Periodontitis
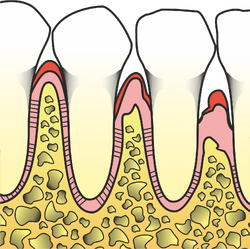
Periodontitis is a disease of all components of the suspension apparatus. . They are typical of the formation of true periodontal trunks. There is destruction of the epithelial attachment and, gradually, changes to the bone (resorption).
Etiopathogenesis[edit | edit source]
Main etiological factors:
- microbial plaque bacteria,
- the susceptible immune system of an individual.
There is destruction of the epithelial attachment and, gradually, changes to the bone (resorption).
Secondary factors:
- hormonal influences,
- diabetes mellitus,
- smoking,
- increased plaque retention plaku (overhanging fillings, inadequate prosthetic work, hyperplastic gums, orthodontic anomalies, side effects of drugs, ...)
- traumatic articulation,,
- anatomical deviations of soft tissues (shallow vestibule, pull of frenulum, ...)
Plaque theory[edit | edit source]
- Non-specific plaque theory
- The quantity of bacteria plays a greater role than species representation (non-specific infection). It mainly applies to marginal periodontitis.
- Specific plaque theory
- A specific periodontal pathogen, or their group. Applies to juvenile periodontitis.
- Exogenous plaque theory
- The infection is caused by bacteria that are not found in the physiological microflora of the plaque.
Clinical picture[edit | edit source]
Right periodontal trunk[edit | edit source]
It penetrates through loss of attachment due to destruction of collagen fibers, resorption of alveolar bone and apical migration of connective epithelium. We distinguish 2 types:
- The supraalveolar trunk ends above the level of the alveolar bone.
- The intraalveolar trunk ends below the level of the alveolar bone.
Alveolar bone resorption[edit | edit source]
Initially, the compacta decreases and gradually the edge of the alveolar bone decreases. There are 2 basic types of resorption:
- Inhorizontal resorption the septa are equally affected and the resorptive surface thus forms a line.
- Vertical resorption is steeply inclined towards the affected tooth. Typical for overloaded teeth (traumatic articulation, …)
Types of bone defects[edit | edit source]
According to the relationship of alveolar bone resorption to the tooth or teeth, we distinguish the following types of bone defects:
- A three-walled bone defect occurs in the case of alveolar bone involvement only in relation to 1 tooth.
- in a double-walled bone defect, esorption affects both adjacent teeth.
- A single-walled bone defect also includes resorption of the oral or vestibular wall of the alveolar bone.
- in a circular bone defect, the bone around the tooth is missing.
Impairment of furcations[edit | edit source]
In multi-rooted teeth (molars) bone resorption can also occur between the individual roots. Impairment of the furcation is detected with a special Nabers probe, which is calibrated and has an arc-shaped shape.
- Furcation is not affected ( F0 ).
- Affected part of the furcation, the probe reaches between the roots up to 3 mm (F1).
- The probe extends between the roots further than 3 mm (F2).
- The entire furcation is affected, the probe can be penetrated through (F3).
Other symptoms of periodontitis[edit | edit source]
In advanced forms of periodontitis,;the teeth become loose and a very late symptom is the so-called;wandering of the teeth. Recessions, may also occur , which are receding gums that lead to the exposure of the necks and roots. are also common . Periodontal abscesses.
Loose teeth[edit | edit source]
We perform the gait examination bimanually using the fingers or a finger and a tool.
- Grade I wobble means horizontal mobility up to 1 mm.
- Clumsiness II. degree is only horizontal mobility up to 3 mm.
- Clumsiness III. degrees we denote mobility of the tooth in the vertical direction and greater mobility in the horizontal direction.
Teeth wandering[edit | edit source]
A spontaneous change in the position of the teeth is typical for the upper frontal teeth in advanced periodontitis. The upper incisors move apart and protrude.
Diagnostics[edit | edit source]
Clinical examination:
- bleeding after probing;
- periodontal trunks deeper than 3.5 mm;
- looseness of teeth;
- tooth migration.
X-ray vyšetření – X-ray status (intraoral images):
- rubbed, unclear compact;
- vertical/horizontal bone resorption.
Therapy of periodontitis[edit | edit source]
TWe plan therapy for each patient individually, according to a specific finding. In general, it can be divided into several stages.
- Initial therapy
- regulation hygiene;
- patient education and motivation;
- restoration of teeth;
- scaling, root planing;
- prosthetic treatment plan;
- ground glass;
- splinting.
- Surgical phase
- extraction of teeth with poor prognosis;
- reactive periodontological procedures.
- Reconstructive (prosthetic) phase
- Maintenance phase
- repeated visits, examination, motivation, instruction.
Individual types of periodontitis[edit | edit source]
Marginal periodontitis[edit | edit source]
It is an inflammatory, bacterial plaque induced disease of all parts of the marginal periodontium, i.e gingiva , periodontium, cementum and alveolar bone. It is associated with loss of supporting tissues.
Clinical picture[edit | edit source]
- symptoms of gingivitis;
- bone loss, abscesses , tooth displacements and inclinations;
- periodontal trunks with loss of attachment;
- increased tooth mobility (late symptom);
- affected individual teeth, groups of teeth and the entire dentition;
- active trunk = trunk with typical signs of inflammation (bleeding, exudate, ...);
- bumpy course – a period of progression alternates with a period of stagnation.
Causes[edit | edit source]
- Bacterial infection based on previous gingivitis.
Periodontitis marginalis superficialiss[edit | edit source]
- Inflammatory disease of all components of the periodontium with loss of attachment (radiologically, loss of attachment) up to about 1/3 of the root length (cemento-enamel border - apex).
Periodontitis marginalis profunda[edit | edit source]
- Inflammatory disease of all components of the periodontium with loss of attachment (radiological bone resorption) of more than 1/3 of the root length or with furcation involvement
Division according to the rate of progression and according to the age of the patient[edit | edit source]
Prepubertal periodontitis[edit | edit source]
- already during the eruption of milk teeth (2-4 years of age);
- localized form – only individual teeth are affected;
- generalized form - all teeth are affected, the gingiva is strongly inflamed - up to the loss of the entire milk dentition, often associated with a general susceptibility to infections (e.g. otitis media);
- cause – mixed bacterial flora, functional defects of granulocytes and monocytes (heredity).
Localized Juvenile Periodontitis (LJP)[edit | edit source]
- from the age of 10 and above;
- severe periodontal lesions – rapidly progressing osteolysis (can slow down to stop) – central incisors, first molars – symmetrical distribution;
- without treatment - localized form - generalized;
- in a short time, complete destruction of the suspension apparatus of the affected teeth may occur;
- gingiva only minimal signs of inflammation !!! (the amount of plaque and calculus does not correlate with the degree of periodontal destruction);
- prevention – probing I1 and M1 in adolescent patients (early detection of the disease);
- often functional defects of granulocytes and monocytes (reduced ability of phagocytosis and chemotaxis, neutrophils are unable to kill phagocytosed bacteria) – AR or GD.
Rapidly progressive periodontitis (RPP)[edit | edit source]
- RPP = rapid progressive periodontitis;
- between puberty and the age of 35 – may arise from juvenile periodontitis;
- patients do not suffer from systemic disease;
- severe periodontal lesions in many teeth;
- different occurrence of plaque – ome patients have a lot, others a little;
- cyclic bone destruction – very fast (periodontal breakdown);
- gingiva only slightly inflammatory;
- microbial flora – G- anaerobes and spirochetes (Porphyromonas gingivalis);
- again possible genetic disposition (defect of monocytes and granulocytes) – GD.
Slowly progressive periodontitis (AP)[edit | edit source]
- AP = adult parodontitis;
- From 30-35 of the year – development on the basis of previous gingivitis;
- bone destruction – not limited to certain groups of teeth (more common in M and I);
- chronic course – in shocks (quiet trunks and active trunks);
- gingiva fibrotic or inflammatory thickened (shrinkage rarely);
- insufficient hygiene, a large amount of supra- and subgingival plaque and stone;
- cause – a large amount of plaque settling in suitable places (subgingival) without a genetic disposition.
Links[edit | edit source]
[edit | edit source]
- Anatomy of the periodontium
- Periodontology - basics
- Pathology of the periodontium
- Gingivitis
- Aggressive periodontitis
External links[edit | edit source]
Source[edit | edit source]
- POLENÍK, Pavel. Patologie parodontu [lecture for subject Preventivní zubní lékařství, specialization Zubní lékařství, LFP UK]. Plzeň. 19.12.2008.
- POLENÍK, Pavel. Subgingivální ošetření v praxi zubního lékaře. 1. edition. Quintessenz, 2008. ISBN 978-80-86979-04-5.
- POLENÍK, Pavel. Odborná praxe zubního lékaře : komplexní průvodce stomatologií. Část 6. 1. edition. Dashöfer, nakladatelství, 2004. ISBN 80-86229-21-1.