Primary and secondary vein varicoses
Varicoses are the expansion of superficial veins or veins of the superficial venous system of the lower extremities. It is one of the most common diseases in industrialized countries. It is reported that by the age of fifty, half of the population already has some form of venous insufficiency .
Lower limb varicose veins are classically divided into:
- primary (idiopathic)
- secondary (postthrombotic).
Primary varices[edit | edit source]
A more common type of varicose veins. A certain degree of enlargement of DK veins is seen in half of adult men and 2/3 of women. A more severe degree of the disease occurs in up to 20% of the population.
Degrees of varicose veins[edit | edit source]
- Varicose veins;
- reticular (affecting smaller veins);
- trunk (impairment directly in saphena magna and/or parva).
Pathogenesis[edit | edit source]
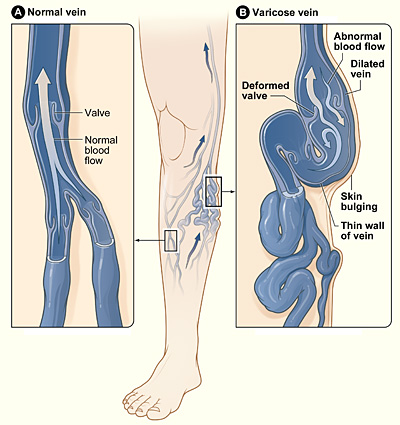
The genetic basis of the congenital weakening of the vein wall and immobility of the venous valves has a great influence. The effect of progesterone is also involved. Another important factor in the pathogenesis is the insufficiency of the valves in the junctions between the deep and superficial systems , which leads to the pushing of blood from the deep to the surface during the action of the muscle pump.
An additional factor for the development can be an increase in intra-abdominal pressure, work while standing or sitting . Congestion occurs in the venous system, resulting in capillary proliferation, increased permeability of the vascular wall and, subsequently, leakage of substances into the interstitium (fibrinogen).
Clinical picture[edit | edit source]
At first, varicose veins are just a cosmetic problem. Later, typical problems occur - a feeling of heaviness or tension in the limbs (especially in the evening, in the heat), night cramps, burning or itching of the skin , pain, a feeling of fatigue and restlessness in the limbs, edema, deposition of pigment (hemosiderin), eczema and even leg ulcers .
The main complications of varices include thrombophlebitis and variceal rupture .
Diagnosis[edit | edit source]
A physical examination will determine the extent of the varicosities. Propagation of the pressure wave induced by tapping on the varices distally indicates valvular insufficiency. By palpation, it is possible to detect enlarged openings in the fascia through which insufficient perforators pass.
Classic tests - Perthes and Trendelenburg - are no longer used, instead diagnostics using ultrasonography .
Therapy[edit | edit source]
Small phlebectasies can be treated with injections of a sclerosing solution followed by a compression bandage. If the entire saphena is relatively healthy and smaller branches are extended, we remove them through small incisions.
A classic procedure for affecting the saphenous trunk - Babcock's operation (stripping). It consists in the careful dissection of the point of entry of the great saphenous vein into the femoral vein in the fossa ovalis in the groin. At this point, we ligate all venous tributaries (v. circumflexa ilium spf., v. epigastrica spf., vv. pudendae ext.) and cross the trunk at the outlet. Then we dissect the saphenous vein in front of the inner ankle and insert the endostripor. We pass the wire through the saphenous vein. At the end, it has an extension on which the entire saphena is inserted when the wire is pulled through the channel.
Both saphenous veins are often used for bypasses, so this operation is indicated judiciously. We always try to ligate insufficient perforators.
Secondary varices[edit | edit source]
Pathogenesis[edit | edit source]
Consequence of deep vein thrombosis. Hypertension in the superficial venous system during deep vein occlusion. Alternatively, as a result of post-thrombotic syndrome – damage to the valves of deep veins during recanalization of thrombosis.
Clinical picture[edit | edit source]
They tend to be smaller and more dispersed. Skin changes, eczema, skin atrophy with pigmentation and leg ulcer develop more quickly. In addition to USG , phlebography is also done to determine the extent.
Therapy[edit | edit source]
Mainly conservative – positioning, bandaging, skin care. In the case of a leg ulcer, it is good to ligate the supply vein and cover the ulcer with skin grafts.
- Closure of the pelvic vein – sapheno-femoral cross-over bypass.
- Femoral vein occlusion – sapheno-popliteal bypass.
Links[edit | edit source]
Related articles[edit | edit source]
Zdroj[edit | edit source]
- BENEŠ, Jiří. Studijní materiály [online]. [cit. 28.6.2010]. <http://jirben.wz.cz>.
- RICHARD, ŠTULC, TOMÁŠ, VLADIMÍR TESAŘ A MILAN LUKÁŠ, Češka. Interna. 3. edition. Praha : Stanislav Juhaňák - Triton, 2020. 964 pp. pp. 239-242. ISBN 978-80-7553-780-5.