several radio frequency pulses by means of rapid changes in the magnetic field. The obtained signal is then divided into a finite number of samples, which have information about the signal from each section.
Functional magnetic resonance imaging allows you to specify diagnostics of some neurological and psychiatric diseases and provides options for planning surgical procedures.
Instrumentation[edit | edit source]
The patient is placed in the gantry (tunnel) of the MR device and there is exposed to a strong homogeneous magnetic field of the MR magnet (in the range of 0.5–3T). In order to be able to distinguish signals from different layers of tissues, another magnetic field formed by so-called gradient coils is added. Surface coils ("organ coils") are used to examine individual parts of the body. These coils are used to receive a signal in the immediate vicinity of the examined area, so the resulting signal is stronger (head, cervical spine, shoulder coils, etc.) and the image quality is higher.
fMRI is an examination that requires the cooperation of patients. The correct execution of the assigned task is a crucial point in the entire investigation chain. For some cognitive tasks (eg verbal fluency test), it is impossible to directly objectify the patient's performance when scanning fMRI data to verify that he was performing the task as assigned.
The examination is controlled by a computer and the provided image data are then processed by image analysis programs. Preprocessing, statistical analysis and evaluation of results usually take place outside the MR workplace itself. It is necessary that the workplace is shielded so that there is no interference from the transmission frequencies of radio waves. The walls of the examination room are insulated with a Faraday cage.
MR spectroscopy[edit | edit source]
Nuclear magnetic resonance spectroscopy, more commonly known as MR spectroscopy, is a research technique that uses the magnetic properties of some atomic nuclei to determine the physical and chemical properties of the atoms or molecules in which these nuclei are contained. MR spectroscopy is based on the principle of nuclear magnetic resonance and provides detailed information on the structure, dynamics, reaction state and chemical environment of molecules. The intramolecular magnetic field around the atom in the molecule changes the resonant frequency and thus provides access to detailed information about the electronic structure of the molecule.
MR spectroscopy enables non-invasive monitoring of biochemical processes in various organs under both normal and pathological conditions. MR spectroscopy is one of the few techniques that allows the determination of metabolites in tissues in vivo, and is therefore sometimes referred to as in vivo MR biopsy.
Types of MR spectroscopy[edit | edit source]
Proton 1H MR[edit | edit source]
Proton 1H MR spectroscopy can provide information on the proportion and concentration of some hydrogen-containing compounds. The coil is focused on the frequency band in which hydrogen in various compounds (63MHz) resonates - N-acetyl aspartate NAA, creatine, choline, myoinositol, lactate, glutamate, aspartate, GABA. This method is mainly used in monitoring the metabolism of brain tissue.
Phosphorus 31P spectroscopy[edit | edit source]
In phosphorus 31P spectroscopy, we obtain information on the relative proportion of metabolites containing phosphorus, which is present mainly in macroergic phosphates (phosphomonoesters PME, phosphodiesters PDE, ATP, ADP, phosphocreatine, inorganic phosphate (Pi)). Phosphor spectroscopy (31P MRS) is suitable for describing the energy metabolism of a tissue or organ. It is most often used to examine patients with metabolic muscle disease. In recent years, changes in the energy metabolism of the liver have been monitored by phosphorus spectroscopy.
Use[edit | edit source]
MR spectroscopy is mostly used in chemistry and biochemistry to study the properties of organic molecules. The method allows non-invasive, in vivo measurement of the concentration of a number of chemical compounds in the CNS. It also serves to evaluate various biological processes - membrane and energy metabolism, concentrations of excitatory and inhibitory neurotransmitters. Data obtained by MR spectroscopy can provide new insights into the causes, diagnosis and therapy of many neuropsychiatric diseases.
Links[edit | edit source]
Resources[edit | edit source]
- NAVRÁTIL, Leoš a Jozef ROSINA, et al. Medicínská biofyzika. 1. vydání. Praha : Grada, 2005. 524 s. ISBN 80-247-1152-4.
- ŽIŽKA, Jan a Vlastimil VÁLEK, et al. Moderní diagnostické metody. III. díl, Magnetická rezonance. 1. vydání. Brno : Institut pro další vzdělávání pracovníků ve zdravotnictví, 1996. ISBN 80-7013-225-6.
- CHLEBUS, P, M MIKL a M BRÁZDIL. Funkční magnetická rezonance – úvod do problematiky. Neurologie pro praxi [online]. 2005, roč. 6, vol. 3, s. 133-138, dostupné také z <http://fmri.mchmi.com/articles/chlebus_prehled.pdf>. ISSN 1213-1814.
- SEDLÁŘ, Martin, Erik STAFFA a Vojtěch MORNSTEIN, et al. Zobrazovací metody využívající neionizující záření [online]. Brno : Biofyzikální ústav Lékařské fakulty Masarykovy univerzity v Brně, 2013, dostupné také z <http://www.med.muni.cz/biofyz/zobrazovacimetody/files/zobrazovaci_metody.pdf>.
- HRAZDIRA, Ivo a Vojtěch MORNSTEIN. Lékařská biofyzika a přístrojová technika. 1. vydání. Brno : Neptun, 2001. 396 s. ISBN 80-902896-1-4.
- ROSINA, Jozef, Jana VRÁNOVÁ a Hana KOLÁŘOVÁ, et al. Biofyzika : Pro zdravotnické a biomedicínské obory. 1. vydání. Praha : Grada, 2013. 0 s. ISBN 978-80-247-4237-3.
Internet resources[edit | edit source]
- Unknown author, MRI, http://fmri.mchmi.com/main_index.php?strana=13
- Unknown author, NMR, https://physics.mff.cuni.cz/vyuka/zfp/txt_410.pdf
- Evžen Amler, Elektřina a magnetismus, https://moodle.mefanet.cz/login/index.php
- Jakub Nezval, NMR, http://artemis.osu.cz/biofyzika/Studium/Studmat/material/NMR.pptx
- Jitka Mazánková, Kontrastní látky a jejich nežádoucí účinky, https://is.muni.cz/th/326352/lf_b/Kontrastni_latky_a_jejich_nezadouci_ucinky.pdf
- Karla Miller, Manus Donahue, Rob Tijssen, Dan Bulte, Jamie Near, MRI Physics Course, FMRIB Centre – Department of Clinical Neurology, University of Oxford, https://www.win.ox.ac.uk//education/graduate-training-course/program/lectures/mri-physics/mri-physics-course
- Miloš Vojtíšek, RF cívka pro MR systém, https://www.vutbr.cz/www_base/zav_prace_soubor_verejne.php?file_id=40375
- Viktor Babjak, Zeemanov jav, https://www.viktorbabjak.cz/domains/viktorbabjak.cz/public/documents/practical/prak4-17-zeemanov-jav.pdf