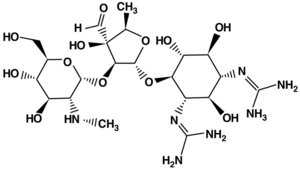
Aminoglycosides
Aminoglycosides are bactericidal antibiotics, mainly used in hospitals.
Mechanism of action[edit | edit source]
They inhibit protein synthesis by irreversible binding to the 30S subunit of the ribosome.
Antimicrobial spectrum[edit | edit source]
Aminoglycosides are mainly effective against infections caused by Gram-negatives (Escherichia, Klebsiella, Enterobacter, Serratia, Citrobacter, Pseudomonas, Acinetobacter, Salmonella, Shigella) and Gram-positives (Staphylococcus aureus, including β-lactamase-producing strains, Staphylococcus epidermidis). Less sensitive to resistant are streptococci and enterococci. Anaerobes are naturally resistant.
Pharmacokinetics[edit | edit source]
Aminoglycosides are not absorbed per os and act locally in the GIT. They are used parenterally (mostly i.v.). They are also well absorbed after i.m. administration. They penetrate poorly into body fluids and tissues. They are not metabolised and are excreted by glomerular filtration. Elimination is markedly reduced in renal impairment (in patients with renal insufficiency and failure; in children in the first week of life, especially premature infants due to renal immaturity; in old age when glomerular filtration decreases due to reduced renal blood flow). In these cases, aminoglycosides may accumulate and cause toxic damage. In the renal tubules, they enter cells by active transport and penetrate into lysosomes, where they cause intracellular shedding of autolytic lysosomal enzymes and subsequent cell autolysis and necrosis.
Pharmacodynamics[edit | edit source]
The effect of aminoglycosides is dependent on plasma concentration. They are hydrophilic, so they do not penetrate biological membranes easily. They are subject to active O2-dependent transport across the inner part of the membrane (therefore they do not act on anaerobes). They induce a rapid killing phase (6 h), followed by a bacteriostasis phase (even when antibiotic concentrations are low), when bacterial regrowth does not occur. This phase is also called the "post-antibiotic effect" (PAE). Its magnitude is determined by the size of the cmax, and the type of bacteria. It is amplified by the presence of leukocytes. Combination with β-lactams facilitates penetration by passive diffusion.
Side effects and toxicity[edit | edit source]
Aminoglycosides are potentially ototoxic. Ototoxicity may be acute (after high dose) from reversible blockade of calcium current in hair cells, which can be corrected by calcium administration because of the competitive antagonism between the antibiotic and calcium. Chronic ototoxicity is attributed to the time of exposure (AUC) and is up to 50% irreversible, unpredictable, sudden and intense after 5-7 days of treatment. Adverse effects include neurotoxicity. Aminoglycosides are also nephrotoxic due to their effect on the renal tubules. The damage tends to be reversible. It is important to note that they are one of the few antibiotics whose effect and toxicity correlate closely with plasma concentrations (better than dose). Yet the difference between the concentrations underlying antibiotic and toxic effects is small (they have a narrow therapeutic window). Therapeutic drug monitoring (TDM) is performed.
Benefits of aminoglycosides[edit | edit source]
- Bactericidal
- postantibiotic effect
- low price
Indications[edit | edit source]
Treatment with aminoglycoside antibiotics is indicated for more serious infections: septic conditions, CNS infections, respiratory tract infections (pneumonia), intra-abdominal and hepatobiliary infections, endocarditis, complicated urinary tract infections with sensitive agents included in the antibiotic spectrum. In monotherapy they are used only in urinary tract infections, otherwise in combination mostly with β-lactams. In enterococcal endocarditis in combination with ampicillin.
Representatives of antibiotics[edit | edit source]
- basic aminoglycosides of older type (with defined indication): streptomycin, neomycin, kanamycin
- highly effective newer ones with lower toxicity: gentamicin, tobramycin, amikacin, netilmicin
Streptomycin
It is the drug of choice for brucellosis, tularemia, nodular fever, used as an antituberculosis. In combination with penicillin, it is used to treat endocarditis caused by viridal streptococci or enterococci.
Gentamicin
The basic broad-spectrum antibiotic of this group. It should not be given to pregnant women, newborns and premature infants. Adverse effects include nephrotoxicity (albuminuria, proteinuria), ototoxicity (dizziness, vertigo), curareform effects (neostigmine is an antagonist), skin manifestations, increased liver tests, changes in blood pressure and others.
Amikacin
It is used to treat infections that are caused by gentamicin-resistant microbes.
Links[edit | edit source]
Related articles[edit | edit source]
Sources[edit | edit source]
- MARTÍNKOVÁ, J., S. MIČUDA a J. CERMANOVÁ. Antibiotika [online]. [cit. 2010-07-25]. <https://www.lfhk.cuni.cz/farmakol/predn/bak/kapitoly/atb-bak.doc/>.
- LINCOVÁ, Dagmar a Hassan FARGHALI, et al. Základní a aplikovaná farmakologie. 2. vydání. Praha : Galén, 2007. ISBN 978-80-7262-373-0.
Antibiotics and chemoterapeutics[edit | edit source]
| baktericidal | aminoglycosides | amikacin, gentamycin, isepamycin, neomycin, netilmicin, spectinomycin, streptomycin, tobramycin | ||
|---|---|---|---|---|
| antituberkulotics | izoniazid, cykloserin, ethambutol, ethionamid, kapreomycin, pyrazinamid, viomycin | |||
|
|
cephalosporins | I.generation | cafazolin, cefadroxil, cefalexin, cefalotin, cefapirin | |
| II.generation | cefuroxim, cefamandol, cefpodoxim, proxetil, cefprozil monohydrate, cefuroxim-axetil | |||
| III.generation | cefotaxim, cefetamet pivoxil, cefixim, cefoperazon, cefsulodin, ceftazidim, ceftibuten, ceftriaxon, co-cefoperazon | |||
| IV.generation | cefepim, cefpirom | |||
| V.generation | ceftarolin | |||
| carbapenems | imipenem, doripenem, ertapenem, merapenem | |||
| monobaktams | aztreonam | |||
| penicillins | narrow-spectrum penicillins | penicillin G, penicillin V, cloxacilin, dicloxacilin, oxacilin, flucloxacilin | ||
| broad-spectrum penicillins | amoxicilin, ampicilin, ticarcilin, piperacilin | |||
| beta-lactam inhibitors | co-amoxicilin, co-ticarcilin, sulbaktam, tazobaktam | |||
| glycopeptides | teikoplanin, vankomycin | |||
| quinolones | I.generation | nalidixic acid, oxolinic acid | ||
| II.generation | ciprofloxacin, norfloxacin, pipemicid acid, rosoxacin | |||
| III.generation | sparfloxacin, enoxacin, floroxacin, lomefloxacin, ofloxacin, pefloxacin | |||
| IV.generation | moxifloxacin | |||
| nitroimidazoles | metronidazol, ornidazol | |||
| nitrofurans | furazolidon, nifuratel, nifuroxazid, nitrofurantoin, | |||
| polypeptide antibiotics | bacitracin, colistin, gramicidin, polymyxin B | |||
| rifamycins | rifampicin, rifabutin, rifaximin, rifamycin | |||
| bakteriostatic | amphenicol | azidamfenikol, chloramfenikol, florfenikol, thiamfenikol | ||
| glycylcyclines | tigecyclin | |||
| lincosamides | klindamycin, linkomycin | |||
| macrolides | I.generation | erytromycin, josamycin, oleandomycin, spiramycin | ||
| II.generation | azithromycin, clarithromycin, roxithromycin | |||
| oxazolidinones | linezolid | |||
| pyrimidines | co-trimoxazol, pyrimetamin, trimetoprim | |||
| streptogramins | streptogramin A, B | |||
| sulphonamides | sulfamothoxazol, sulfasalazin, sulfathiazol, sulfisoxazol | |||
| sulfones | dapson | |||
| tetracyclines | doxycyklin | |||