Penicillin
Penicilin belongs to the group of beta-lactam antibiotics. Its name is derived from the fungus (Brush, Penicillium), from which they were first obtained. This antibitic was discovered by Alexander Fleming in 1928.
Antimicrobial spectrum[edit | edit source]
Narrow-spectrum penicillins (basic, natural) – effective against G+ bacteria and G− cocci (meningococci, gonococci) [1], oxacillin acts only against Staphylococcus aureus and partly against streptococci,
Broad-spectrum penicillins – effective against both G+ and G−.
Pharmacokinetics and pharmacodynamics[edit | edit source]
After parenteral administration, they are rapidly and completely absorbed. I.V. administration is preferred over i.m. (especially high dises), which is painful. Absorption after oral administration varies with penicillins, depending on the resistance to the acidic environment (pH of gastric juice). To minimize losses due to their adsorption in food, it is recommended to administer at least 1 hour before or after meal. Bioavailability is usually higher than 60 %. Plasma protein binding ranges from 18 % (amoxicilin) to 94 % (oxacilin), but only the unbound fraction is antimicrobially effective.
Penicillins are easily distributed into the eextracellular fluid, due to their low liposolubility they do not penetrate the cells. They penetrate the blood-brain barrier poorly. Inflammatory meningeal changes facilitate their penetration into the CNS.
Most of the absorbed amount is excreted in the urine , by tubular secretion (90 %). This route of excretion may be inhibited by probenecid. 30–50 % of amount of penicillins present in the blood is excreted in breast milk. The biological half-life is short (about 1 hour).
Penicillins have a concentration-independent but time-dependent effect. At least 40 % of the dosing interval time, the antibiotic concentration should be higher than the minimum inhibitory concentration.[1] They have no post-antibiotic effect.
Side effects and toxicity[2][edit | edit source]
Penicillins are very safe drugs. The most common side effect is allegic reactions (I-IV). They occur in approxymately 1-10% of patients. Rarely, an anaphylactic reaction (0,05 %) may occur, which occurs 15-30 minut after administration (most often i.v.). Anaphylaxis usually occurs after previous sensitization. Late allegic manifestations include urticaria, fever, joint pain, skin sfflorescence, angioneurotic edema, interstitial nephritis (autoimunne reactions to the penicillin-protein complex), serum sickness, hemolytic anemia but also very serious complications such as Lyell's or Stevens-Johnson syndrome.
When aminopenicillins are administered to patients with infectious mononucleosis or lymphatic leukemia, a morbiliform rush may occur, which is a toxic reaction, not an allergic one. All penicillins have the ability to cause a cross-reaction, wheter they are contained in food (milk from cows treated for mastitis) or in cosmetics. The allegic reaction to penicillins can be reduced by the administration of glucocorticoids.
Oral administration of oenicillins can lead to dyspeptic problems – nausea, vomiting and diarrhea (especially iwth broad-spectrum penicillins). Diarrhea, even psuedomembranous colitis rarely occurs in broad-spectrum penicillins as a redult of dysmicrobia.
Hoigné syndrome may occur as unusual side effects. It is induced in some patients after the administration of procaine penicillin The clinical picture can quickly disappear, other times the psychological symptoms persist for many months. It retreats spontaneously. The syndrome is not a contraindication to repeated administration of penicillin. Nicolau's syndrome can also arise, as a result of incorrect administration techniques, in this case intraarterially. The symptoms depend on the type of organ affected.
The direct toxic effect of penicillins affects the CNS. Penicillins increase the irritability of neuron. It is used in experimental pharmacology for the intracerebral administration of penicillin to induce epilepsy in small laboratory animals and for the testing of antiepiletics. For this reason, we avoid intrathecal administration of penicillins. A direct effect on the CNS may occur even after administration so high (MIU) doses, especially in inflammatory meninx or reduced renal excretion.
Indications and contraindications[2][edit | edit source]
OWe usually use penicillins for treatment of repiratory infections, in the emprical therapy of community-acquired infections, in the treatment of nosocomial infections.
They are often combined with aminoglycosides.[1] Interactions with other drugs are rare.
Penicillin allegies and increased seizures are contraindicated. High Na+ and K+ levels should be consdered in cardiac and renal impairment.
Overview of penicillins[edit | edit source]
| basic penicillins | penicilin G, penicilin V | |
|---|---|---|
| antistaphylococcal penicillins | oxacillin, cloxacillin, dicloxacillin, flucloxacillin | |
| broad-spectrum penicillins | aminopenicillins | ampicillin, amoxicillin |
| carboxypenicillins | ticarcillin | |
| acylureidopenicillins | piperacillin | |
Basic penicillins[edit | edit source]
They include a group of acid-labile and acid-stable penicillins of narrow antimicrobial spectrum.
- Template:HVLP (benzylpenicilin)[2][1]
Penicillin G
It is not acid-resistant and therefore is not absorbed after oral administration, therefore it must be administered parenterally. It is not resistant to β-laktamases. It works against both G+ and G- bacteria.
We use it as a drug of first choice in the treatment of infections caused by pneumococci, streptococci, meningococci, gonococci and staphylococci not producing β-laktamase, Bacillus anthracis and other G+ microorganisms, Treponema pallidum (syphilis) and other spirochetes, clostridia, actinomycetis, listerie a Bacteroides (s výjimkou B. fragilis), some Borrelia (a drug of first choice for Lyme disease). It is therefore used in the treatment of gonorrhea, diphtheria, measles, tonsillitis, erysipelas, rheumatic fever, leptospirosis. Some anaerobes are also sensitive.
- Crystalline benzylpenicillin – vaqueous solution of potassium or sodium salt, well soluble in water for i.v. administration (infusion), first-line drug for meningococcal meningitis, me\neumoncoccal pneumonia, S. pyogenes, clostridial infections, actinomycetes.
- Procaine-benzylpenicillin – suspension for i.m. administration (cannot be administered by i.v.), procaine increases the size of the molecule and thus prolongs the absorption and persistence of plasma concentrations, the drug of first choice for sleeping sores adn streptococcal tonsilopharyngitis.
- Benzatin-benzylpenicillin[2] –suspension with very low solubility in water, intended for strictly i.m. administration. It is absorbed very slowly, reaching low plasma concentrations that persit for a long time (up to 10 days). It is suitable for the treatment of acute naasopharyngitis caused by beta-hemolytic streptococci, as a prevention of rheumatic endocarditis.
The usual dose is 2-30 mil. IU. every 4-6 hours in the infusion (0,5 mil. IU)[3] Increased potassium intake should be expected when benzylpenicillin potassium is administered.
- Template:HVLP (phenoxymethylpenicillin)[2][1]

Penicillin V
Acid-resistant (potassium salt), therefore, is not inactivated in the acidic environment of the stomach, so it can be administered orally. Bioavailability is about 60 %. Within 6 hours, its level reaches the limit of effectiveness.
The same antimicrobial spectrum as penicillin G is not resistant to β-laktamases. The drug of first choice for streptococcal tonsilopharyngitis (in case of allergy it is replaced by macrolides). Absorption from the GIT is not completely complete, so it is used for mild infections with sensitice bacteria (eg. sinusitis, otitis media, nasopharyngitis, erysipelas, measles, Lyme disease, prophylaxis endocarditis, periodontal and other dental infections).
Antistaphylococcal penicillins[edit | edit source]
These penicillins are resistant to staphylococcal β-laktamases. Their spectrum of action is staphylococci and streptococci. They are used where other penicillins are not effective.
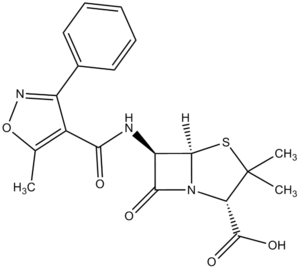
Isoazolylpenicillins[edit | edit source]
Oxacillin
They are given orally for less severe staphylococcal infections. Oxacillin is usually indicated when penicillin-resistant staphylococci are detected. Recently, the resistance of staphylococci (Staphylococcus aureus, Staphylococcus epidermidis) to oxacillin (MRSA) has been increasing.
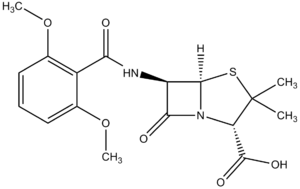
Methoxypenicillins[edit | edit source]
Methicillin
It is not registered in the Czech Republic. It is considered a standard antistaphylococcal anibiotic worldwide. In the acidic environment of the stomach, it is inactivated, so it is usually administered only parenterally. Efficacy against staphylococci is identical to oxacillin.
Broad-spectrum oenicillins[2][1][4][5][edit | edit source]
It differes from basic penicillins by a wider antimicrobial spectrum, which can be extended even more in combination with beta-lactamase inhibitors. Use in common respiratory tract infections, urinary tract infections, skin and soft tissue infections caused by eg. Streptococcus pyogenes, Streptococcus pneumoniae, Haemophilus influenzae and Neisseria catarrhalis.
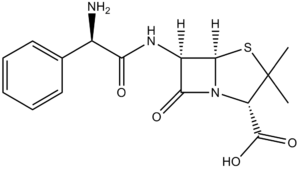
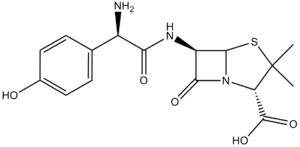
Aminopenicillins[edit | edit source]
Acid-resistant, semisynthetic antibiotic, not resistant to beta-lactamases. More effective on Enterococcus spp. and Listeria monocytogenes.
Ampicillin
Empirical treatment of community bacterial respiratory infections, urinary tract, typhoid fever, septic salmonella, listeriosis and meningitis. Absorption is limited by food, administered on an empty stomach, and may be administered by i.m.
Amoxicillin
The ampicillin analogue, a broader spectrum of action, produces higher serum levels. The advantage is complete absorption after oral administration, which isi not limited by food. Part of regimens eradicating Helicobacter pylori.
Carboxypenicillins[edit | edit source]
The broad spectrum of action, partly against Pseudomonas aeruginosa, is not resistant to β-laktamases. Currently, no representative is registered in the Czech Republic.
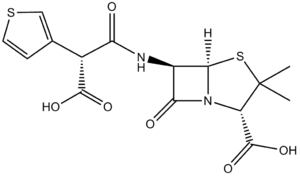
Ticarcillin
Effective on G- microbes that are resistant to ampicillin. It is often combined with beta-lactamase inhibitors and combined with aminoglycosides (because resistance develops rapidly in monotherapy). It is administered only i.v.
Acylureidopenicillins[edit | edit source]
The spectrum of action is even wider than ticarcillin, they are not resistant to β-laktamases.
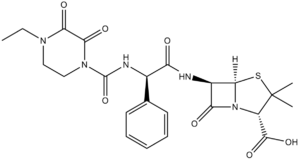
Piperacilin
It is often combined with tazobactam. The product is effective against both G+ and G- bacteria, including nosocomial pathogens. It acts on Bacteroides sp. and Clostridia sp., do not affect MRSA. In severe infections, their effect is enhanced by combination with aminoglycosides.
Links[edit | edit source]
[edit | edit source]
External links[edit | edit source]
- https://www1.lf1.cuni.cz/~hrozs/Atb2011/antibio02.htm
- Peniciliny (česká wikipedie)
- Penicillin (anglická wikipedie)
Source[edit | edit source]
- ws:Peniciliny
- BENEŠ, Jiří. Study materials [online]. [feeling. 2010]. < http://jirben.wz.cz >.
- LINCOVÁ, Dagmar and Hassan FARGHALI, et al. Basic and applied pharmacology. 1st edition. Prague: Galén, 2002. ISBN 80-7262-168-8 .
- MARTÍNKOVÁ, Jiřina, et al. Pharmacology for medical students. 2nd edition. Prague: Grada, 2018. ISBN 978-80-271-0929-6 .
- JAN, Švihovec and A KOLEKTIV. Pharmacology. - edition. Grada Publishing as, 2018. 1008 pp. ISBN 9788027121502
Reference[edit | edit source]
1. LINCOVÁ, Dagmar and Hassan FARGHALI, et al. Basic and applied pharmacology. 2nd edition. Prague: Galén, 2007. ISBN 978-80-7262-373-0 .
2. MARTÍNKOVÁ, Jiřina, et al. Pharmacology for medical students. 2nd edition. Prague: Grada, 2018. ISBN 978-80-271-0929-6 .
3. ŠVIHOVEC, Jan, et al. Pharmacology. 1st edition. Prague: Grada, 2018. ISBN 978-80-271-2150-2 .
4. HAVLÍK, Jiří, et al. Infectious diseases. 2nd edition. Prague: Avicenum, 1990. 393 pp. ISBN 80-201-0062-8 .
5. LOBOVSKÁ, Alena. Infectious diseases. 1st edition. Prague: Karolinum, 2001. 263 pp. ISBN 80-246-0116-8 .