Schistosomiasis
Schistosomiasis (also bilharziasis, schistosomiasis or schistosomiasis) is a disease caused by the parasitic schistosome tapeworm - Schistosoma haematobium, S. mansoni, S. japonicum. Schistosomes live for up to 35 years and belong to the most medically important genus of flukes. They are small thin worms that have a separate sex. They live only in the fresh waters of the tropics and subtropics, in which their typical carriers - snails. More than 200,000 people die from the disease each year and it is the leading cause of pulmonary hypertension worldwide.
Forms:
- Intestinal: S. mansoni, S. japonicum, S. mekongi.
- Urine: S. haematobium.
- Rectal: S. intercalatum.
Occurence[edit | edit source]
Schistosomes occur mainly in the tropics and subtropics, only in the fresh water where their intermediate hosts live. Worldwide, 200 million people are infected, with 85% of infections in sub-Saharan Africa, of which 20% are pregnant women.
- S. mansoni: Africa, SE America.
- S. haematobium: Africa, Middle East.
- S. intercalatum: Africa.
- S. japonicum: China, Philippines, occasionally Japan and Indonesia.
- S. mekongi: SE Asia.
![]() Risk site of infection: Lake Malawi, where there is more than a 75% chance of infection.
Risk site of infection: Lake Malawi, where there is more than a 75% chance of infection.
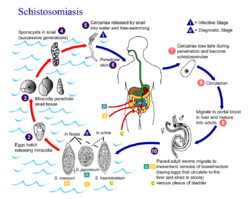
Life cycle[edit | edit source]
The egg enters the water from the host, where the miracidium hatches, which is a floating larva with eyebrows, which actively penetrates into freshwater snails. Individual species of snails are specific to individual species of schistosomes. In snails, it changes into a sporocyst, which multiplies many times. It then turns into cercariae, a forked-tailed larva that leaves the snail. These larvae penetrate the skin or mucous membranes when in contact with humans. In the blood, the cercariae then loses its tail and turns into schistosomulae, which nest in the lungs and continue to grow. In order to mature in adulthood, they must be transported by blood to the portal system. Here the adults come together and move together to their typical location. The female then begins to produce eggs, which either leave the stool or urinate back into the water.
- In the wall of the urogenital tract nests female S. haematobium.
- In the intestinal wall and liver, there are females of S. mansoni, S. japonicum and S. mekongi.
- In the wall of the large intestine and rectum parasites S. intercalatum.
Pathogenesis[edit | edit source]
Susceptibility to infection is not affected by age or gender. The infection is not transmissible from person to person.
- Infectious stage: cercariae that takes minutes to penetrate the skin.
- Pathogenic agents: eggs.
The female parasites in the venous system, where she lays eggs. Eggs produce lytic enzymes for penetration from the veins into the wall of the GIT (mainly intestine) or urogenital tract (mainly bladder), where they accumulate and cause local obstruction. In addition, the eggs circulate to the liver, lungs and other organs (hematogenous spread), and thus the disease enters a chronic phase. Adults are able to live and produce eggs for up to 35 years. On the other hand, eggs have a limited lifespan (1 month), which is why we often find viable and dead eggs in the tissues that calcify.
Antigens and enzymes released from eggs activate the host's immune system. A local inflammatory reaction develops around the eggs, forming granulomas and fibrosis.
![]() In S. haematobium, local reactions can result in dysplastic changes in the epithelium as well as bladder cancer.
In S. haematobium, local reactions can result in dysplastic changes in the epithelium as well as bladder cancer.
Clinical signs[edit | edit source]
Clinical symptoms depend on the intensity of the infection and the stage of the infection. The onset is often asymptomatic, with clinical symptoms developing slowly. The disease has a serious prognosis. Factors affecting the severity of the infection are the duration, the number of mites, the location of the parasites, and the immune status of the individual.
Skin phase[edit | edit source]
- The so-called cercarial dermatitis.
- The rash occurs within 12-48 hours after staying in high-risk waters ("bathing rash").
- The location of the rash is only at the site of skin contact with the cercariae.
- Accompanying symptoms: very intense itching, edema, swollen lymph nodes, fever.
- Symptom disappearance even without therapy within 14 days after infection (for symptom relief: antihistamines).
![]() The skin manifestations caused by the cercariae of avian and human schistosomes cannot be distinguished from each other.
The skin manifestations caused by the cercariae of avian and human schistosomes cannot be distinguished from each other.
Subacute and acute schistosomiasis[edit | edit source]
- The so-called toxic stage.
- It appears 2-16 weeks after infection and manifests as Katayama syndrome (hyperergic reaction):
- fever, fatigue,
- pain in the limbs, head, abdomen,
- diarrhea,
- eosinophilia,
- urticaria,
- skin edema,
- swelling of the liver, spleen and lymph nodes. [3]
Chronic schistosomiasis[edit | edit source]
- The so-called traumatic stage.
- It manifests 3-6 months to several years after infection. It is the result of the accumulation of eggs in the tissues, so it depends on which type of patient it has infected.
- The inflammatory reaction around the eggs can manifest itself as:
- diarrhea (sometimes bloody), hematuria,
- abdominal pain, hepatosplenomegaly,
- anorexia,
- portal hypertension,
- neurological problems - granulomatic reactions around the eggs in the brain and spinal cord (atypical migration of adult moths to the brain has been reported in S. japonicum).
Diagnosis[edit | edit source]
Travel history is important. Schistosomes have a long incubation period, so several years old anamnestic data are important.
- Microscopy: native stool specimen (3 samples), urinary sediment.
- Biopsy: for cercariae dermatitis can be done within 3 days after infection, bladder and bowel biopsy can give a false negative result.
- Serology: ELISA.
- Detection of pathological changes on X-ray, ultrasound, colposcopy of the cervix and vaginal wall.
Therapy[edit | edit source]
- Praziquantel is effective against all types of schistosomes. [3]
- Oxamnichin effective only on S. mansoni. [5]