Congenital developmental defects
Congenital developmental defects are deviations from the normal prenatal development of the fetus that exceed the level of variability of the general population and can be pathological for their carrier. Disruption can be both at the structural and functional level. The basis is abnormal ontogenetic development , the cause of which can be genetic, environmental or multifactorial factors.
Clinical severity depends on the type, character, extent, and localization of the defect (from cosmetic deviations to conditions incompatible with life).
History[edit | edit source]
Congenital developmental defect is a phenomenon that has accompanied humanity since its beginnings. Skeletal findings bring us evidence of the occurrence of structural congenital defects from times when there was no question of any industrial pollution of the environment. Congenital developmental defects should therefore be viewed as undesirable but naturally occurring abnormalities in the development of a human individual.
Already from antiquity and the Middle Ages, some records have been preserved about individuals with a congenital defect and their often unhappy fate. The example of the Greek state of Sparta, where infanticide of affected individuals was officially carried out, is well known. These were actually negative eugenic measures in practice; in addition to Sparta, other ancient states also applied them. In medieval Europe, birth defects were often explained by the action of demonic forces, which sometimes had unfortunate consequences not only for the affected child, but also for the mother. In the modern age, with the development of medical sciences (especially embryology), the view of the causes and consequences of birth defects began to change fundamentally.
In the twentieth century, the cause of a number of birth defects was clarified and general risk factors were identified. Down's syndrome was described by the English pediatrician John Langdon Down as early as 1866, but it was not until 1959 that the French geneticist and pediatrician Jérôme Lejeune identified an extra chromosome 21 as the cause of this syndrome . ". In connection with the use of thalidomide (originally directly recommended for morning sickness, headaches etc.) to pregnant women at the turn of the 1950s and 1960s, at least 6,000 children with serious birth defects (mostly limb defects , typically of the phocomelia type - as part of the so-called thalidomide syndrome) were born worldwide. Thanks to the rapid development of genetics and the mapping of the human genome , a number of genes causing monogenic congenital defects (such as achondroplasia) have been discovered to date .
The topics of congenital developmental defects, their prenatal diagnosis and the overall approach to born and unborn disabled individuals are still very problematic, not only from a medical and social point of view, but especially from an ethical point of view .
Distribution of birth defects[edit | edit source]
- According to the mechanism of formation:
- Malformation – abnormal development of an organ/tissue from the beginning of pregnancy ( heart defects , spina bifida, polydactyly, clefts).
- Disruption – pathological disruption of the normal development of the organ/tissue (malformation of the limbs caused by amniotic bands – wrapping, strangulation of the limb as a result of amniocentesis).
- Deformation – mechanical damage to a hitherto healthy organ/tissue (pes equinovarus with lack of amniotic fluid).
- Dysplasia – abnormal arrangement of cells forming the relevant organ/tissue (osteogenesis imperfecta, kidney dysplasia).
- By frequency and complexity:
- Isolated defects – not associated with other defects or anomalies (isolated polydactyly).
- Sequence - the result of a pathologically initiated cascade of events (Potter's sequence, or the so-called oligohydramnial sequence, in agenesis of the kidneys, the lack of amniotic fluid leads to facial deformation due to the pressure of the uterine walls and hypoplasia of the lungs - they cannot develop properly without enough amniotic fluid).
- Association - development together with other defects (VACTERL/ VATER association from English vertebral defects, anal atresia, cardiac defects, tracheo-esophageal fistula, renal anomalies, and limb abnormalities ).
- Syndrome – is a complex of phenotypic features (anomalies) that are typical for a defined clinical diagnosis (Down syndrome).
Causes of birth defects[edit | edit source]
The causes of congenital developmental defects can be different. In general, it can be said that genetic factors, environmental factors and a combination of both groups of factors can contribute to abnormal prenatal development and the development of congenital developmental defects. The exact cause of many types of birth defects remains unknown even today.
Genetic causes[edit | edit source]
- Chromosomal aberrations
- They represent a specific group of diagnoses that are classified under the ICD-10 classification as congenital developmental defects. They are caused by structural or numerical deviations in the karyotype and often manifest themselves in a complex manner - as syndromes (for example, Down's syndrome, Edward's syndrome, Patau's syndrome, Turner's syndrome, etc.).
- Monogenic congenital defects
- Caused by a mutation in a single gene . This includes, for example, some significant congenital defects of the skeleton and connective tissue, such as achondroplasia or Marfan syndrome . A certain advantage in this case is the possibility of targeted molecular-genetic diagnostics in order to verify the diagnosis (even as part of prenatal diagnostics).
- Multifactorial birth defects
- They represent a very large group, which etiologically stands at the interface between defects caused by genetics and defects caused by external factors. In the case of multifactorial congenital developmental defects, both groups of factors apply.
External factors (teratogens)[edit | edit source]
External factors that are able to cause the emergence of a congenital developmental defect, or significantly increase the risk of such a defect, are generally referred to as teratogens. Similar to mutagens, teratogens can be divided into three main groups:
- Biological
- This includes, in particular, various causative agents of infectious diseases. Proven teratogens include viruses ( Rubivirus ( rubella ), Cytomegalovirus , Herpesviruses , Parvovirus B-19 , influenza virus, HIV , etc.), bacteria ( Treponema pallidum ( syphilis ), but also, for example, the protozoan Toxoplasma gondii ( toxoplasmosis ).
- Chemical
- Teratogens of a chemical nature include a number of chemical substances used in industry or agriculture (organic solvents, polychlorinated biphenyls, heavy metals, etc.). Medicines and medicinal preparations are an important group .
- Significant teratogens include cytostatics (e.g. the no longer used Aminopterin ), some antibiotics (especially tetracyclines), antiepileptics (phenytoin, valproate), lithium, warfarin , thalidomide , ACE-inhibitors, substances of a steroidal nature, retinoids, etc.
- Alcohol (ethyl alcohol, the abuse of which during pregnancy causes fetal alcohol syndrome) and some other drugs (pervitin, etc.) are also significant teratogens . Other diseases of the mother can also be dangerous - for example, diabetes mellitus, phenylketonuria, myasthenia gravis and others.
- Physical
- This group mainly includes various types of ionizing radiation (X-ray radiation, gamma radiation, etc.), as well as high temperature and mechanical teratogens (e.g. amputation of limbs with amniotic strips).
** See the Teratogens page for more detailed information .
Prenatal diagnosis[edit | edit source]
Prenatal diagnostics includes a set of procedures and methods used in the diagnosis of an unborn human individual. Developmental defects are probably the most significant group of diagnoses that can be diagnosed prenatally. Screening programs for pregnant women are used for the early detection of birth defects .
Early diagnosis of VV will make it possible to adjust prenatal, perinatal and postnatal care, which leads to complete or significant correction ( caesarean section , early surgical intervention). Rarely, prenatal therapy of the fetus is also possible (for example, in the case of obstructive developmental defects of the urinary system).
In the case of serious or incompatible developmental defects, in many countries of the world, in accordance with current legislation, it is possible to terminate the pregnancy prematurely and thus kill the fetus (artificial termination of pregnancy for genetic reasons is currently legal in the Czech Republic up to the 24th week of pregnancy).
Non-invasive[edit | edit source]
This includes non-invasive methods, used mainly in screening programs. The relevant methods are generally safe and non-burdensome for both the mother and the fetus.
First of all, it is a biochemical examination of specific markers (according to the timing and the markers used, we distinguish between first-trimester and second-trimester screening), which is actually a semi-invasive examination (requires sampling of the mother's peripheral blood). It is also an ultrasound examination that can be performed as part of a screening for congenital developmental defects (combined first-trimester screening) or targeted (for example, a targeted fetal echocardiographic examination in case of suspected developmental heart defects).
Invasive[edit | edit source]
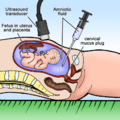
These methods are used in a targeted manner, with an increased risk of a certain birth defect. The methods are invasive, so they are relatively more risky for the mother and the fetus . The most commonly performed methods include amniocentesis , chorionic villus sampling , and cordocentesis . Using these methods, it is possible to obtain a sample of fetal tissue for cytogenetic or molecular-genetic examination.
For historical reasons, it is possible to mention fetoscopy , during which the fetus in the womb can be directly examined (today, fetoscopy is practically not used at all).
** More detailed information can be found on the page Prenatal diagnosis .
Examples of birth defects[edit | edit source]
Congenital defects by organ system[edit | edit source]
- Cleft defects ( facial clefts • cleft neural tube defects ).
- Congenital defects of the nervous system .
- Congenital defects of the respiratory system .
- Congenital heart defects .
- Congenital defects of the gastrointestinal tract .
- Congenital defects of the urinary system .
- Congenital defects of the genital organs ( developmental defects of the uterus and vagina • cryptorchidism ).
- Congenital defects of limbs .
Chromosomal aberrations[edit | edit source]
** See the Chromosomal Aberrations page for more detailed information .
Mitochondrially inherited defects[edit | edit source]
They arise from mtDNA mutation (transmission from the mother), great phenotypic variability due to multiple mitochondrial genotypes.
The most well-known is the MELAS syndrome (Myopathy, Encephalopathy, Lactic Acid, Stroke).
Monitoring systems[edit | edit source]
The field that deals with the incidence of birth defects in the population and its trends is called population teratology. In the second half of the twentieth century, the first epidemiological programs aimed at monitoring the incidence of birth defects in the population began to emerge. It was also the infamous thalidomide affair that drew attention to the need for such monitoring, which is able to quickly record changes in the incidence of birth defects. The first registries were mostly created in larger hospital facilities or within some universities.
The first population registers appeared , which covered the occurrence of VVV in the entire territory of the respective state (Czechoslovakia was one of the first states). Mandatory, nationwide and regular registration was started here in 1964 . Thanks to the involvement of the National Register of Birth Defects of the Czech Republic in international structures, these data are also available in an international comparison.
Links[edit | edit source]
[edit | edit source]
References[edit | edit source]
- ŠÍPEK, Antonín. Vrozené vývojové vady [online]. ©2008-2010. [cit. 2009-06-03]. <http://www.vrozene-vady.cz/>.
External Links[edit | edit source]
- MKN-10 klasifikace: VROZENÉ VADY‚ DEFORMACE A CHROMOZOMÁLNÍ ABNORMALITY (Q00–Q99)
- Národní registr vrozených vad (Institute of Health Information and Statistics of the Czech Republic)
- ICBDSR (International Clearinghouse for Birth Defects Surveillance and Research)
- EUROCAT (European Surveillance of Congenital Anomalies)