Hemorrhagic disease of the newborn
Hemorrhagic disease of the newborn (morbus hemorrhagicus neonatorum) is a disease caused by a deficiency of vitamin K, which is manifested by spontaneous bleeding. As a result of vitamin K deficiency, there is a decreased activity of vitamin K dependent coagulation factors II, VII, IX, X, protein C and [[protein S|S] ]. Vitamin K is key to the activation (γ-carboxylation) of these proteins. The level of these factors in a newborn reaches 30% of the adult level. Vitamin K does not pass well through the placenta, its reserves after birth are not sufficient. Breast milk contains low levels of vitamin K, and the formation of vitamin K by intestinal bacteria is absent in newborns. [1][2][3] With a lack of vitamin K, ineffective precursors of coagulation factors, the so-called PIVKA (proteins induced by vitamin K absence), with impaired coagulation function are formed in hepatocytes.[4]
Risk factors for bleeding disease[edit | edit source]
- exclusive breastfeeding (mother's milk contains significantly less vitamin K than cow's milk, the intestinal flora of breastfed children produces less vitamin K);
- medications given to the mother before delivery (anticonvulsants etc.);
- prematurity (due to the immaturity of the liver, they are more prone to bleeding);
- liver damage (hepatitis), biliary atresia, malabsorption syndrome, cystic fibrosis, diarrhea, celiac disease, alpha1- antitrypsin|alpha1-antitrypsin deficiency]], short bowel syndrome, bacterial overgrowth syndrome, chronic exposure to broad-spectrum antibiotics.[1][2][5]
Sources of Vitamin K[edit | edit source]
- External: food – the presence of fats and bile acids is necessary for resorption,
- internal: by synthesis by intestinal bacteria (synthesis decreases with administration of ATB)[2].
Clinical symptoms[edit | edit source]
GIT bleeding, skin, navel, punctures, nose, hematuria, later CNS bleeding. Forms:
- according to O. Hrodka and J. Vavřince, Pediatrics (2002):
- early' (0-24 hours) - the least frequent form, severe bleeding including bleeding into the digestive tract and intracranial bleeding, occurs with severe vitamin K deficiency in utero, for example due to drugs administered to the mother before delivery (antiepileptic drugs (phenobarbital, phenytoin), antitubercular drugs (e.g. rifampicin, isoniazid), barbiturates, salicylates, coumarin preparations, ATB, CHT), vitamin K can be given prophylactically to the mother at the end of pregnancy;
- classical' (2nd-7th day) - in newborns who were not given prophylactic vitamin K after birth, it manifests as bleeding from the navel, gastrointestinal tract (melena), skin, nose, surgical sites (e.g. . after circumcision), there is no bleeding into the CNS[6];
- late (1st-6th month) - most often between the 2nd and 8th week of life, the first manifestation is a sudden bleeding into the CNS in an otherwise healthy breastfed full-term newborn or in children with liver disease (e.g. . with biliary atresia) or malabsorption, can have fatal consequences.[2][3]
- according to A. C. Muntau, Pediatrics (2009):
- early form (2-5 days of life): hematemesis, melena, nose and navel bleeding;
- late form (3-7 days of life): acute life-threatening CNS hemorrhage in fully breastfed neonates - 20% lethality[1].
Diagnosis[edit | edit source]
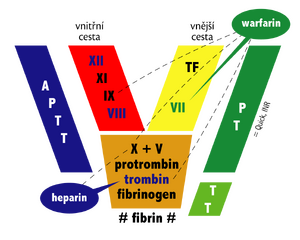
Coagulation parameters: prolonged prothrombin time' (Quick, INR) with normal level of platelets and fibrinogenu, in severe cases also prolongation of aPTT. The diagnosis is confirmed by the normalization of PT after administration of vitamin K. Alternatively, the diagnosis can be confirmed by examination of the level of vitamin K-dependent factors and PIVKA II, the inactive form of factor II (decarboxyprothrombin).[1][3]
Therapy[edit | edit source]
According to the severity of bleeding. Vitamin K (Kanavit inj.) – 1 mg i.v. or i.m. - the level of active vitamin-K dependent factors is adjusted within hours. In severe bleeding, fresh frozen plasma is also given along with vitamin K.[3]
Risk of nuclear icterus due to reduced binding capacity of albumin for bilirubin.[1]
Prevention[edit | edit source]
In full-term newborns:
- 1 mg i.m. (Kanavit® 1 mg = 0.1 ml) or
- 2 mg p.o. (1 drop = 1 mg), in fully breast-fed infants it is necessary to repeat 1 mg p.o. once a week. until 10-12 weeks of age.[7]
Vitamin K[edit | edit source]
Vitamin K is a group of lipophilic and hydrophobic vitamins. The name vitamin K is derived from the German term koagulations-vitamin. There are 3 known forms of vitamin K:
- K1 (phylloquinone) is found in green leafy vegetables, legumes, soybeans, vegetable oils and dairy products. Vitamin K given prophylactically to newborns after birth is vitamin K1.
- K2 (menaquinone) is formed by intestinal flora (especially Bacteroides species; on the other hand, Lactobacilli, which colonize the intestines of breast-fed children, do not produce vitamin K).
- K3 (menadione) is a synthetic, water-soluble form that is no longer used in medicine because of the potential risk of hemolytic anemia.
Vitamin K is an essential cofactor of γ-glutamyl carboxylase enzymatic activity, which catalyzes the γ-carboxylation of some proteins (so-called Gla-proteins) - coagulation factors II, VII, IX and X, protein C, protein S, protein Z.
With a lack of vitamin K, there is an increased level of abnormal prothrombin (so-called PIVKA II), which is not involved in the formation of a blood clot. It is a protein with impaired function (des-carboxylated prothrombin), which is unable to bind calcium and phospholipids.[8]
Links[edit | edit source]
Related Articles[edit | edit source]
References[edit | edit source]
- ↑ a b c d e MUNTAU,. Pediatrics. 4. edition. Grada, 2009. pp. 24. ISBN 978-80-247-2525-3.
- ↑ a b c d HRODEK, Otto – VAVŘINEC,. Pediatrics. 1. edition. Galén, 2002. pp. 78. ISBN 80-7262-178-5.
- ↑ a b c d RENNIE, JM, et al. Textbook of Neonatology. 5. edition. Churchill Livingstone Elsevier, 2012. pp. 777. ISBN 978-0-7020-3479-4.
- ↑ HAVRÁNEK, Jiří: ' 'Hematology. (edited)
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedNimavat - ↑ Pichler E, Pichler L. The neonatal coagulation system and the vitamin K deficiency bleeding - a mini review. Wien Med Wochenschr. 2008. 158(13-14):385-95.
- ↑ Czech Neonatology Society of the Czech Medical Society J.E. Purkyně. Prevention of Vitamin K Deficiency Bleeding (Bleeding Diseases of Newborns) : Recommended Practices in Neonatology [online]. ©2010. [cit. 2010-10-26]. <http://www.neonatologie.cz/fileadmin/user_upload/Doporuceni_CNEOS/Vitamin_K_2010.pdf>.
- ↑ name="Nimavat">NIMAVAT, D J. Vitamin K Deficiency Bleeding [online]. Medscape, ©2019. [cit. 2020-09-19]. <https://emedicine.medscape.com/article/974489-overview>.