Energy storage in the human body - glycogen metabolism and the formation of fatty acids and triacylglycerols
Subchapter content[edit | edit source]
- Introduction to energy storage in the human body
- Glycogen metabolism
- Formation of fatty acids and triacylglycerols
Introduction to energy storage in the human body[edit | edit source]
Energy in the human body is mainly stored in two storage substances - triacylglycerols (TAG) and glycogen. TAGs are more convenient for storage. The complete oxidation of 1 g of TAG yields approximately 38 kJ (9 kcal), from 1 g of carbohydrates or proteins only 17 kJ (4.1 kcal). During starvation, some plasma proteins (e.g. albumin ) and also muscle proteins are broken down first .
- 400,000 kJ in TAG (about 10.5 kg, about 15% of body weight)
- 100,000 kJ in protein (muscle)
- 8,000 kJ in glycogen (2,500 kJ in liver glycogen and more than twice that in muscle glycogen)
- 170 kJ in glucose
- If we calculate that our body consumes approximately 2,000 kcal per day, the reserves of liver glycogen and glucose would be enough for a maximum of one day. But TAG can cover these claims for weeks.
Glycogen Metabolism[edit | edit source]
Glycogen is a branched homopolymer of glucose molecules . Most of the glucose residues are linked by α 1→4 linkages. Every twelfth glucose residue is connected to the next residue by means of an α 1→6 bond – a branching point of the glycogen molecule is created. These branches are extended by additional glucose residues connected by α 1→4 linkages. This creates insoluble glycogen molecules resembling tree branches in their structure. All reactions during glycogen metabolism take place only at the non-reducing ends of its molecule - these can be shortened or lengthened.
Glycogen function[edit | edit source]
In animals, glycogen serves as a storehouse of carbohydrates, from which glucose esters can be released by cleavage. Richly hydrated glycogen granules are found in the cytoplasm of all cells. The human body can store approximately 450 g of glycogen. Of this amount, 80-100 g is found in the liver - the so-called liver glycogen , which is used to maintain a constant level of glucose in the blood (glycemia). Another 300 g is in muscle cells - so-called muscle glycogen. It serves rather as an internal muscle energy reserve during muscle work. Muscle cells do not contain glucose-6-phosphatase, and therefore the muscles cannot release pure glucose into the bloodstream. The rest (about 50 g of glycogen) goes to other cells of the human body.
Glycogen as an energy store[edit | edit source]
As mentioned above, glycogen is not the body's main energy store (liver glycogen is depleted within 12-24 hours of starvation). This is because it is a polar, richly hydrated molecule, and the bound water only "takes up space" and does not bring energy gain. The energy supply in adipose tissue is much more economical – because it is not hydrated (TAGs have a hydrophobic character) and at the same time fatty acids are formed by a more reduced carbon skeleton −CH 2 − compared to carbohydrates −CH(OH)−. By oxidizing them, a larger amount of energy is released. However, glycogen represents a storehouse of glucose, which is important, for example, for glucose-dependent cells (e.g. brain, erythrocytes).
Histochemical evidence[edit | edit source]
In histochemistry, its presence is proven by the so-called PAS-reaction (oxidation of two adjacent hydroxyl groups with periodic acid and subsequent reaction of the aldehyde groups formed in this way with Schiff's reagent).
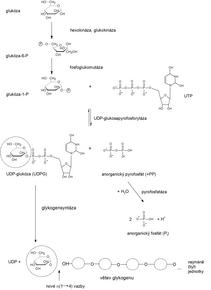
Glycogenesis (synthesis of glycogen)[edit | edit source]
The process of glycogen synthesis takes place in the cytosol . It is intense mainly in the liver and skeletal muscle. Glycogen synthesis is based on glucose molecules and additionally requires a so-called primer – i.e. a molecule that contains a chain of several glucoses connected by glycosidic bonds (most often it is the rest of the glycogen present in the cell, or the protein glycogenin ).
Progress[edit | edit source]
1. Phosphorylation of glucose to Glc-6-P
- in the liver, this reaction is catalyzed by glucokinase,
- hexokinase in muscles .
2. Conversion of Glc-6-P to Glc-1-P
- using glucose phosphate isomerase.
3. Glc-1-P reacts with UTP
- catalyzed by UDP-glucose pyrophosphorylase,
UDP-Glc is formed , or the activated form of glucose (UDP binds to C1).
The formation of glycosidic bonds between glucose molecules is an endergonic process , thus requiring energy-rich substrates. The transfer of glucose residues from UDP-Glc is direct (ΔG < 0).
4. UDP-Glc with its C1 attaches to C4 of the non-reducing end of glycogen
- catalyzed by the enzyme glycogen synthase, and at the same time releases UDP.
Thus, an α 1→4 bond O-glycosidic bond is formed.
5. Once the growing chain reaches a certain length (> 11 glucose residues), the molecule branches. An oligosaccharide graft consisting of 6–7 glucose residues is removed from the chain with the help of a branching enzyme (amylo-(1,4-1,6)-transglycosylase), which is then attached to the −OH group located at C6 of the glucose molecule located inside the glycogen chain – an α 1→6 bond is formed. These branches can be newly elongated by the action of glycogen synthase (see above).
Regulation of glycogen synthesis[edit | edit source]
Glycogen synthesis takes place at a time when the organism has a sufficient supply of energy substrates from food, i.e. it can create energy reserves for worse times. The main regulatory enzyme is glycogen synthase. Its activity is regulated by means of phosphorylation - if the enzyme is phosphorylated, it is inactivated, dephosphorylation, on the contrary, leads to the activation of the enzyme. Phosphorylation is influenced by the insulin/ glucagon ratio (e.g. through the intracellular concentration of cAMP) . Increasing the ratio activates glycogen synthesis (insulin is an anabolic hormone). A decrease in the ratio or catecholamines, on the contrary, inhibit it.
Glycogenolysis (degradation of glycogen)[edit | edit source]
Glycogen is never completely degraded, its degradation takes place in the cytosol of cells. This happens gradually in the form of so-called phosphorolytic splitting (phosphorolysis, binding of inorganic phosphate), when with the help of the enzyme glycogen phosphorylase (abbreviated phosphorylase), individual glucose monomer units are released from the non-reducing ends in the form of Glc-1-P - the so-called Cori ester. During the splitting of a glycogen molecule, phosphorylated glucose is produced directly, without the consumption of ATP :
N glucose residues + HPO 4 2- → Glc-1-P + (N−1) glucose residues
The richly branched glycogen molecule has many non-reducing ends, which is why glycogen is broken down quickly. At this point it is useful to mention that the breakdown of polysaccharides in the digestive tract takes place quite differently. Polysaccharides are first cleaved inside their chains to form shorter polysaccharides and oligosaccharides. Subsequently, free (not phosphorylated) glucose is released.
The course of glycogenolysis[edit | edit source]
1. Glycogen phosphorylase can only cleave α-1→4 glycosidic bonds. It starts cleaving glycogen from the non-reducing end and Glc-1-P is formed.
2. Glc-1-P is converted to Glc-6-P
- by the activity of phosphoglucomutase.
3. Breakdown of glycogen
- it stops at the 4th glucose residue before the branch point where the α 1→6 bond occurs.
4. The so-called debranching enzyme (glucanotransferase, transglycosidase
- separates a graft consisting of three glucose residues from the side chain and transfers it to the end of the linear (main) chain. There, it connects it using an α 1→4 bond.
5. At the point of the original branching, there is only one residue bound by an α 1→6 bond
- it is cleaved by the enzyme amylo-α1→6-glucosidase .
As a result, an unbranched chain is formed with the possibility of further cleavage by glycogen phosphorylase.
6. Glc-6-P is converted to glucose
- by glucose-6-phosphatase (catalyzes the cleavage of phosphate).
- This enzyme is found in liver and kidney cells and in enterocytes, where it binds to smooth endoplasmic reticulum membranes.
7. Glc-6-P
- it is transported to the ER by the enzyme translocase .
This separation into the ER serves to ensure that the resulting glucose is not immediately rephosphorylated to Glc-6-P.
8. Free glucose is then released into the blood, where it can serve as a source of energy.
Regulation of glycogenolysis[edit | edit source]
If the concentration of glucose in the blood falls, the insulin/glucagon ratio in the plasma decreases. Liver glycogen is broken down under these conditions. If the glycogen content in the liver decreases during starvation or under stressful conditions of the organism, glucose is synthesized de novo by gluconeogenesis reactions from non-sugar sources. The main regulatory enzyme of glycogenolysis is glycogen phosphorylase, one of those enzymes whose activity is regulated by covalent modification of the molecule. In this case, the phosphorylase is active phosphorylated.
- Activated phosphorylase is referred to as phosphorylase a.
- Inactive phosphorylase (does not have a phosphate group attached) is called phosphorylase b.
Phosphorylation of glycogen phosphorylase is catalyzed by the enzyme phosphorylase kinase, while dephosphorylation is catalyzed by protein phosphatases. Glycogenolysis is activated by counter-regulatory hormones – glucagon, catecholamines and glucocorticoids (e.g. cortisol), while insulin inhibits it.
In muscle cells, the regulation of glycogenolysis is also associated with a change in the concentration of Ca^{2+} ions. An increase in their intracellular concentration results in the activation of phosphorylase kinase and glycogen phosphorylase – activation of glycogenolysis. Mediators of their effect are the binding protein calmodulin and calmodulin-dependent protein kinases.
Clinical correlation[edit | edit source]
Congenital disorders of glycogen metabolism are called glycogenoses. In them, glycogen accumulates in cells (mainly in liver and muscle cells), which can result in a varied spectrum of symptoms - e.g. liver enlargement, hypoglycemia or developmental delay. Their incidence is approximately 1:10,000. The best-known type is type I – the so-called von Gierke's disease, when glucose-6-phosphatase is defective.
Summary of the regulation of glycogen metabolism[edit | edit source]
It clearly follows from the above that the regulation of both processes, glycogen synthesis and degradation, is contradictory. The individual effects are summarized in the following table.
| Regulatory enzyme | Activation | Inhibition |
|---|---|---|
| Glycogen phosphorylase
(glycogenolysis) |
Glucagon, adrenaline (phosphorylation),
reduction of ATP/AMP Ca2+ ratio (in muscle) |
Increase in ATP/AMP ratio insulin |
| Glycogen synthase
(glycogen synthesis) |
Insulin | Glucagon, adrenaline (phosphorylation) |
Formation of fatty acids and triacylglycerols[edit | edit source]
We perceive the formation of fatty acids and triacylglycerols as a highly energy-demanding process localized mainly in the cells of the liver, adipose tissue, CNS or lactating mammary gland. It takes place mainly in the postprandial period.
The process of fatty acid formation is in many ways the reverse of β-oxidation – instead of oxidation, reduction takes place, similarly, hydration is replaced by dehydration. However, it is not an exact reversal of events, the two processes differ in many significant ways. We will show these differences before describing the individual reactions.
Differences between the breakdown and synthesis of fatty acids
- Synthesis of MK takes place in the cytoplasm, degradation in the mitochondria matrix .
- Intermediate products of MK synthesis are bound to the so-called acyl carrier protein (ACP, acyl-carrying protein), intermediate products of degradation to the coenzyme A molecule .
- Enzymes of MK synthesis are combined into a multi-enzyme complex called MK synthase , degradation enzymes are stored freely in the matrix.
- The fatty acid chain is always lengthened by two carbon atoms - the initial substrate is AcCoA (the activated donor is malonyl~CoA).
- The reducing agent of synthesis is NADPH, the oxidizing agents of degradation are FAD and NAD + .
- Chain elongation at MK synthase ends with the formation of palmitate (C 16 ), further chain elongation and the formation of unsaturated acids takes place by the action of other enzymes in the ER and in the mitochondria.
Now we will look at the individual reactions of fatty acid synthesis.
Formation of malonyl~CoA[edit | edit source]
1. The input substance for the synthesis of fatty acids is AcCoA.
- In the first step, when ATP is consumed, it is carboxylated to malonyl-CoA :
- AcCoA + ATP + HCO – → malonyl~CoA + ADP + Pi + H+
- This reaction is catalyzed by the regulatory enzyme AcCoA-carboxylase, whose cofactor is biotin – vitamin H, or B 7 (in general, it is a cofactor of carboxylases).
- The formation of malonyl~CoA occurs in two steps. First, the ATP-dependent carboxylation of biotin takes place :
- Biotin-enzyme + ATP + HCO– → CO2 -biotin-enzyme + ADP + Pi
2. Subsequently, the carboxyl is transferred to acetyl-CoA
- CO 2 -biotin-enzyme + AcCoA → malonyl-CoA + biotin-enzyme
- Biotin is linked to the enzyme by an amide bond between the carboxyl of biotin and the ε-amino group of lysine. CO 2 is removed from the molecule again during condensation with the growing fatty acid chain.
Fatty acid synthase[edit | edit source]
Mammalian fatty acid synthase has a homodimer structure composed of two identical subunits (260 kDa). Each subunit consists of three domains connected by mobile regions:
- Domain 1 – substrate entry and condensation unit – both transferases (acetyltransferase and malonyltransferase) and β-ketoacyl synthase (condensation enzyme – CE).
- Domain 2 – the reducing unit – contains ACP, β-ketoacyl reductase, dehydratase and enoyl reductase.
- Domain 3 – palmitate-cleaving thioesterase.
The intermediate binding sites for MK synthase are:
- Thiol group of cysteine CE
- The thiol group of phosphopantetheine, which binds to the serine in ACP. The phosphopantetheine arm can also be found in the coenzyme A molecule. This flexible arm enables the transfer of intermediates between the individual catalytic sites of the synthase
Individual steps of fatty acid synthesis[edit | edit source]
1. Synthesis of malonyl-CoA
- catalyzed by acetyl-CoA carboxylase – does not take place on MK synthase
2. Binding of AcCoA to CE
- acetyl transacylase
3. Binding of malonyl-CoA to ACP
- malonyl transacylase
4. Condensation reaction
- condensing enzyme
5. MK synthase functions as a dimer.
- In this step, condensation occurs between the malonyl suspended on the ACP of one subunit and the acetyl on the condensing enzyme of the other subunit. The new acyl remains attached to the ACP:
- Acetyl-CE + malonyl-ACP → acetoacetyl-ACP + CE + CO2
6. First reduction
- β-ketoacyl reductase
Acetoacetyl-ACP + NADPH + H+ → D-3-hydroxybutyryl-ACP + NADP+
7. Dehydration
- 3-hydroxyacyl dehydratase
- D-3-Hydroxybutyryl-ACP → crotonyl-ACP + H2O
8. Second reduction
- enoyl reductase
- Crotonyl-ACP + NADPH + H+ → butyryl-ACP + NADP+
9. Chain transfer from ACP to the SH group of the condensing enzyme of the same subunit
10. The new malonyl binds to the ACP of the second subunit.
- Subsequently, condensation occurs on the opposite subunit of the dimer than it was during the first condensation. Thus, the subunits alternate regularly during synthesis.
Another MK synthesis procedure[edit | edit source]
The newly synthesized fatty acid chain is gradually lengthened. Termination occurs at the length of C 16 - the end product of MK synthase is therefore palmitate. Thioesterase cleaves it from the bond to ACP (hydrolysis of the thioester bond to phosphopantetheine).
In total, the formation of palmitate requires 8 molecules of AcCoA, 14 molecules of NADPH and 7 molecules of ATP:
8 AcCoA + 7 ATP + 14 NADPH + 14 H+ → palmitate + 14 NADP + + 8 CoA + 6 H2O + 7 ADP + 7 P i
AcCoA is produced in the mitochondrial matrix, MK synthesis takes place in the cytoplasm. However, the inner mitochondrial membrane is impermeable to AcCoA, so it is transported to the cytoplasm in the form of citrate (see below). 8 molecules of NADPH are obtained by transporting citrate into the cytoplasm, the remaining 6 in the pentose cycle.
Citrate as a carrier of acetyls from the mitochondrial matrix to the cytosol[edit | edit source]
If there is enough AcCoA in the mitochondrial matrix, it reacts with OAA to form citrate (catalyzes citrate synthase).
- It is transported to the cytoplasm, where it is cleaved by ATP-citrate lyase (ATP consumption):
- Citrate + ATP + HSCoA + H2O → AcCoA + ADP + Pi + OAA
Thus, AcCoA and OAA enter the cytosol together. AcCoA is used in the cytoplasm, whereas OAA must be returned to the matrix. What is his fate?
The inner membrane of the mitochondrion means an impermeable dam for him. OAA is therefore reduced with the participation of NADH to malate by cytosolic malate dehydrogenase :
- OAA + NADH + H+ → malate + NAD+
Malate is subsequently oxidatively decarboxylated by the NADP + -malate enzyme (the so-called malic enzyme ) to pyruvate:
- Malate + NADP+ → Pyr + CO2 + NADPH
Pyruvate can enter the mitochondrion, where it is carboxylated by pyruvate carboxylase:
- Pyruvate + CO2 + ATP + H2O → OAA + ADP + Pi + 2 H+
Summary transport equation:
- NADP+ + NADH + ATP + H2O → NADPH + NAD^+ + ADP + Pi + H+
Regulation of MK formation[edit | edit source]
The synthesis of fatty acids takes place in a situation where the body has enough substrates and enough energy. AcCoA-carboxylase plays a key regulatory role:
- Insulin stimulates MK synthesis by activating carboxylase.
- Citrate activates it - it means enough building units and energy.
- Glucagon and adrenaline have the opposite effect - they inhibit carboxylase (through its phosphorylation).
- Palmitoyl-CoA inhibits it - it is a product of MK synthesis, and if it is not removed, there is no need to create another - feedback inhibition.
- AMP inhibits it.
- Tip : Insulin stimulates MK synthesis by activating carboxylase - the synthesis of fatty acids takes place in a situation where the body has enough substrates and enough energy
Insulin signals the body to get rid of glucose at all costs. When glycolysis and glycogen formation are insufficient, excess glucose is converted to pyruvate, which is irreversibly changed to AcCoA by the pyruvate dehydrogenase reaction. Fatty acids are formed from this. Insulin also strengthens the activity of the pyruvate dehydrogenase complex.
Elongation and desaturation of fatty acids[edit | edit source]
MK synthase can only synthesize palmitate. Other MKs are synthesized by other enzymes. Chain lengthening (elongation) and the formation of unsaturated MKs (desaturation) takes place on the side of the ER membrane facing the cytosol and in the mitochondria.
A description of the exact course of elongation exceeds the scope of this text. We limit ourselves to noting that it is catalyzed by elongases.
Desaturases introduce double bonds into the MK chain (in the cis configuration). Mammals lack the enzymes catalyzing the entry of the double bond beyond C9 fatty acids. New double bonds are always introduced between an already existing double bond and a carboxyl group. Thus, mammals can not synthesize linoleic acid (18:2 cis Δ9, Δ12, belongs to ω-6 MK) or α-linolenic acid (18:3 cis Δ9, Δ12, Δ15, belongs to ω-3 MK) – both are essential. On the contrary, we can synthesize arachidonic acid (20:4 cis Δ5, Δ8, Δ11 and Δ14, ω-6 acid - it is formed by desaturation and elongation of linoleic acid), eicosapentaenoic acid (20:5 cis Δ5, Δ8, Δ11, Δ14 and Δ17, ω-3 – arises from linolenic acid) or docosahexaenoic acid (22:6 cis Δ4, Δ7, Δ10, Δ13, Δ16a Δ19, ω-3 – again arises from linolenic acid).
As an example, we can cite the formation of oleoyl-CoA (cis Δ9) from stearoyl-CoA:
Stearoyl-CoA + NADH + H+ + O2 → Oleoyl-CoA + NAD+ + 2 H2O
The description of the exact course is again beyond the scope of this text.
Synthesis of triacylglycerols[edit | edit source]
In order for the newly synthesized fatty acids to fulfill the role of energy reserves, they must first be converted into triacylglycerols. Similar to fatty acids, most TAG is formed in liver cells and adipocytes. Their synthesis requires activated glycerol – glycerol-3-P, and activated fatty acids. Formation takes place on the endoplasmic reticulum.
Glycerol-3-P is produced mainly by reduction of dihydroxyacetone phosphate, the reaction is catalyzed by glyceraldehyde-3-P-dehydrogenase. A second source may be glycerol released by lipolysis. The latter is activated by phosphorylation catalyzed by glycerol kinase. Glycerol-3-P is then gradually combined with two acyl-CoA molecules (catalyzed by acyltransferases), phosphatidic acid is formed. A phosphate group is cleaved from it to form 1,2-diacylglycerol, which is esterified with the help of the last molecule of acyl-CoA – triacylglycerol is formed. TAGs formed in the liver are transported to adipose tissue wrapped in VLDL lipoprotein particles.