Yersinia
Yersinias are pathogenic to humans. Yersinia pestis and Yersinia pseudotuberculosis have ecological and genetic similarities, but epidemiological differences. Yersinia enterocolitica is found mainly in water, soil and the digestive tract of vertebrates.
Yersinia pestis[edit | edit source]
Yersinia pestis is G- bacteria and a major pathogen causing plague pandemics. It was first isolated by Alexander Yersin in 1894 in Hong Kong. Plague is associated with high mortality without antibacterial therapy. In the wild, Yersinia pestis was found in several rodent species. However, Yersinia pestis circulates through flea bites, in humans it is a rat flea bite. Bacteria get into the wound. Human-to-human transmission can occur via aerosol particles or droplet infection and a primary plague infection arise. Plague is rare at this time, occurring in Africa, India, Southeast Asia, Mexico, and the western United States.[1]
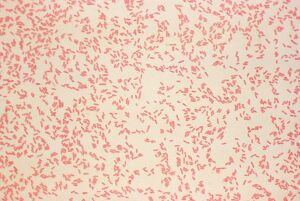
Morphology[edit | edit source]
Yersinia pestis is a pleomorphic rod-shaped bacterium with a capsule. It is a stationary stick. Other yersinias are mobile. A common feature of Y. pseudotuberculosis and Y. enterocolitica is that it stains polar. This rod, like all Enterobacteriaceae, is characterized by the ability to grow on simple laboratory soils. Their undemanding growth ranges from 0 to 40°C with a temperature optimum around 30°C.[2]
Antigenic structure[edit | edit source]
On its surface is a localized F1 protein complex, which is a protective antigen. O-specific side chains are not present. Virulent strains form V and W proteins, the production of which is linked to plasmids.
Pathogenicity[edit | edit source]
The pathogenicity of Yersinia pestis is determined by a complex of chromosome and plasmid-linked factors. Surface factors that block phagocytosis are important. Virulent strains of this bacterium are facultatively intracellular parasites that multiply in macrophages. During infection, Yersinia pestis, an facultative intracellular bacterium, exhibits the ability to first invade cells and then thwart phagocytosis of the host cell. During these two distinct phases, the invasion phase and the anti-phagocytic factor phase, the bacteria in manipulating the host cell help to complete each of these functions, but the mechanism by which Yersinia regulates these functions during each step remains unclear. In addition to macrophages, the bacterium is also able to penetrate epithelial cells. During the invasion at the site of injury, a hemorrhagic pustule is formed, from where the infection is further distributed to the descending lymph nodes, in which the subsequent enlargement produces smoke (bubonic form of the plague). Later, bacteremia and sepsis develop. A secondary disease, Pneumonia, may develop, causing Yersinia pestis to spread to the surrounding area by coughing up, and the infected person will develop primary pneumonia – a pulmonary form of the plague. When a patient manages to overcome the disease, he develops good immunity.
Diagnosis and therapy[edit | edit source]
Bacteria are diagnosed from the contents of the pustules, lymph nodes, blood culture, bone marrow, and sputum. Cultivation is possible on blood agar. Bacteria stain according to Gram negative. When testing Yersinia pestis for antibiotic susceptibility, the bacteria were found to be susceptible to chloramphenicol, streptomycin, kanamycin, tetracycline, quinolones. However, plague vaccines produced by Yersinia pestis are in clinical development. Streptomycin can be used in endemic areas. We can induce short-term immunity when a dead vaccine with a protective antigen is given. A live vaccine with live attenuated strains is more effective, but the use of this vaccine is only approved in some parts of the world. There is currently no licensed vaccine to prevent plague in Western Europe.
Yersinia enterocolitica[edit | edit source]
Yersinia enterocolitica is a G- non-sporulating, facultatively anaerobic straight rod. It is pathogenic to humans and is the cause of human yersiniosis. The disease is transmitted alimentary through infected raw pork. It is widespread cosmopolitanly. The prevention is to avoid consuming badly roasted pork, or to observe hygiene after contact with the meat. The disease can be treated with antibiotics.
Morphology[edit | edit source]
Yersinia enterocolitica is a gram-negative straight rod that is only mobile at lower temperatures. Its size is 0.3–1.0 μm and 1.0–6.0 μm. It can be grown on conventional cultivation soils because it is easy to grow. It has no problem growing in a low glucose environment at 28°C. It is recommended to use selective soils for culturing bacteria from faeces. The ideal pH for growth is in a wide range of 4.6-9 with an optimal pH of 7-8.
Epidemiology[edit | edit source]
Yersinia enterocolitica was discovered by Schleifstein and Coleman in year 1939 in the USA. It has been a well-known pathogen in the last four decades. It occurs mainly in food, especially in raw pork, but has no problem surviving on fruits and vegetables in the refrigerator at lower temperatures. Most Y. enterocolitica isolates recovered from natural samples, including houses where animals are slaughtered or in butchers. They were non-pathogenic in nature and in water. Bio serotypes 4/O:3 are the most common cause of human yersiniosis, food poisoning caused by Y. enterocolitica is known cosmopolitanly.
Pathogenicity and virulence[edit | edit source]
Virulence is bound on the chromosome and on the plasmid. It is given by the invasiveness and penetration of the microbe into the cell. Food can enter the terminal ileum and appendix, where it penetrates cells and lymphatic tissues to which it has a particularly high affinity. Virulent strains multiply in macrophages and induce granuloma formation. Non-virulent strains are eliminated without penetrating the cells.
Clinical picture[edit | edit source]
We observe clinical signs from mild diarrhea to serious complications such as liver abscesses and post-infectious extraintestinal consequences. The main reservoir is pigs, which are asymptomatic carriers.
Disease[edit | edit source]
Manifestations of the disease in humans are different in children and adults. Children develop fever and diarrhea, where blood may appear. Abdominal pain is also typical in the right lumbar pit. In adults, we observe gastrointestinal infections and diarrhea. With long-term illness, secondary complications can occur and these are inflammations of the joints. An unusual case of infection manifesting as perianal ulcers and colon ulcers has also been observed. An individual can become infected from infected pork. Toxic bacteria produce a thermostable toxin at 25°C in milk. However, at 4°C they will not produce significant amounts of this toxin.
Therapy[edit | edit source]
Bacteremia requires antibiotic treatment. Tetracycline is used. Tests have shown that bacteria have a high degree of resistance to ampicillin and cephalothin. In the diagnostic laboratory, examinations of the stool, nodes, and appendix are performed. Immunochromatic test for the quantitative determination of serotypes O3 and O9 in a stool sample with a result within 1 hour. The test is highly sensitive and specific.
Prevention[edit | edit source]
Prevention against Yersinia enterocolitica and Yersinia pseudotuberculosis is to avoid eating undercooked pork or drinking unpasteurized milk. After contact with raw pork, it is recommended to wash your hands thoroughly with soap.
Yersinia pseudotuberculosis[edit | edit source]
Yersinia pseudotuberculosis is a G−, facultatively anaerobic, pleomorphic rod capable of moving at lower temperatures. It is widespread cosmopolitanly. Alimentary, orofecal transmission from infected animals or food. Diseases are associated with gastrointestinal problems, fever, diarrhea. The best prevention is personal hygiene and avoiding contact with infected animals.
Morphology[edit | edit source]
Yersinia pseudotuberculosis je G−, pleomorphic rod. It is able to move at lower temperatures. This organism was described in 1889 as a disease of Guinea pigs. However, Yersinia pseudotuberculosis has emerged as the ancestor of Yersinia pestis, which was the cause of pandemic plague during the years 541-767.
You can find more information on the page Yersinia pestis.
Epidemiology[edit | edit source]
It is undemanding to cultivation, it is cultivated on common soils. It is widespread cosmopolitanly and has been isolated from several animal species such as cats, dogs, pigs, monkeys, and more. Y. pseudotuberculosis is widespread in the environment (feces, water), where it can survive for a long time. The environment itself is contaminated with the faeces of infected animals, especially rodents and birds. In addition to animals, it was also found in water, both in rivers and in alpine streams.
Antigenic structure[edit | edit source]
We can distinguish 5 serotypes according to somatic antigen.
Pathogenicity and virulence[edit | edit source]
The toxin bound in the cell is different from the plague toxin. Virulent strands can cause the septicemic form akin to the plague especially in individuals with a weakened immune system. Gastrointestinal tract diseases such as acute and chronic appendicitis, gastroenteritis, or disorders of mesenteric lymph nodes occur much more often. Infections with Y. pseudotuberculosis were reported all around the world. These infections happen less frequently than infections by Yersinia enterocolitica. Most of the infections are sporadic and arise rarely, e.g., outbreaks in Finland and Japan.
Clinical manifestations[edit | edit source]
The disease manifests itself in humans with fever, rashes, abdominal pain, and diarrhea. Yersinia pseudotuberculosis has been associated with Kawasaki disease.
Diagnostics[edit | edit source]
Laboratory tests are obtained from stool, urine, or blood tests for bacterial antibodies. Serotyping of an isolated strain. Antibiotics are used for treatment. We must not forget that the patient may be dehydrated due to fever and diarrhea. Rehydration of the patient is necessary.
Links[edit | edit source]
Related articles[edit | edit source]
References[edit | edit source]
References[edit | edit source]
- BEDNÁŘ, Marek – SOUČEK, Andrej – FRAŇKOVÁ, Věra, et al. Lékařská mikrobiologie : Bakteriologie, virologie, parazitologie. 1. edition. Praha : Marvil, 1999. 558 pp. ISBN 8023802976.
- JULÁK, Jaroslav. Úvod do lékařské bakteriologie. 1. edition. Praha : Karolinum, 2006. ISBN 80-246-1270-4.