Preeclampsia
Synonyms: Pregnancy toxicosis, late gestosis, EPH gestosis (Edema, Proteinuria, Hypertension).
The condition can result in a woman's life being threatened - eclampsia, it can be complicated by HELLP syndrome.
It occurs in 10-14% of primiparas, 5-7% of pluriparas. Risk factors for preeclampsia are primiparity, multiple pregnancy, low socio-economic status of the pregnant woman, occurrence of preeclampsia in the family, chronic renal diseases, hypertension, preeclampsia in a previous pregnancy, DM, hydatid mole, obesity and avitaminosis.
| Preeclampsia | |
| Risk factors | obesity, hypertension, DM, nulliparity [1] |
|---|---|
| Classification and references | |
| ICD | O10 − O14 |
| MeSH ID | D011225 |
| OMIM | 189800 |
| MedlinePlus | 000898 |
| Medscape | 1476919 |
Etiology[edit | edit source]
The etiology is unknown, with many theories. One of them is, for example, abnormal trophoblastic invasion, when the trophoblast does not grow into all capillaries. These vessels stiffen, have a high resistance (reminiscent of atherosclerosis), spasm occurs, which reduces blood flow through the placenta (IUGR and fetal hypoxia). This is followed by the development of hypovolemia and hypoperfusion of the uterine area, which is reflected in changes in blood flow through the mother's kidneys and liver. Another theory depends on hemodynamic changes. From the fundus of the uterus(most preeclampsia occurs when the fetus is in the position of the fundus) blood flows mainly through the ovarian veins, which leads to blood stasis in the kidneys (the left ovarian vein opens directly into the renal vein), it is more pronounced in twins and polyhydramnios.
Other possibilities of occurrence depend on immunological defects (vasculitis), genetic predisposition, dietary errors (deficiency of proteins, thiamine, Fe, vitamins, excessive intake of salt, low calcium), the action of oxygen radicals, but also on geographical factors
Pathogenesis[edit | edit source]
The main mechanism is generalized vasoconstriction, which causes the movement of water into the tissues and increases the hematocrit. The organism responds to this state of dehydration hemodynamically by redistributing the volume, which is caused by sympathetic activation. For this reason, the flow through the kidneys decreases, water and salts are retained and edema occurs. Next, a humoral reaction occurs, which includes the activation of the RAAS and changes in the action of prostaglandins, which change the balance between thromboxane and thus lead to preeclampsia. Prostacyclin also lowers blood pressure and prevents platelet aggregation, supports flow through the uterus (vasodilatans), inhibits uterine contractions, thus reducing the incidence of preeclampsia. On the contrary, thromboxane acts as a vasoconstrictor, stimulates platelet aggregation and stimulates the activity of the uterus.
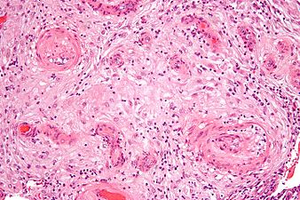
Pathological changes in preeclampsia[edit | edit source]
The most important diagnostic triad: Edema, proteinuria, hypertension. The characteristic lesion is glomerular endotheliosis. The endothelium is swollen, amorphous, the capillary lumen is uneven. Its cause is vasospasm and ischemia. In moderate preeclampsia, glomerular flow decreases by 25%, in severe preeclampsia by 50%. The liver is affected by periportal hemorrhagic necrosis, thrombosis in arterioles and subcapsular hematomas. All these changes are related to generalized vasospasm and impaired coagulation. The most pathological changes are in the placenta (vascular changes on spiral arterioles, placental infarctions).
Laboratory[edit | edit source]
Proteinuria is usually present in the laboratory. It is rated semi-quantitatively as + to +++, usually above 300 mg/day. Furthermore, uric acid, which is created due to an excess of oxygen radicals. Increasing ischemia increases the proportion of the xanthine oxidase enzyme, which also increases urate ( a rise in urate above 320 μmol/l is a marker of preeclampsia). We also measure malondialdehyde (MDA) (a product of lipid peroxidation, a new marker).
Abnormal liver test values are increased when HELLP syndrome is suspected. There is often a rise in hemoglobin and hematocrit. We also evaluate changes in hemocoagulation (aPTT, fibrinogen, prothrombin time – usually normal), FDP rises, thrombin time increases.
Care of women with preeclampsia[edit | edit source]
We hospitalize in the event of an increase in blood pressure above 140/90 or more (measured twice), or if there is an increase compared to the previous control by 30 (systole) or 15 (diastole). Furthermore, with proteinuria over 300 mg/day, rise in liver tests, evidence of thrombocytopenia and IUGR.
It is important to recognize the initial stages of preeclampsia (great weight gain (edema), headaches , visual disturbances, vomiting, pain in the epigastrium). The beginning is sometimes slow, sometimes fast. If all symptoms are not fully developed and there are no indications for hospitalization, we monitor patients on an outpatient basis.
In severe preeclampsia (BP above 160/110, proteinuria above 5 g/day, oliguria , visual disturbances, initial stages of pulmonary edema), we consider termination of pregnancy.
Treatment of impending eclampsia and eclamptic seizure[edit | edit source]
The main principles of therapy include timely treatment of hypertension, ensuring placental perfusion, prevention of spasms, fluid balance, reduction of edema. If it is a very severe, difficult to correct condition, we consider terminating the pregnancy.
Therapy includes strict bed rest, oxygenation with oxygen (oximeter monitoring). We administer magnesium sulfuricum, which promotes the release of prostacyclin from the endothelium, reduces vasoconstriction and platelet aggregation, and dilates CNS vessels (prevention of cerebral ischemia). We use calcium (chloratum or gluconicum) as an antidote. Symptoms of Mg overdose include a decrease in respiratory rate below 15 breaths/min and disappearance of the patellar reflex. Antihypertensives are given when diastole is above 95, the pressure is lowered slowly (there is a risk of fetal hypoxia). The drug of first choice is methyldopa, beta blockers (Vasokardin), calcium channel blockers can also be used(Cordipine). In acute conditions, we administer Dihydralazine-Nepresol (decrease in vascular resistance).
We supplement the treatment with infusion therapy (mannitol, frozen blood plasma, glucose 40%, etc.). Corticosteroids are administered in case of incipient brain edema.
Lasting effects[edit | edit source]
There is emerging evidence of an increased risk of cardiovascular disease and kidney disease in women whose pregnancies have been complicated by preeclampsia. See: L. Greiffeneggová; D. Gross; P. Kaňová Pract. Medicine. 2017; 97(3): 117-122 online For physicians (registration required)
Links[edit | edit source]
Related Articles[edit | edit source]
Literature[edit | edit source]
- BENEŠ, Jiří. Studijní materiály [online]. [cit. 2009]. <http://jirben.wz.cz>.
References[edit | edit source]
- ↑ AL-JAMEIL, Noura – AZIZ KHAN, Farah – FAREED KHAN, Mohammad. , et al. A brief overview of preeclampsia. J Clin Med Res [online]. 2014, y. 6, vol. 1, p. 1-7, Available from <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3881982/?tool=pubmed>. ISSN 1918-3003.