Glycemia
The concentration of glucose in blood (blood glucose) is maintained in a narrow range of 3.9-5.6 mmol/l on an empty stomach and after a meal lower than 10 mmol/l. It is tightly regulated by a number of mechanisms: insulin, which lowers blood glucose, and anti-insulin hormones - glucagon, catecholamines, glucocorticoids and growth hormone which increase blood glucose. The liver is also significantly involved in the regulation of glucose homeostasis. Maintaining a constant blood glucose level is essential for the activity of the CNS and other tissues and cells (eg erythrocytes).
Sources of glucose[edit | edit source]
The exogenous glucose source for the body is the Disaccharides and Polysaccharides in the diet. Glucose is formed by their breakdown in the small intestine and is utilized in the liver, muscle, adipose and brain tissue as a direct source of energy. Non-oxidized glucose is stored in the form of glycogen or converted to fatty acids and triacylglycerols. In the fasted state, normal glucose concentration is maintained by glycogen cleavage by glycogenolysis and glucose formation from non-saccharide precursors (amino acids, glycerol and lactate in the gluconeogenesis process.
Changes in blood glucose concentration[edit | edit source]
- A drop in blood glucose below 3.2 mmol/L is referred to as hypoglycemia. In hypoglycemia, the supply of glucose to brain tissue is compromised. It can occur during various diseases, most often in overdose antidiabetics, more rarely in long-term starvation, in some endocrine tumors or inherited metabolic disorders that also affect glucose metabolism (eg in antidiabetics). glycogenosis [glycogenosis]]). Severe hypoglycaemia is accompanied by restlessness, sweating and tremor;
- Glycaemia elevated above the reference range is referred to as hyperglycemia. Chronic hyperglycemia is an underlying manifestation of diabetes. However, we may also encounter transient non-diabetic hyperglycaemia. All situations where there are elevated levels of catecholamines, glucocorticoids and other stress hormones lead to it, including a number of acute diseases. A change in the regulation of glucose metabolism leading to hyperglycemia also accompanies inflammatory conditions. Hyperglycemia can also be induced iatrogenically, most often as a result of treatment with steroid hormones and their analogues.
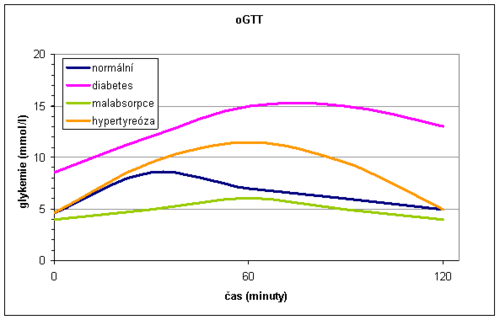
Oral glucose tolerance test[edit | edit source]
The oral glucose tolerance test (OGTT) reflects the body's response to glucose in a physiological way and assesses whether the body is able to maintain blood glucose levels within the normal range after glucose exposure. It is a summary of information not only about the effects of hormones regulating glycemia, but also about processes in the gastrointestinal tract (rate of gastric emptying, intestinal passage and resorption) and liver function.
The oral glucose tolerance test is used primarily for the early diagnosis of gestational diabetes. In this case, it is used as a routine screening examination, performed on all pregnant women at the turn of the second and third trimesters (at high risk, in addition, as soon as possible after pregnancy).
In others, the oral glucose tolerance test is recommended as an additional diagnostic test for the diagnosis of DM if fasting and random glucose values cannot be determined (especially if fasting blood glucose is between 5.6 - 7.0 mmol/l). If fasting or random blood glucose levels are conclusive for the diagnosis of DM, OGTT would be an unnecessary burden for the patient and is therefore contraindicated. Furthermore, it is not performed in acutely ill and immobilized patients or in patients on a reduction diet.
Performing an oral glucose tolerance test[edit | edit source]
- 3 days before the test we do not limit the intake of carbohydrates (at least 150 g/day) and the patient performs the usual physical effort
- after fasting for 8-14 hours, a fasting blood sample is taken;
- the patient drinks 75 g of glucose dissolved in 250-300 ml of tea or water within 5-10 minutes;
- the patient remains seated and does not smoke during the examination;
- another blood sample is taken from pregnant women at 60 and 120 minutes, from all other patients only at 120 minutes after glucose exposure.
In addition to the above-mentioned oGTT method, an even more detailed so-called glycemic curve can be performed, where blood is taken several times, usually at 30-minute intervals.
During the glycemic curve we can describe three sections:
- Glucose administration orally absorbed in the intestine and blood glucose increases - the rising part of the glycemic curve. It is usually steep after gastrectomy and flat during malabsorption. As the blood glucose increases, the oxidation of glucose in the muscles is stimulated and glycogen is formed in the liver.
- The function of the liver and the effects of insulin in the liver are reflected by another - the peak part of the glycemic curve. In the onset of DM , glucose in the liver is not sufficiently converted to glycogen, and therefore the peak of the glycemic curve exceeds 11.1 mmol/l and the maximum occurs later than in 60 minutes. In liver disease , the apex of the curve is also altered. Hepatocytes are not enough to metabolize the absorbed glucose, so more glucose passes into the periphery. The peak also exceeds 11.1 mmol/l and the increase persists for more than 60 minutes, but unlike DM, it returns to normal at 120 minutes (bell shape of the curve). In hyperthyroidism, the level of 11.1 mmol/l is also exceeded due to rapid absorption, but the decrease is rapid (gothic curve shape).
- The descending part of the glycemic curve is dependent on the effects of insulin and is physiologically characterized by a decrease in glucose levels. A slow and insufficient return of blood glucose to normal is a classic manifestation of DM
Normally, we observe a maximum rise in 30-60 minutes, there is no glycosuria and after 2 hours the blood glucose returns to fasting values.
In general, the oGTT is burdened with a large random error and low reproducibility.
Evaluation of blood glucose and OGTT[edit | edit source]
Healthy individuals have fasting plasma glucose <5.6 mmol/l, with oGTT having a fasting blood glucose <7.8 mmol/l at 120 minutes. It testifies to the diagnosis of DM:
- fasting blood glucose> 7.0 mmol / l
or
- random blood glucose> 11.1 mmol / l
or
- glycemia> 11.1 mmol / l at 120 minutes OGTT
together with classic clinical symptoms (thirst, polyuria, weight loss).
To confirm the diagnosis of DM, a re-examination from the next collection on one of the following days is required.
Glycated hemoglobin[edit | edit source]
Glycated haemoglobin is formed by a non-enzymatic reaction between haemoglobins and glucose in the blood. Jeho tvorba je ireverzibilní. Princip neenzymové glykace proteinů Therefore, the glycated hemoglobin level reflects the blood glucose concentration throughout the erythrocytes lifetime, i.e. about 120 days, and is used to assess the success of treatment/compensation of diabetes in the 4-8 weeks prior to the examination. Most commonly, the stable fraction form of HBA1c is determined.
- Terminology
- Glycated hemoglobin - the sum of the carbohydrate adducts at the N-terminal end or ε amino groups of lysineu in hemoglobin.
- HbA1 - the sum of the various minor fractions of hemoglobin (glycated), including HbA1c, HbA1a1/a2, HbA1b1/b2/b3, HbA1d1/d2/d3, and HbA1e.
- HbA1c - the glucose adduct valineu at the N-terminal end of β-globin; corresponds to the so-called stable ketoamine (N-[1-deoxyfructosyl]hemoglobin).
Glycated haemoglobin can be determined by ion-exchange chromatography followed by spectrophotometry. The amount of glycated haemoglobin is expressed in % of total haemoglobin or now in mmol/mol according to the IFCC (International Federation of Clinical Chemistry).
- Reference limits
- in healthy adults up to 39 mmol/mol, (2.8-4.0%)
Links[edit | edit source]
- Doporučený postup. Diabetes mellitus - laboratorní diagnostika a sledování stavu pacientů. 2015. Dostupné také z URL <http://www.cskb.cz/res/file/doporuceni/DM/DM_dop_201601.pdf>.
- ↑ Doporučený postup. Dooručené diagnostické a terapeutické postupy pro všeobecné praktické lékaře. 20ěé. Dostupné také z URL <https://www.svl.cz/files/files/Doporucene-postupy/2020/DIABETES-MELLITUS-2020.pdf>.
Related articles[edit | edit source]
- Glycaemia determination
- The blood glucose assessment is discussed together with the assessment of oGTT
- Hepatogennous diabetes