Syphilis
Syphilis (acute, lues or lues venerea) is a worldwide infectious chronic systemic disease with a characteristic course of alternating symptomatic and asymptomatic periods. It is transmitted mainly through sexual intercourse.
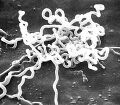
Treponema pallidum
The causative agent of syphilis is an anaerobic spiral fibrous bacteria belonging to spirochetes. It is primarily pathogenic to humans, who are its only host in nature.
Pathogenicity
Treponema pallidum is naturally pathogenic to humans only. There are three possible transmission paths:
- sexual intercourse;
- transmission by contaminated objects;
- penetration through the placenta and infection of the fetus (adrenal syphilis develops).
By far the most common transmission is sexual intercourse, because the resistance of T. pallidum is very low and it dies quickly when away from the body. It is destroyed by oxygen, temperatures above 39 ° C, diluted solutions of common disinfectants and dies in blood cans within 4 hours. Transmission by contaminated objects is extremely rare.
Pathogeneses
Treponema pallidum penetrates the body through the mucous membranes or skin. It multiplies extracellularly and does not have a chemotactic effect on polymorphonuclear leukocytes. Virulent strains are coated with a mucous layer that prevents treponem from killing in phagocytes and from attaching complement or antibodies to its surface. Morphological changes (characteristic of all stages) are caused by capillary endothelial damage and dysfunction. It is not the bacteria themselves but the immunopathological processes that arise in response to the presence of Treponem in the body and which lead to extensive destruction at a time when Treponemas are almost eliminated from the body.
- Causes of syphilis symptoms
- capillary endothelial damage;
- immunopathological changes:
- immunocomplexes of antigens and antibodies (antigens are largely released during the breakdown of bacteria);
- cell hypersensitivity.
Imunita
Specific immunity (both antibody and cellular) against treponemas develops during the course of the disease. Cell hypersensitivity is due to activation of macrophages. Immune reactions can lead to complete recovery in the untreated. Protection against a new infection is only in the early stages, reinfection is possible.
- It can affect virtually any tissue or organ, and untreated disease can cause death or disability. The infection can be transmitted to the fetusduring pregnancy (early and late congenital syphilis).[1]
Characteristics
- Incidence in the Czech Republic in 2009: 997 cases (ie 10 per 100 thousand inhabitants, of which 22% of foreigners), in 2006: 502 cases (5 per 100 thousand inhabitants).[2]
- Originator: spirocheta Treponema pallidum.
- Transmission: sexual intercourse, transplacental, blood transfusion.
- Place of entry: any area of skin and mucous membranes, most often the genital, rectal and oral mucosa.
- Incubation period: 21 days (9-90 days).[3]
- Risk groups: drug addicts, patients with AIDS.
- It is infectious from primary infection until the end of the 2nd year of the disease (ie stage 1 and 2).[4] Isolation in the venereology department is therefore mandatory in patients with stage 1 and 2 syphilis.[5]
- Subject to reporting.
- There is no vaccination.
Clinical picture
Acquired syphilis typically develops in three clinical stages.
Primary stage
The primary stage is characterized by changes in the site of infection. The incubation period from infection to manifestations on the mucosa or skin is about 21 days. The following lesions are characteristic of the primary stage of syphilis:
- Ulcus durum (hard ulcer):
- at first a flat papule changing gradually in erosion and ulcer;
- raised margins, deep red base;
- palpable (gloved!) stiff ulcer with indurated edges;
- painless;
- lymphocytes, plasma cells and macrophages predominate in the infiltrate;
- treponems survive intracellularly after the primary infection has healed.
2. Regional lymphadenitis (swelling of the descending nodes)
- arises in 1-2 weeks;
- the nodules are enlarged, painless and reddish.
Antibodies generated in the primary stage do not prevent the development of the secondary stage.
Secondary stage
The secondary stage is a manifestation of the generalization of the infection, it occurs within two years of the primary infection. Treponemata multiply in the bloodstream. The manifestation is maculopapular rash on the skin and mucous membranes. The concentration of antibodies increases significantly and immunocomplexes are formed.
- Manifestations of generalization of infection
- skin rash - macules or papules 0.5–1 cm, red, may be covered with scales
- condylomata lata - papules to bumps, red or skin color;
- leucoderma syphiliticum - depigmentation of the neck;
- on the mucous membranes of the enanthema (mucous membranes of the mouth, genitals);
- alopecia areolaris (diffuse alopecia in the forehead and beard, loss of eyelashes and lateral thirds of the eyebrows);
- hepatitis, lymphadenitis (lasts 2-8 weeks), from 6 months in 25% neurological symptoms - acute syphilitic meningitis.
The first and second stages are contagious.
Tertiary stage
The tertiary stage is a late and non-infectious manifestation of lues after varying lengths of latency. Treponemata show up only rarely. Organ changes develop, vascular damage and CNS damage occur.
- Manifestations of tertiary syphilis
- rubber:
- sharply demarcated bumps (on the skin and internal organs), obviously red, palpably stiff, collapsed in the center;
- the contents perforate on the outside, an ulcer is formed and a viscous yellowish fluid flows out;
- heals with a depigmented scar;
- skin - syphilis noduloulcerosa:
- papules and bumps merging into deposits of deep red color, heal in the center with an atrophic pigment scar;
- on extensors, back and face;
- in 7% neurological symptoms - progressive paralysis, dorsal tabes
- In 25% of untreated lues, acute syphilitic meningitis occurs no earlier than 6 months after primary infection;
- it is caused by the meningeal invasion of Treponema pallidum (a spirochete sensitive to environmental influences);
- does not affect the brain parenchyma.
- Some untreated obliterative endarteritis (syphilis meningovasculosa), chronic subpilar meningitis (syphilis spinalis), and optic atrophy appear 5-15 years after infection.
- Some people do not have to go through all stages of the disease, about a third of people recover after the primary infection without treatment, and another third remain infected with no clinical manifestations. Only one third of patients develop the tertiary stage.
Congenital syphilis
See the Congenital Syphilis page for more information.
Congenital syphilis is caused by transplacental transmission of the disease from mother to fetus. In maternal infection in II. In the first trimester of pregnancy, syphilis congenita tarda (school-age manifestations, Hutchinson's Triassic and bone involvement) develops when the mother becomes infected in III. during the trimester of pregnancy, syphilis congenita praecox (manifestation in neonatal age, symptoms of stage 2 syphilis) occurs.
Hutchinson's Triassic: blindness, deafness, barrel-shaped teeth.
Links
Related Articles
- Syphilis
- Congenital syphilis
- Treponema pallidum
External links
- Syfilis (česká wikipedie)
- Syphilis (anglická wikipedie)
Reference
- ↑ SEIDL, Zdeněk and Jiří OBENBERGER. Neurology for study and practice. 1st edition. Prague: Grada Publishing, 2004. ISBN 80-247-0623-7.↑ DOSTÁL, Václav, et al. Infectious diseases. 1st edition. Prague: Karolinum, 2005. ISBN 80-246-0749-2.
References
- SEIDL, Zdeněk and Jiří OBENBERGER. Neurology for study and practice. 1st edition. Prague: Grada Publishing, 2004. ISBN 80-247-0623-7.
- POVÝŠIL, Ctibor and Ivo ŠTEINER, et al. Special pathology. 2nd edition. Prague: Galén-Karolinum, 2007. pp. 297-299. ISBN 978-80-7262-494-2.
- DOSTAL, Vaclav, et al. Infectious diseases. 1st edition. Prague: Karolinum, 2005. ISBN 80-246-0749-2.
- BEDNÁŘ, Marek, et al. Medical microbiology. 1st edition. Prague: Marvil, 1996. 558 pp. 186.
Diagnostics
- clinical picture, anamnesis
- indirect diagnostics - serological examination of antibodies:
- non-treponemal tests (VDRL, RRR) - show non-specific anticardiolipin antibodies ("reagins")
- treponema tests (TPHA, FTA, ELISA, ...) - show specific antibodies against Treponema pallidum antigens
- Non-specific antibodies disappear within weeks to months after effective treatment, but specific IgG remains detectable over a long period of time.[6]
- direct diagnostics:
- examination under a shadow microscope
- basic, standard examination in case of suspicion of a specific lesion on the skin or mucosa
- allows to examine serous exudate from lesions, cerebrospinal fluid, amniotic fluid, etc.
- PCR (polymerase chain reaction)
- direct immunofluorescence antigen detection (DFA-TP) - expensive, not available in our country
- histopathological examination (silver impregnation) - lengthy and burdened with a number of artifacts[7]
- examination under a shadow microscope
Serological examinations
- RRR (Rapid Reaction Reaction) or RPR (Rapid Plasma Reagin) - a cheap screening test
- microflocculation reactions where the antigen is cardiolipin mixed with cholesterol and lecithin
- Cardiolipin is a phospholipid (hapten) contained in the membrane of Treponema pallidum, but also in other bacteria and also in mitochondria
- anti-cardiolipin antibodies produced in syphilis are called "reagents"
- clusters form when the antigen meets the antibodies
- may be false positive (for tumors, pregnancy, malaria), therefore positivity needs to be confirmed eg by TPHA test[8]
- VDRL (Venereal disease research laboratory) microscopic test
- can be used to test serum and cerebrospinal fluid[7]
- TPHA (Treponema pallidum hemagglutination) or MHA-TP (micro hemagglutination of T. pallidum) - cheap screening test
- FTA-ABS IgG, IgM (fluorescent treponemal antibody – absorbed)
- allows diagnosis from the 2nd to the 3rd week of syphilis
- the antigen is Nichols strain T. pallidum
- a so-called sorbent is used to remove cross-reactive antibodies from the patient's serum
- the patient's antibodies are labeled with a fluorescent dye and fluorescent upon reaction with the antigen
- evaluation of the immunofluorescence response is subjective
- tends to be false positive in systemic lupus erythematosus[9]
- ELISA
- Westernblot (WB)
- Previously, Nelson's (-Mayer's) Treponema pallidum immobilization test (TOPIT) and BWR (Bordet-Wasserman reaction) - complement fixation reaction - were used.
Laboratory diagnosis of neurosyphilis
- examination of serum and cerebrospinal fluid
- positive treponemal (specific) serological tests (TPHA, ELISA, etc.) are a prerequisite.[10]
- in cerebrospinal fluid there is lymphocytic pleocytosis, proteinocytological association, proliferation of immunoglobulins[4]
- positive intrathecal antibody production and TPHA index
- WHO (1982) neurosyphilis criteria: pleocytosis, cardiolipin test positivity (CSF-VDRL) and elevated cerebrospinal fluid protein levels.[10]
- To rule out neurosyphilis in a patient with positive seroreactions, the negativity of specific cerebrospinal fluid tests is sufficient for me.[10]
Clinical picture
- we most often encounter cranial nerve damage, which is typical for all stages
- Argyll-Robertson pupils (isocorbic, remarkably broad, non-rounded, do not respond to exposure in a preserved response to convergence) - cause: lesion n. III or directly mesencephalus
- papillary edema followed by atrophy n. II and blindness
- deafness is a consequence of the lesion n. VIII
Therapy
- Penicillin is a causal treatment for all stages of the disease
- All forms of syphilis are treatable, the better the results the sooner penicilin is administered
- Penicilin G i.v. 2-4 MIU after 4 hours 10-14 days
- Procain penicillin G G i.m. 2-4 MIU (and probenecid 500 mg / 6 h) after 24 hours - a total of 15 days
- Pendepon (benzathine benzylpenicillin) i.m. 2-4 MIU every 7 days for 3 weeks
- Jarisch-Herxheimerova reaction - fever and tachycardia at the beginning of treatment, the body's response to endotoxin from decayed spirochetes, responds favorably to corticoid treatment
- in case of hypersensitivity to penicillin → p.o. erythromycin or tetracycline for 30 days
- tobacco crisis (see below) will affect atropine in part[4]
Acute syphilitic meningitis
- The first manifestation of untreated neurolues, has 3 forms:
- asymptomatic - most, shows only an accidental finding in the cerebrospinal fluid after lumbar puncture.
- aseptic - fatigue, meningeal syndrome, febrile rash
- acute basal - hydrocephalus, cranial nerve lesions (n. VII, VIII), papillary edema n. II
- fluid: lymphocytes 100–1000 cells / mm3, increased protein 0.5–2 g / l, sugars decreased, RRR +
- treatment: 1st and 2nd stage - penicillin[4]
Late neurological consequences of untreated syphilis
- rare
- in those not treated at the earliest 5 years after the infection during the latency period[4]
Meningovascular syphilis (5-10 years)
Spinal syphilis (10-15 years)
- the spinal cord is affected by subpiically chronic meningitis
- radicular pain, upper limb muscle atrophy, paraplegia[4]
Optical atrophy (in 10-15 years)
- chronic meningitis and subpilar necrosis exclusively around n. II bilaterally and bilaterally
- the narrows
- cerebrospinal fluid is always the same in untreated syphilis with late neurological consequences: lymphocytic pleocytosis 100 / mm3, increased protein and gamma globulins, positive serology
- penicilin is the drug of choice[4]
Progressive paralysis (in 15-20 years)
- subacute meningoencephalitis with predominantly frontal involvement
- very rare today
- neurastenie → poruchy afektivity (manie), koncentrace, chování, úsudku a paměti → progresivní demence – preparalytické stadium
- paralytic stage - + corticospinal, extrapyramidal, myoclonus, or Argyll-Robertson pupil, dysarthria, epilepsy → ends with personality breakdown and general marasmus, sudden death - ictus paralyticus
- most often - megalomaniac form - giant delusions, depressive form, simplex form - picture of progressing dementia, Lissauer form - neurological symptomatology, cerebrospinal fluid paralysis - cerebrospinal fluid finding, without clinical manifestation
- dg: seropositivity - treponemal reactions (TPHA, TPI)
- fluid: lymphocytic pleocytosis 50 / mm3, protein 0.5–2 g / l, gamma globulins +++, RRR +
- autopsy: brain atrophy. cortex, diaper thickening, lymphocyte and plasma cell infiltrates around blood vessels, microglia proliferation, neuronal degeneration
- penicillin stops progression in 40% of patients (formerly Wagner-Jauregg - malariotherapy)[4]
Tabes dorsalis (in 15-20 years)
- atrophy of the posterior cords and spinal roots
- Inflammation occurs on the spinal cord as chronic progressive meningitis
- very rare
- it also affects the optic nerves (20% have papillary atrophy)
- ataxia, imbalances, hyporeflexia (up to patellar and Achilles tendon areflexia), lanceic lower limb pain, trophic and pupil changes (90% miotic unresponsive to exposure, positive Romberg symptom
- tobacco crises = visceral colic that faithfully mimics a sudden abdominal event - pain, nausea, vomiting, tenezms, diarrhea
- bouts of burning paresthesias often affect the sciatic nerve and the ulnar nerve.
- incontinence, impotence, genital numbness
- painless joint deformities, trophic ulcers on the leg (malum perforans) are the result of trauma from a lack of proprioception, with no hope of improvement
- cerebrospinal fluid is closer to normal than in progressive paralysis, IgG, lymphocytic pleocytosis to several dozen elements is increased. moderate hyperproteinosis, RRR is up to 30% negative
- syphilitic gum is extremely rare, as infiltrative limited inflammation affects not only the brain but also other organs, such as the liver[4]
Bone syphilis
- rare
- adrenal syphilis: osteochodritis growth plates of long bones, reactive periostitis (bone line doubling)
- acquired syphilis: negumous periostitis with skull and tibia involvement / gummy syphilitic periostitis and destructive osteomyelitis(defects in the skull, perforation of the palate, compression fractures of the vertebrae)[11]
Links
Related articles
External links
Sources
- ↑ DOSTÁL, Václav, et al. Infektologie. 1. edition. Praha : Karolinum, 2005. ISBN 80-246-0749-2.
- ↑ ÚSTAV ZDRAVOTNICKÝCH INFORMACÍ A STATISTIKY ČR,, et al. Pohlavní nemoci 2009 [online]. [cit. 2011-07-17]. <http://www.uzis.cz/category/klicova-slova/zdravotni-stav/pohlavni-nemoci>.
- ↑ POLÁČKOVÁ, Z. Pohlavní choroby I. díl. Dermatologie pro praxi [online]. 2008, vol. 2, p. 74-76, Available from <http://www.solen.cz/pdfs/der/2008/02/06.pdf>.
- ↑ a b c d e f g h i j SEIDL, Zdeněk – OBENBERGER, Jiří. Neurologie pro studium i praxi. 2. edition. Praha : Grada Publishing, 2004. ISBN 80-247-0623-7.
- ↑ Česká republika. Sbírka zákonů č. 275 / 2010. 2010. Available from <http://www.szu.cz/uploads/sb103_10_1_novela.pdf>.
- ↑ http://www.medmicro.info/portal/syfilis/lvl3/ch09.html
- ↑ a b http://www.szu.cz/tema/prevence/syfilis-tradicni-choroba-soucasny-problem-ii
- ↑ a b http://mikrobiologie.lf3.cuni.cz/mikrobiologie/bak/uceb/obsah/lues/lues.htm
- ↑ a b http://www.medmicro.info/portal/syfilis/lvl3/ch09s05.html
- ↑ a b c http://www.medmicro.info/portal/syfilis/lvl3/ch05s03.html
- ↑ POVÝŠIL, Ctibor – ŠTEINER, Ivo, et al. Speciální patologie. 2.. edition. Praha : Galén-Karolinum, 2007. pp. 297-299. ISBN 978-80-7262-494-2.
Use literature
- SEIDL, Zdeněk – OBENBERGER, Jiří. Neurologie pro studium i praxi. 1. edition. Praha : Grada Publishing, 2004. ISBN 80-247-0623-7.
- POVÝŠIL, Ctibor – ŠTEINER, Ivo, et al. Speciální patologie. 2.. edition. Praha : Galén-Karolinum, 2007. pp. 297-299. ISBN 978-80-7262-494-2.
- DOSTÁL, Václav, et al. Infektologie. 1. edition. Praha : Karolinum, 2005. ISBN 80-246-0749-2.
- NEVŠÍMALOVÁ, – RŮŽIČKA, Evžen – TICHÝ, Jiří. Neurologie. 1. edition. Praha : Galén, 2002. ISBN 80-7262-160-2.