Replacement of kidney function
There are several methods of replacing kidney function, some of which can be described as relatively permanent solutions and others as temporary. A group of patients can be singled out for whom temporary replacement of kidney function must be provided for some acute condition, or where kidney damage is reversible. The second group consists of patients whose kidneys are irreversibly damaged and need to replace kidney function for life.
Kidney replacement methods include:
- kidney transplant,
- hemodialysis,
- peritoneal dialysis (lavage).
Specific indications are given for each method separately (below). In general, preparing a patient for kidney replacement should begin before kidney failure occurs (no later than stage 4 chronic kidney failure), but often the sooner the better. The choice of which method should be adapted to the patient - his age (IgA nephropathy often affects young people), prognosis. Kidney transplantation appears to be the most advantageous method of replacing kidney function, which can be not only the most effective (return of lost function, patient independence, prolongation of survival...) but also the most economical.
Kidney transplantation[edit | edit source]
Kidney transplantation is indicated in any patient with chronic renal failure. Currently, it is a routine method of kidney function replacement, which should be preferred over others (hemodialysis, peritoneal dialysis), both from a prognostic and economic point of view.
Indication[edit | edit source]
Transplantation should be indicated for a patient who reaches stage 4 of chronic renal insufficiency according to K/DOQI in the progression of renal failure, generally the earlier the better. It would be ideal if the patient did not have to undergo another method of replacing kidney function (hemodialysis) before the transplant.
Diseases that lead to kidney failure:
- glomerulopathy (most often IgA);
- chronic tubular diseases;
- diabetic nephropathy;
- polycystic kidney disease.
In the case of a diagnosis of diabetes mellitus type I in combination with severe (terminal) diabetic nephropathy, the kidneys are transplanted at the same time as the pancreas as a combined pancreas and kidney transplantation, where the benefits of subsequent joint immunosuppressive treatment are used. A previous kidney transplantation (with subsequent immunosuppressive treatment) is also a supporting factor for the decision to perform a pancreas transplantation in a diabetic.
Contraindication[edit | edit source]
- Acute or chronic infection;
- Heart Failure;
- coagulopathy;
- AIDS;
- malignant disease;
- advanced liver or lung diseases.
Donors[edit | edit source]
- Living donors
Most often they are relatives, partners, but it is not a condition. They can also be strangers. The main factor is the voluntariness of the donation and the health of the donor. In order not to endanger the donor by removing one kidney, it is necessary to assess the function of the kidney in the future, if there is no risk of, for example, glomerulonephritis?).
- Deceased (cadaveric) donors
In the Czech Republic, the so-called assumed consent for donation after death applies. If a person does not express during his life that he does not want to donate organs, he is automatically considered a donor. One of the requirements is brain death proven by panangiography (2x within 30 min), then also no damage to kidney function (preserved peripheral circulation required) and cold ischemia for up to 24 hours.
Immunology[edit | edit source]
Compatibility in blood groups (AB0 system) is one of the most important. Transplantation is, however, also possible in case of mismatched blood groups (in the Czech Republic since January 2011). Antibodies in the event of a mismatch must be removed from the recipient's blood, for example by adsorption or plasmapheresis. If there is a match in as many HLA features as possible and there is a low titer of lymphocytotoxic antibodies, the cross-test will be negative. The cross-examination means that we combine the recipient's serum, the donor's lymphocytes and the complement. If the cross-test is positive, the antibodies need to be removed.
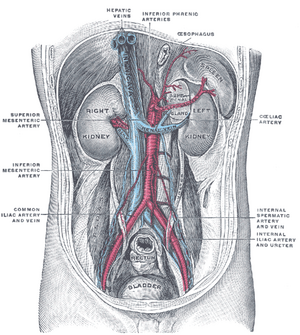
Surgical technique[edit | edit source]
- Kidney removal;
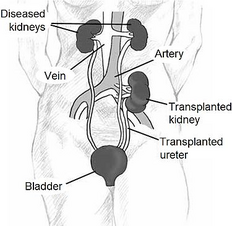
- placement of the graft heterotopically in the right iliac fossa (vessels are connected to the iliac artery and vein, the ureter is sutured to the bladder);
- the original kidneys are usually left in place, where they gradually shrink and atrophy (the exception is polycystic kidneys, which are removed);
- in most cases, only one kidney is transplanted, rarely two (the other to the left iliac fossa), when one would not be enough to restore renal function.
Postoperative development[edit | edit source]
In 65 % of cases, the kidney functions immediately after transplantation. The patient is hydrated to begin urine formation.
In 25 %, there is a delayed development of graft function and the kidney does not function for a short time (days to weeks). After a certain time, the function develops, until then hemodialysis is necessary.
In 10 %, the kidney does not function at all due to thrombosis or unknown causes, for example due to primary afunction.
Statistical data[edit | edit source]
The average waiting time for a kidney is 12 months, which is much less than, for example, in the USA (3-4 years). This is due to the fact that many patients in our country are not indicated for transplantation, even if they could be. Up to 15 % of kidney transplants are repeat transplants. Due to a temporary rejection of the graft, which is not a contraindication to further procedure. One-year survival of patients after transplantation exceeds 95 %. Ten-year graft survival after transplantation is 50 %.
Immunosuppression[edit | edit source]
- Inductive
- ATG – antithymocyte globulin – polyclonal antibodies against T lymphocytes
- basiliximab – monoclonal antibody against the IL-2 receptor on T lymphocytes (anti CD25)
- alemtuzumab (anti-CD52)
- Maintenance - triple combination:
- corticosteroids (prednisone);
- basic immunosuppressants (cyclosporin A or tacrolimus);
- adjuvant immunosuppressants (azathioprine, mycophenolate mofetil).
- Anti-rejection – therapy of acute graft rejection:
- pulse corticosteroid doses of 250–500 mg of prednisone for 3–5 days, if even doses of 2–3 g of prednisone do not take, we consider corticosteroid resistant;
- in corticoresistance to polyclonal antilymphocyte antibodies – ATG or monoclonal basiliximab (anti IL-2R), alemtuzumab (anti CD52).
Cyclosporin A and tacrolimus bind to cycloneurin and inhibit IL-2 expression.
- Possible side effects
Adverse effects include mainly nephrotoxicity and neurotoxicity. Tacrolimus can cause receptor-type DM, so ciclosporin is used instead of tacrolimus in diabetics. Azathioprine is hepatotoxic and myelotoxic. It is therefore recommended to use mycophenolate mofetil instead. Last but not least, it is necessary to mention that other side effects include the threat of developing DM, Cushing's syndrome, osteoporosis, hyperlipidemia due to corticoids.
Complications after transplantation[edit | edit source]
- Early:
- graft rejection (hyperacute, acute) – treatment see above;
- urinary fistula;
- thrombosis of the graft artery or vein;
- opportunistic infections:
- CMV pneumonitis (ganciclovir);
- pneumocystosis (cotrimoxazole);
- legionella (erythromycin).
- Late:
- hypertension (graft artery stenosis);
- chronic liver failure;
- tumors (skin, lymphomas, Grawitz);
- chronic rejection.
Hemodialisis[edit | edit source]
If the kidneys are not able to perform their basic functions (i.e. dialysis, resorption and filtration) even under resting conditions, we speak of kidney failure. Dialysis is a process in which metabolic waste products (e.g. potassium, urea, excess water) retained in the body during kidney failure are removed.
The principle of dialysis[edit | edit source]
Hemodialysis[edit | edit source]
The device that enables this process is known as an artificial kidney. This modern equipment is very technically demanding and high demands are placed on it in terms of efficiency, reliability, safety and ease of use. Hemodialysis is usually performed in a hospital or in special dialysis centers with the help of general nurses, home dialysis is not very common in the Czech Republic, but it can be performed with the assistance of a trained family member. The patient usually undergoes hemodialysis about three times a week for four to six hours. The artificial kidney consists of three basic parts: extracorporeal circulation of the patient's blood, a dialyzer and a circuit ensuring the flow of the dialysis solution.
Extracorporeal circulation of blood[edit | edit source]
This part of the process is carried out by a circuit that pumps the patient's venous blood with the help of rotary pumps through the dialyzer under more or less the same hemodynamic conditions as in the patient's body. Due to the fact that the blood here comes into contact with a surface other than the endothelium of the vessels, there is a risk of the formation of thrombi. Therefore, most patients are heparinized (only patients with bleeding conditions are contraindicated). The circulation also includes sensors that check that there are no air bubbles in the blood that could be a source of embolization.
Dialyzer[edit | edit source]
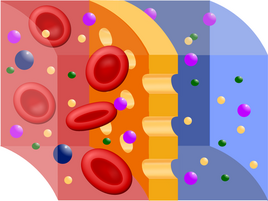
The dialyzer, or capillary, is the main functional unit of the artificial kidney. Dialysis itself (physically, it is a process in which substances of different sizes and solubility are separated from each other) and ultrafiltration of substances and water from the blood into the dialysis solution takes place through a semipermeable membrane (see picture). Membranes of animal origin (e.g. fish bladders, intestines) were used as filters in the first attempts, but now mainly artificial membranes are used, e.g. cellophane, glucose esters or some modern plastic (Cuprophan), which unfortunately can have the ability to stimulate the immune system the patient's system (of course less than the original materials) - therefore the number of dialysis sessions may increase the risk of transplant rejection in the future. The membrane can be arranged in the dialyzer either in the form of sheets or a large number of thin tubes - the goal, of course, is to make the effective surface as large as possible. The membrane thus divides the dialyzer into a blood and dialysate part. On one side of the membrane, blood flows in laminar flow, during which erythrocytes accumulate in the flow axis and the membrane is thus washed more by plasma. The volume flow here is approx. 200-300 ml/min. On the opposite side of the membrane, the dialysis solution flows in the opposite direction in a turbulent flow, the volume flow here is approx. 500 ml/min. In this way, the necessary concentration drop is achieved and thus the rapid diffusion of toxic low molecular weight substances from the patient's blood into the dialysate. Dialyzers are usually single-use, but the same patient can be used multiple times after regeneration, without a decrease in efficiency (disposable capillaries are currently used).
Dialysate circuit[edit | edit source]
This circuit includes both the preparation of the solution and its flow through the dialyzer. The dialysate is prepared by mixing a concentrated sodium bicarbonate solution prepared by the company or in a pharmacy with treated water. It is very important that the dialysis solution contains electrolytes in approximately the same concentration as found in plasma and has the correct pH so that the patient's acid-base balance is not disturbed. At the same time, by adding some ions, especially K+ and Ca 2+, (again using preformed solutions supplied by the company) ion imbalances can be corrected. Glucose can be added to the dialysate, paradoxically in patients who are type 1 diabetics, because they are at risk of hypoglycemia during dialysis (due to the dialysis itself, but also the insulin dosage, which is normal for the patient, but the glucose intake is lower). It is important to control and maintain a constant temperature during the process. Dialysate consumption during 4-6 hour hemodialysis is about 150 liters.
Types of dialysis[edit | edit source]
Acute hemodialysis[edit | edit source]
Acute dialysis is used in sudden conditions where the patient's body is not able to cleanse itself of endogenous or exogenous toxic substances, fluid volume or ions. Indications for acute dialysis include the following conditions:
- acute kidney failure - for example, rapidly progressive glomerulonephritis (RPGN),
- hyperkalemia > 6 mmol/l, which cannot be managed with conservative therapy,
- hypercalcemia > 3.5 mmol/l,
- hyperuricemia > 1000 μmol/l,
- uncorrectable metabolic acidosis, pH < 7.1,
- hyperhydration with heart failure,
- oliguria lasting more than 3 days,
- intoxication with low-molecular substances soluble in water, which after intoxication remain in free form in the bloodstream - e.g. ethylene glycol (fridex - antifreeze), lithium. Other poisons can be eliminated by hemoperfusion, i.e. adsorption on activated carbon, which is carried out by supplementing the hemodialysis machine with a hemoperfusion cartridge (e.g. green toadstool poison, paracetamol, some antidepressants).
Among the generally valid principles of acute dialysis is primarily consideration of whether it is possible to manage some of these conditions with conservative therapy (ion disruptions, disturbances of the internal environment), because dialysis is a method that puts a strain on the organism (cardiovascular, immune system). In acute dialysis, a central venous catheter (CVI) is used as an input. Frequency of dialysis as needed.
Chronic hemodialysis[edit | edit source]
Chronic hemodialysis is used in patients who, usually due to chronic kidney insufficiency, have reached renal failure (stage 5 according to K/DOQI), i.e. a condition where, even when maintaining basal conditions, their body is unable to get rid of excess metabolites, fluid volume and correct internal environment (pH, ions). Patients usually come to dialysis 3 times a week, they undergo dialysis for 4-6 hours. Of the vascular accesses, an arteriovenous shunt between a. radialis and v. cephalica is preferred: If it is contraindicated (heart failure), a central venous catheter is used in the jugular vein. This treatment is for life or until a kidney transplant.
Indications for dialysis (earlier in diabetics):
- urea > 30 mmol/l,
- creatinine 600–800 μmol/l,
- creatinine clearance < 0.25 ml/s.
Diseases that lead to hemodialysis are:
- diabetic nephropathy,
- hypertensive nephropathy,
- chronic glomerulonephritis,
- rapidly progressive glomerulonephritis (RPGN) – when it reaches irreversible fibrotic changes,
- autosomal dominant polycystic kidney disease.
For patients in whom we expect to start dialysis, we should first of all contact the Transplantation Coordination Center or the IKEM transplant surgery clinic in order to ensure the possibility of a kidney transplant in the shortest possible time. Furthermore, we should treat anemia (with erythropoietin), which most patients with renal failure suffer from, and carry out preventive vaccination against hepatitis B (the development of which is the reason for postponing transplantation and shortening survival time). Acute complications of hemodialysis include hypotension (from sudden loss of circulating fluid volume), convulsions (decrease in Na+, K+, Ca2+), arrhythmia (sudden hypokalemia), and bleeding at the vascular access site (related to heparinization). Chronic complications of hemodialysis include cardiovascular complications (ICH, myocardial infarction, CMP, hypertension, which are more common in dialysis patients than in the general population), infections (hepatitis B and hepatitis C), amyloidosis (beta2-microglobulin).
Complications in chronic dialysis[edit | edit source]
- Heart Failure
- infection
- anemia
Peritoneal dialysis[edit | edit source]
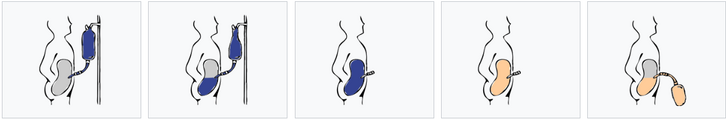
Peritoneal dialysis (PD) is a dialysis method to replace kidney function. PD uses the peritoneum as a membrane through which fluids and solutes (electrolytes, urea, glucose, albumin, osmotically active particles and other small molecules) are exchanged from the blood. Dialysis fluid is fed into the abdominal cavity through a permanently inserted catheter.
Dialysis takes place either every night while you sleep (automatic peritoneal dialysis) or during regular changes during the day (continuous ambulatory peritoneal dialysis). PD is used as an alternative to hemodialysis, although significantly less frequently in many countries (e.g. USA). It is comparably safe, but significantly less expensive in most countries of the world. The main advantage of PD is the possibility to undergo treatment without visiting a medical facility. The most common complication in PD is infection through a permanently inserted catheter in the abdominal cavity.
Performance and types of peritoneal dialysis[edit | edit source]
The fluid enters the abdominal cavity through a peritoneal catheter, which is inserted permanently through the abdominal wall below the level of the navel. The patient can fill and drain the dialysis solution into the abdominal cavity by himself several times a day, up to 4 times during continuous ambulatory peritoneal dialysis (CAPD), when the fluid is usually left in the peritoneal cavity for 6 hours. The used and contaminated dialysis solution is drained out and a new and clean dialysate is infused instead (if the patient dialyzes several times a day).
Automated peritoneal dialysis (APD) using the device limits the number of exchanges to one a day and replaces frequent exchanges at night, the patient connects to the machine before going to sleep, ensuring the exchanges automatically, and his sleep is not affected.
Principle of peritoneal dialysis
Best practices[edit | edit source]
According to the best recommended practice, before starting peritoneal dialysis treatment, it is necessary to evaluate how well the patient understands the PD process itself, to educate them about proper care of the catheter and to complete any missing information. The patient should be continuously monitored to ensure that the dialysis is taking place in the right way and should be regularly examined for possible complications. The patient should also be properly educated about the importance of infection prevention and an appropriate treatment plan should be drawn up with him.
- In preparation for the procedure, the abdominal cavity is cleaned and a catheter is surgically inserted with one end in the abdominal cavity and the other emerging from the skin.
- Before each infusion, the catheter must be cleaned and flow checked in both directions.
- Within about ten to fifteen minutes, 2-3 liters of dialysis fluid (the so-called dialysate) are introduced into the abdominal cavity. Its total volume can reach up to 3 liters and it is possible to add medicines to the liquid just before administration.
- The fluid is left in the abdominal cavity for a certain period of time (the so-called delay), when waste products pass into it from the vascular system through the peritoneum. After this delay (usually 4-6 hours, depending on the treatment), the fluid is pumped out and replaced with fresh. This can happen automatically while you sleep (automated peritoneal dialysis, APD), or during the day, with two liters of dialysate constantly left in the abdominal cavity and exchanged four to six times a day (continuous ambulatory peritoneal dialysis, CAPD).
The fluid usually contains sodium, chloride, lactate or bicarbonate and a high percentage of glucose to provide hyperosmolarity.
The intensity of dialysis depends on the amount of dialysate, the regularity of its exchange and the concentration of the solution. APD has 3–10 exchanges per night, while CAPD has four per day, with dialysate volumes ranging between 2–3 liters and dwell times of 4–8 hours.
The visceral part occupies roughly four-fifths of the total area of the peritoneum, but the parietal peritoneum is more important for PD. The principle of membrane dialysis is explained by two complementary models - the three-pore model (where molecules - proteins, electrolytes or water - pass through the membrane and it "sieves" them depending on the size of the pores) and the distributed model (which emphasizes the role of capillaries and the ability of the solution to increase number of active capillaries participating in PD).
A high concentration of glucose stimulates the osmotic filtration of fluid from the peritoneal capillaries into the abdominal cavity. Glucose passes relatively quickly from the dialysate into the blood (capillaries). After a 4–6 h delay, the osmotic glucose gradient usually drops to too low a level for osmotic filtration to continue. The dialysate is therefore reabsorbed from the abdominal cavity into the capillaries based on the colloid-osmotic pressure of the plasma, which exceeds the colloid-osmotic pressure in the peritoneum by approximately 18–20 mmHg (cf. the Starling mechanism). Lymphatic absorption also contributes to some degree to the reabsorption of fluid from the abdominal cavity into the plasma. In patients with high water permeability (UF coefficient) of the peritoneal membrane, increased reabsorption of fluid from the peritoneum may occur towards the end of the delay.
The ability to exchange small particles and fluids between the peritoneum and the plasma can be classified as high (fast), low (slow), or moderate. Rapid exchange patients have good diffusion (easy exchange of small molecules between blood and dialysate, some improvement in results can be achieved with more frequent, shorter delays as in APD), while slow exchange patients show a higher UF filtration coefficient (due to slower reabsorption of glucose from abdominal cavity, where longer delays with higher fluid volumes show better results), although in practice both types of patients can generally be treated with appropriately adjusted APD or CAPD.
Although there are several different shapes and sizes of catheters that can be used, different catheter insertion sites, number of cuffs, and anchorages, there are no known differences in terms of morbidity, mortality, or rates of infection, but the information is not of sufficient quality to draw definitive conclusions.
Complications[edit | edit source]
The volume of pumped dialysate and the patient's weight are monitored. If more than 500 ml of fluid remains or if 1 liter of fluid is lost during three consecutive treatments, the patient's attending physician is usually notified. Excessive fluid loss can lead to hypovolemic shock or hypotension. Excessive fluid retention can lead to hypertension and edema.
The color of the discharged fluid is also monitored: under normal circumstances it is pinkish in the first four cycles and then clear or pale yellow. The presence of pink or bloody discoloration indicates bleeding into the abdominal cavity, feces indicate intestinal perforation, and turbidity may indicate infection.
The patient may also experience pain or discomfort if the dialysate has an overly acidic reaction, is too cold, or is infused too quickly. Diffuse pain and cloudy discharge may indicate infection. Sharp pain in the anus or perineum may be the result of an incorrectly inserted catheter. Dialysate can also increase pressure on the diaphragm, making breathing difficult, and constipation can limit fluid flow through the catheter.
A potentially fatal complication, estimated to occur in about 2.5% of patients, is encapsulating peritoneal sclerosis, in which bowel obstruction occurs due to a thick layer of fibrin in the peritoneum.
Glucose is the primary osmotic agent in the dialysate, but this can lead to peritonitis, failure of the kidneys and peritoneum as a membrane, and other health complications. Acidity, high concentration and presence of lactate and especially glucose breakdown products in the solution can contribute to such problems. Solutions that have a neutral reaction, use bicarbonate instead of lactate and contain fewer glucose breakdown products, are safer, but there are no studies to confirm this unequivocally yet.
Risks and benefits[edit | edit source]
PD is less effective in removing waste products from the body than hemodialysis, and the presence of a catheter poses a risk of peritonitis by possible introduction of bacteria into the abdominal cavity. There is insufficient evidence on the best treatment for peritonitis associated with PD, although direct intra-abdominal infusions of antibiotics show marginally better results than intravenous administration. There is no clear advantage of other frequently used methods of treatment, e.g. regular peritoneal lavages or the use of urokinase.
Infection of the catheter insertion site may also occur. Prophylaxis using nasal mupirocin can reduce the number of such infections, but it does not affect peritonitis. Infections occur on average once every 15 months (0.8 episodes per patient per year), but in many sites significantly less often – once every 40 or more months compared to hemodialysis allows the PD patient better mobility, occurs to fewer fluctuations in the occurrence of symptoms and phosphates are better removed, but a large amount of albumin is also removed from the body, which requires constant monitoring of the nutritional status.
In most countries of the world, the cost of PD is generally lower than that of HD, the price difference being most pronounced in developed countries.
There has not yet been a large enough study to compare the risks and benefits of CAPD and APD. The independent peer review organization Cochrane compared the results of three smaller clinical trials and found no difference in clinically relevant parameters (ie, morbidity and mortality) in patients with end-stage renal disease, nor an advantage of either method in terms of preserving renal function. The results suggest that APD may have psychosocial benefits in younger patients and those who are employed or studying.
Other complications include hypotension (due to increased fluid exchange and sodium loss), shoulder pain, and hernias or fluid leaks due to increased intra-abdominal pressure. PD can also be used in patients with cardiovascular instability because it does not cause rapid and significant changes in body fluids and in patients with type 1 diabetes because of the impossibility of influencing blood sugar levels through a catheter. Hypertriglyceridemia and obesity are also possible risks due to the large amount of glucose in the dialysis fluid, which can supply the body with 2000-5000 kJ per day.
Of the three connection types and fluid exchange systems (standard, dual-bag, and Y-coupler, the latter two operating with two bags and only one catheter connection, with the Y-coupler set having a single Y-connection between the drain bags, lavage and infusion) dual-bag Y-connector systems show better results in preventing peritonitis than conventional systems.
Extension of the method[edit | edit source]
According to a 2004 worldwide survey, approximately 11 % of end-stage renal disease patients were treated with PD versus the much more common hemodialysis. In Hong Kong and Mexico, PD is more common than the global average – in Mexico it is used in the majority of patients (75 %) – while in Japan and Germany PD use is below the global average.
Improvised dialysis[edit | edit source]
Peritoneal dialysis can be performed impromptu, e.g. in combat conditions or during disasters, using surgical catheters and dialysate made from commonly available infusion solutions, providing temporary replacement of kidney function in patients who have no other option.
Indication[edit | edit source]
This method is advantageous for young patients, who do not have to regularly go to the hospital for hemodialysis, so they can continue their normal activities (work, study). We also use peritoneal dialysis in children and in circulatoryally unstable patients, where we cannot provide permanent and suitable conditions for hemodialysis.
Contraindication[edit | edit source]
Peritoneal dialysis is not indicated in patients with extensive peritoneal adhesions, hernia, colostomy, active bowel disease (Crohn's disease), ascites, or in uncooperative patients.
Complication[edit | edit source]
The most common complication is the development of an infection - usually staphylococcal peritonitis clogged by the catheter (both general and local ATB therapy). Over time, peritoneal dialysis can cause thickening of the peritoneum. This impairs its diffusion function and the patient should be transferred to hemodialysis.
Links[edit | edit source]
Related articles[edit | edit source]
- Chronic kidney disease
- Acute renal failure
- Vascular approaches for dialysis
- Catheter for peritoneal dialysis
- Dialysis amyloidosis
External links[edit | edit source]
- Česká transplantační společnost pacientům - transplantace ledvin
- Koordinační středisko transplantací - transplantace ledvin
Source[edit | edit source]
- PASTOR, Jan. Langenbeck's medical web page [online]. [cit. 24.5.2010]. <http://langenbeck.webs.com>.
References[edit | edit source]
- ČEŠKA, Richard, et al. Interna. 1. vydání. Praha : Triton, 2010. 855 s. s. 558. ISBN 978-80-7387-423-0.
- ↑ ČEŠKA, Richard, et al. Interna. 2. vydání. Praha : Triton, 2015. 909 s. ISBN 978-80-7387-895-5.
- ↑ Wood, M; et al. (2008-08-01). "Nephrology Nursing Standards and Practice Recommendations" (PDF). Canadian Association of Nephrology Nurses and Technologists. Retrieved 2010-09-08.
- ↑ Haralampos V. Harissis et al. A new simplified one port laparoscopic technique of peritoneal dialysis catheter placement with intra-abdominal fixation. The American Journal of Surgery 192 (2006) 125–129 https://www.youtube.com/watch?v=0MuJURb7vpg
- ↑ Skočit nahoru k:a b Best practices: evidence-based nursing procedures. 2007. ISBN 1-58255-532-X.
- ↑ Skočit nahoru k:a b Crowley, LV (2009). An Introduction to Human Disease: Pathology and Pathophysiology Correlations. Jones & Bartlett Publishers. pp. 507–509. ISBN 0-7637-6591-0.
- ↑ McPhee, SJ; Tierney LM; Papadakis MA (2007). Current medical diagnosis and treatment. McGraw-Hill. pp. 934–935. ISBN 0-07-147247-9.
- ↑ Rippe, B, Venturoli, D, Simonsen, O, de Arteaga, J (2004). "Fluid and electrolyte transport across the peritoneal membrane during CAPD according to the three-pore model.". Perit Dial Int 24: 10–27. PMID 15104333.
- ↑ Daugirdas, JT; Blake PG; Ing TS (2006). "Physiology of Peritoneal Dialysis". Handbook of dialysis. Lippincott Williams & Wilkins. p. 323.
- ↑ Strippoli, GFM; Tong A; Johnson DW; Schena FP; Craig JC (2004). Strippoli, Giovanni FM, ed. "Catheter type, placement and insertion techniques for preventing peritonitis in peritoneal dialysis patients". Cochrane Database of Systematic Reviews 4: CD004680.doi:10.1002/14651858.CD004680.pub2. PMID 15495125.
- ↑ Kawanishi, H.; Moriishi, M. (2007). "Encapsulating peritoneal sclerosis: prevention and treatment". Peritoneal dialysis international : journal of the International Society for Peritoneal Dialysis. 27 Suppl 2: S289–S292. PMID 17556321.
- ↑ Perl, J.; Nessim, S. J.; Bargman, J. M. (2011). "The biocompatibility of neutral pH, low-GDP peritoneal dialysis solutions: Benefit at bench, bedside, or both?". Kidney International 79 (8): 814–824. doi:10.1038/ki.2010.515. PMID 21248712.
- ↑ Ballinger, AE; Palmer, SC; Wiggins, KJ; Craig, JC; Johnson, DW; Cross, NB; Strippoli, GFM (26 April 2014). "What is the best treatment to manage peritonitis in people on peritoneal dialysis?". Cochrane Database of Systematic Reviews 4: CD005284.doi:10.1002/14651858.CD005284.pub3. PMID 18254075.
- ↑ Strippoli, GFM; Tong A; Johnson DW; Schena FP; Craig JC (2004). Strippoli, Giovanni FM, ed. "Antimicrobial agents for preventing peritonitis in peritoneal dialysis patients". Cochrane Database of Systematic Reviews 4 (4): CD004679. doi:10.1002/14651858.CD004679.pub2.PMID 15495124.
- ↑ Karopadi, AN; Mason G; Rettore E; Ronco C (2013). Zoccali, Carmine, ed. "Cost of peritoneal dialysis and haemodialysis across the world". Nephrol Dial Transplant 28: 2553–69. doi:10.1093/ndt/gft214. PMID 23737482.
- ↑ Rabindranath, KS; et al. (2007). Rabindranath, Kannaiyan S, ed. "Continuous ambulatory peritoneal dialysis versus automated peritoneal dialysis for end-stage renal disease". Cochrane Database of Systematic Reviews 2 (2): CD006515. doi:10.1002/14651858.CD006515.PMID 17443624.
- ↑ Ehrman, JK; Gordon P; Visich PS; Keteyian SJ (2008). Clinical Exercise Physiology. Human Kinetics. pp. 268–269. ISBN 0-7360-6565-2.
- ↑ Daly, C; Khan, I; Rabindranath, KS; Vale, L; Wallace, SA (13 August 2014). "Y-set and double bag systems offer the most protection against peritonitis during continuous ambulatory peritoneal dialysis (CAPD)". Cochrane Database of Systematic Reviews (8): CD003078.doi:10.1002/14651858.CD003078.pub2. PMID 11406068.
- ↑ Grassmann, A; Gioberge S; Moeller S; Brown G (2005). "ESRD patients in 2004: global overview of patient numbers, treatment modalities and associated trends". Nephrology Dialysis Transplantation 20 (12): 2587–2593. doi:10.1093/ndt/gfi159. PMID 16204281.
Used literature[edit | edit source]
- ČEŠKA, Richard, et al. Interna. 1. edition. Praha : Triton, 2010. 855 pp. ISBN 978-80-7387-423-0.
- BENEŠ, Jiří – STRÁNSKÝ, Pravoslav – VÍTEK, František. Základy lékařské biofyziky. 2. edition. Praha : Karolinum, 2007. 201 pp. ISBN 978-80-246-1386-4.
- HRAZDIRA, Ivo – MORNSTEJN, Vojtěch. Lékařská biofyzika a přístrojová technika. 1. edition. Brno : Neptun, 2001. ISBN 80-902896-1-4.
Categories: Nephrology, Pathology, Internal Medicine, Patophysiology