Blood clotting examination
Blood clotting or haemocoagulation is the third stage of stopping bleeding. The first stage consists first of reflex, later humoral stimulation of vasoconstriction. In the second stage, platelet activation and adhesion and the formation of a primary (unstable) platelet thrombus occurs. The third stage then involves the activation of the plasma coagulation cascade and the formation of a fibrin network that stabilizes the thrombus.
Indications for blood coagulation tests[edit | edit source]
- Screening examination – before invasive procedures (surgery, biopsy, etc.);
- suspected bleeding or thrombophilic conditions;
- monitoring of anticoagulant treatment – Warfarin;
- an auxiliary indicator in the evaluation of hepatic proteosynthesis.
Procedure[edit | edit source]
Blood is drawn into a tube with EDTA or citrate. These substances have the ability to bind calcium to themselves (form a complex with it) and prevent immediate blood clotting. The blood is sent without delay to the laboratory, where the blood cell fraction is separated from the decalcified plasma by centrifugation. The required tests are then carried out, e.g. aPTT, PT = Quick test, fibrinogen level or D-dimers.
APTT[edit | edit source]
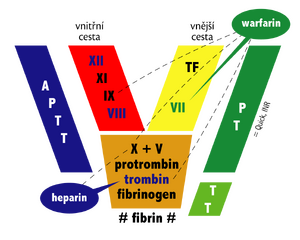
APTT (activated partial thromboplastin time) is a test of the intrinsic and common pathways of haemocoagulation.
Performance[edit | edit source]
At 37°C, kaolin-kephalin complex (kephalin, a phospholipid from rabbit brain) is added to decalcified plasma along with excess calcium ions. Here, kaolin represents the negatively charged surface activating the intrinsic pathway and kephalin functions as a partial thromboplastin(nothing to do with tissue thromboplastin!), i.e. actually a substitute for platelet phospholipid, necessary for factor X activation. This activates the intrinsic and then the common pathway. The time to fibrin clot formation is measured.
Physiological values[edit | edit source]
- 25,9–40 s[1]
- APTTR = value for comparison with the standard plasma parameter is in the range 0,83 - 1,3
- APTT depends primarily on the initial events of hemocoagulation in the intrinsic pathway (f. XII, XI, IX a VIII), as this part of coagulation proceeds more slowly. Only secondarily does it capture the efficiency of the common pathway factors, X, V, II and I.
Prolongation[edit | edit source]
- Haemophilia A (deficiency of f. VIII), haemophilia B (deficiency of f. IX), haemophilia C (deficiency of f. XI);
- treatment with i.v. heparin, but not with fractionated heparin s.c. - heparin increases the effectiveness of the physiological anticoagulant antithrombin III, which inhibits factors XII, XI, IX, X, II and VII. In addition to f. VII, all these changes are included in the APTT. Heparin also directly affects factor X activity;
- Warfarin treatment;
- von Willebrand disease – hereditary disorder of vW factor production, which carries factor VIII and thus affects its activity;
- Antiphospholipid syndrome – presence of antibodies to phospholipids;
- consumptive coagulopathy – DIC.
Quick's test[edit | edit source]
The Quick test, PT (prothrombin time) or TT (thromboplastin time), is a test of the external and common pathways. It indicates the rate of conversion of prothrombin to thrombin due to the action of tissue thromboplastin (coagulation factor III)
Performance[edit | edit source]
Tissue thromboplastin is added to decalcified plasma along with excess calcium ions. This activates the extrinsic and then the common pathway. The time to formation of the first fibrin clot is measured. The results of the test are usually given by the INR (international normalised ratio), i.e. the ratio of the patient's measured time to the normal value of the control plasma. Commercially supplied types of tissue thromboplastin (tissue factor III) differ from each other. Therefore, the potency factor of the thromboplastin used is added to the INR calculation equation.
Physiological values[edit | edit source]
- 12–15 s
- INR: 0,8–1,2 (80–120 %) [1]
The resultant time depends on the concentration of the individual coagulation factors of the external and common system. When blood clotting is increased, the INR is lower; when clotting is prolonged (e.g., during treatment with anti-Vitamin K), the INR increases.
Prolongation[edit | edit source]
- physiologically in newborns – factor VII deficiency;
- Warfarin therapy or other conditions with hypovitaminosis K;
- i.v.heparinem therapy;
- severe disorder of hepatic proteosynthesis;
- consumptive coagulopathy – DIC.
Other examinations[edit | edit source]
- Lee-White method
- A tentative method of examining coagulation at the patient's bedside that has minimal clinical use. The principle of the test involves spontaneous activation of the intrinsic coagulation cascade in vitro (in a test tube). The result depends on the state of the internal branch and the common coagulation system.
- The normal time is: 5–15 min at room temperature.
- Total fibrin degradation products
- FDP (fibrin degradation products) and D-dimers are specific for stabilized fibrin (norm below 160 μg/l).
- mmunological determination of fibrin degradation products monitors acute phase proteins. It is an indicator of activated fibrinolysis and from a diagnostic point of view, primarily a marker of recently initiated coagulation with subsequent fibrinolysis. It is mainly used in suspected thromboembolic disease. However, the high sensitivity of the method is at the expense of its specificity. It can also be used in monitoring treatment to induce thrombus dissolution in the patient.
- Fibrinogen concentration
- This is referred to as Fbg. It is the determination of the plasma fibrinogen concentration. The norm is between 1,5–4,5 g/l.
- Antithrombin III
- Determination of functional activity in plasma, normal range given by comparison with control plasma (70–100 %). Primary or secondary (consumption in DIC) deficiency of antithrombin III is a risk factor for thrombophilia.
- Thrombin time
- Thrombin time (TT) is a direct measurement of the conversion of Fbg to fibrin.
- Execution: thrombin added to decalcified plasma along with excess calcium. The time to fibrin clot formation is measured.
- The physiological range is 17–24 s.
- Prolonged in dysfibrinogenemia, severe hypo- or afibrinogenemia, activated fibrinolysis and heparin therapy.
- Euglobulin method of determining fibrinolytic activity
- A euglobulin fraction containing plasminogen is precipitated from plasma at the isoelectric point with acetic acid. The fraction is separated, dissolved and precipitated again with calcium chloride. The plasmin present, freed from the action of α2-antiplasmin by precipitation, lyses the resulting clot. When the fibrinolytic system is activated, more activated free plasmin is present and lysis of the clot is faster.
- The physiological lysis time is 120–240 minutes. Shorter times indicate increased activation of the fibrinolytic system.
- Activated coagulation time (ACT)
- Blood collected without anticoagulant is injected into a tube with contact activator (kaolin) and mixed in the machine at 37 °C until the coagulation time is read. Routine to check heparinization during extracorporeal circulation and hemodialysis. ACT of normal blood is about 150 s, for heparinization for long-term extracorporeal circulation or hemodialysis 180−300 s, for MO in cardiac surgery > 600 s.
- Other examinations
- examination Protein C, protein S, examination APC resistance (genetic resistance of factor V to activated protein C, a risk factor for thromboembolic disease);
- antiphospholipid antibody testing – llupus anticoagulants, modified aPTT, anticardiolipin antibodies;
- examination of the fibrinolytic system – plasminogen activators (tPA, uPA, PAI-1), plasminogen;
- examination of activity of individual factors of coagulation and fibrinolytic cascade – dg. e.g. haemophilia A, B, C.
Evaluation of haemostasis examination[edit | edit source]
| aPTT | PT (Quick) | Platelets | Bleeding time | Common causes |
|---|---|---|---|---|
| Vasculopathy, deficiency of f. XIII | ||||
| ↑ | Thrombocytopathia | |||
| ↓ | ↑ | Thrombocytopenia | ||
| ↑ | Heparin treatment, f. deficiency. VIII, IX, XI, XII | |||
| ↑ | Deficiency of f. VII | |||
| ↑ | ↑ | Warfarin treatment and other hypovitaminosis K | ||
| ↑ | ↑ | von Willebrand's disease | ||
| ↑ | ↑ | ↓ | ↑ | Impaired hepatic proteosynthesis, DIC (sepsis)
|
based on E. Lechler
Links[edit | edit source]
Related articles[edit | edit source]
Reference[edit | edit source]
- ↑ a b Maxdorf. Velký lékařský slovník On-line: Normální laboratorní hodnoty dospělých [online]. ©2008. [cit. 2010-02-28]. <http://lekarske.slovniky.cz/normalni-hodnoty>.