Systemic vasculitides
Vasculitides are a heterogeneous group of diseases that are caused by inflammation of the vascular (mainly arterial) wall - angiitis. Histology, X-ray is essential for the diagnosis. According to the size of the affected vessel, we distinguish vasculitis into:
- aortitis – inflammation of the aorta,
- arteritis – inflammation of medium and small arteries.
- arteriolitis – inflammation of arterioles,
- vasculitis – inflammation of arterioles, capillaries and venules,
- phlebitis – inflammation of the veins.
The consequence of vasculitis is usually the weakening of the vessel wall (in some cases it arches as microaneurysms) with rupture and bleeding (petechiae to purpura – disorders of primary hemostasis), as well as thrombosis superimposed on damage to the intima caused by inflammation, or obliteration of the lumen during repair of inflammation, which lead to ischemia.
Pathogenesis[edit | edit source]
- Unclear etiopathogenesis (primary vasculitides), mostly autoimmune diseases (immunocomplexes), can be one of the following mechanisms:
- immune complexes and the inflammatory reaction triggered by them (type III immunopathological reaction);
- immunopathological reaction IV. type;
- autoantibodies against lysosomal enzymes of neutrophils (ANCA - Anti Neutrophil Cytoplasmatic Antibodies) - stimulate neutrophils to produce oxygen radicals and secrete lysosomal enzymes, which lead to damage to the surrounding tissue - the so-called pauciimmune type of reaction (without immunocomplexes).
- Transfer from the environment (phlegmon, tuberculosis), septic embolus in central pyemia - secondary vasculitis.
Distribution of inflammation of the arteries[edit | edit source]
| allergic vasculitis | |
| polyarteritis nodosa and related diseases | Polyarteritis nodosa, Kawasaki disease, Wegener's granulomatosis, Churg-Strauss syndrome |
| granulomatous (giant cell) inflammations | Temporal arteritis, Takayasu's disease |
| other | Bürger's disease (thrombangiitis obliterans), Aortitis luetica |
Allergic vasculitis[edit | edit source]
Immune-related systemic inflammation of small vessels (arterioles, capillaries, venules) mainly in the skin, but also in other organs (brain, kidneys, GIT, lungs). These include vasculitides in:
- systemic diseases of the connective tissue (systemic lupus erythematosus, rheumatoid arthritis, etc.);
- allergic reactions to bacterial and viral antigens and to some drugs (antibiotics...);
- Henoch-Schönlein purpura - usually affects children and adolescents after an upper respiratory tract infection, affects the skin, kidneys, GIT, joints.
- Pathogenesis
- Immune complexes are deposited in the vessel wall and activate complement. Chemotactic components of complement (C3a, C5a) attract neutrophils, which release lysosomal enzymes. These enzymes subsequently cause necrosis of the vessel wall.
- Microscopic
- Fibrinoid necrosis of the vessel wall with infiltration by neutrophils, disintegration of their nuclei (karyorhexis = leukocytoclasia) resulting in chromatin dust in the vessel lumen of thrombosis. All lesions are at the same stage of development, i.e. the same age, unlike polyarteritis nodosa.
Polyarteritis nodosa (PAN)[edit | edit source]
It is inflammation affecting all layers of the vessel wall (hence polyarteritis) and aneurysms are formed segmentally (hence nodosa). Previously, it was referred to as periarteritis, because the inflammatory infiltrate extends far into the vessel's surroundings.
- Pathogenesis
- The disease arises as a result of the formation of immune complexes that bind to small and medium-sized arteries. The causative antigen is very often the hepatitis B virus). The immunocomplexes then "attack" the arteries of all tissues, especially the kidneys, GIT, heart, skeletal muscles, but miss the lungs. The disease takes place in attacks, that is why we find damage of different ages on the vessels. Among the complications of this disease are the formation of aneurysms and also thrombosis, which can cause a heart attack.
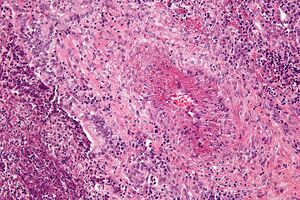
- Microscopic
- Transmural fibrinoid necrosis first with polymorphocellular infiltrate (neutrophils), in later stages round cell infiltrate (mononuclear cells). The infiltrate extends periadventitially. The inflammation heals with the help of ligaments and the lumen of the vessel is often obliterated.
Kawasaki disease[edit | edit source]
"Children's PAN" - mainly affects children under one year of age, in addition to the involvement of blood vessels, it is characterized by skin rashes, inflammation of the conjunctiva and mucous membranes of the oral cavity, enlargement of the lymph nodes (mainly neck) - mucocutaneous and nodal syndrome, it is not very serious, it heals spontaneously, but it is the risk of forming aneurysms of the coronary arteries (rupture) or their thrombosis (heart attack).
Granulomatosis with polyangiitis[edit | edit source]
Wegener's granulomatosis - lungs Previously, Wegener's granulomatosis is apparently an autoimmune vasculitis (95% of patients had ANCA in their serum), which is characterized by a triad:
- necrotizing vasculitis of the PAN type, mainly affecting small vessels in the lungs;
- necrotizing granulomas in the upper respiratory tract;
- necrotizing glomerulonephritis (focal-segmental, sickle-shaped).
Churg-Strauss syndrome[edit | edit source]
Eosinophilic granulomatosis with polyangiitis (EGPA, Churg-Strauss syndrome) is a combination of necrotizing vasculitis, which affects small to medium-sized vessels, and eosinophilic granulomatosis, which mainly affects the respiratory tract and closely resembles Wegener's granulomatosis. The disease is associated with eosinophilia and bronchial asthma, and in 30-40% of cases also with the formation of ANCA antibodies.
Temporal arteritis (Horton's giant cell arteritis)[edit | edit source]
Segmental granulomatous inflammation of larger and medium arteries (mainly branches of a. carotis externa et interna - a. temporalis superficialis, orbital arteries (can lead to blindness), cerebral arteries (can lead to encephalomalacia), mainly affects older women, sometimes associated with polymyalgia rheumatica .
- Macroscopically
- Redness on the temple, palpable pain, the artery can turn into a stiff fibrous band.
- Microscopic
- At the beginning of lymphoplasmocytic infiltration, later the formation of granulomas in the media, the breakdown of the internal elastic membrane and phagocytosis of its fragments by giant multinucleated cells), thrombosis of the lumen, the chronic stage corresponds to reparation - fibrosis of all layers of the wall and the organization of the thrombus leads to the obliteration of the lumen and the transformation of the vessel into a fibrous band.
Takayasu's disease[edit | edit source]
Chronická idiopatická granulomatózní aortitis, postihuje i odstupující velké tepny (bezpulsová nemoc HK, poruchy zraku, neurologické poruchy), někdy plicnici, postihuje především mladé ženy v Japonsku.
- Macroscopically
- Wall thickening, wrinkling and sclerosis of the intima to occlusion of the lumen.
- Microscopic
- Lymphoplasmacytic and granulomatous inflammation of all layers of the wall, destruction of elastic, scarring of the media, fibroproduction in the intima and adventitia, often thrombosis.
Bürger's disease (thrombangiitis obliterans)[edit | edit source]
Bürger's disease Chronic inflammatory disease of the arteries and (deep) veins, especially in the lower limbs (a. tibialis), in the upper limb the a. radialis is most often affected, it affects younger smokers. It starts as inflammation of an artery (arteritis) with thrombosis, the inflammation then spreads to neighboring veins (including superficial veins - phlebitis migrans) and nerves, by reparation of the inflammation and organization of the thrombus, the entire nerve-vascular bundle is built into a fibrous band, the clinical symptoms are caused by the occlusion of the artery – Raynaud's phenomenon (often the first symptom of the disease), claudication, gangrene.
Next[edit | edit source]
Other important vasculitides are:
Links[edit | edit source]
[edit | edit source]
External links[edit | edit source]
Source[edit | edit source]
- PASTOR, Jan. Langenbeck's medical web page [online]. [feeling. 3/11/2010]. < http://langenbeck.webs.com >.
References[edit | edit source]
- ↑ MAHR, Alfred, Frank MOOSIG, and Thomas NEUMANN, et al. Eosinophilic granulomatosis with polyangiitis (Churg-Strauss): evolutions in classification, etiopathogenesis, assessment and management. Curr Opin Rheumatol [online] . 2014, vol. 26, no. 1, pp. 16-23, also available from < https://www.ncbi.nlm.nih.gov/pubmed/24257370 >. ISSN 1040-8711 (print), 1531-6963.
References[edit | edit source]
- KLENER, Pavel, et al. Internal Medicine. 3rd edition. Prague: Galén, 2006. 1158 pp. ISBN 80-7262-430-X .