Vulvitis
Vulvitis or inflammation of the external genital organs occurs more often in older women, in connection with damage to the superficial layers of the skin, or, on the contrary, in children with neglected hygiene. Normally the skin is very resistant to infection, but the problem arises when a woman is too obese or when the skin is repeatedly injured by scratching or macerated by urine, sweat, etc. Skin resistance also decreases in general metabolic disorders - diabetes mellitus, hepatopathy, anaemia, etc.
Clinical pattern[edit | edit source]
- Itching of the external genitalia, burning during and after urination - i.e. pseudodysuria, difficulties during sexual intercourse.
Bacterial vulvitis[edit | edit source]
- Folliculitis, furunculosis - self-limiting form;
- phlegmon - without boundries.
- On inspection we see reddened skin, which is sensitive to touch, warm, and swollen. When the hair follicles of the vulva become infected, the infection penetrates into the deeper layers, the so-called furuncles form. Furuncles often merge to form multiple purulent deposits, even phlegmon.
- The solid infiltrate gradually coagulates to form an abscess. We rarely see this condition today, but if we diagnose it, we must think about possible immune system disorders - AIDS - and we must rule out diabetes mellitus.
- If ulcerations occur, weshould think of syphilitic ulcer (ulcus molle), tuberculous ulcer (ulcus vulvae chronicum), lymphogranuloma venereum. Sometimes we can also see swollen plaques on the vulva - condylomata lata - representing the second stage of syphilis.
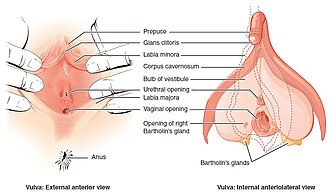
Inflammation of Bartholini's gland (Inflammatio glandulae vestibularis majoris seu Bartholini)[edit | edit source]
- Inflammation of a part or the whole gland;
- It begins with inflammation of the duct of the gland, swelling and obstruction of the duct, the contents stagnate, become infected and empyema develops; if left untreated, the inflammation spreads to the surrounding area and an abscess develops;
- retention cyst - chronic form, the process is usually unilateral, the thickened duct of the gland is clogged with thick mucus.
- Origins
- E. coli, Chlamydia trachomatis, Neisseria gonorrhoeae, streptococci, staphylococci.
- Clinical pattern
- Pain, swelling of the area, difficulty walking, fever, reddened skin, elevated CRP and leukocytes.
- Diagnostics
- Culture is necessary.
- Therapy
- In the beginning we provide conservative therapy - rest, compression, ATB, analgesics, in case of development of an empyema or abscess, surgical intervention is necessary - incision with drainage, chemical extirpation (we suction the contents of the cyst through the incision, then we insert 0.5 cm of AgNO3 (lapis) rods into the abscess cavity, we close the incision with a suture and within 48 h after removing the suture we pull out the wrinkled gland capsule).
Mycotic vulvitis[edit | edit source]
- Whitish plaques on the vulva, small epithelial defects, itching.
Viral vulvitis[edit | edit source]
Condylomata accuminata[edit | edit source]
- Warty growths caused by non-oncogenic papillomaviruses;
- the virus multiplies in the squamous epithelial cells, hence the growths are also found in the vagina and cervix.
Herpes simplex virus[edit | edit source]
- The disease manifests itself after 3-6 days of incubation by small blisters on the labia and in the vagina;
- possible bacterial superinfection;
- highly infectious fluid oozes after blister rupture.
- Diagnostics
- Bacteriological examination, parasitological examination of stool, biochemical, haematological examination.
- Therapy
- is determined by the results of the examination - application of anti-inflammatory drugs, antifungal drugs, ointment with corticosteroids, in more severe forms of herpetic infections acyclovir (administration of the drug must be as soon as possible after sowing). In papillomavirus infections, a 20% solution of podophyllotoxin or trichloroacetic acid is used. Recently imiquimod - causes local immunoreaction.
References[edit | edit source]
Related articles[edit | edit source]
- Causative agents of female genital tract infections
- Vulvovaginitis
- Non-cancerous diseases of the vagina
- Bacterial vaginosis
Used literature[edit | edit source]
- ROB, Lukáš, Alois MARTAN a Karel CITTERBART, et al. Gynekologie. 2. vydání. Praha : Galén, 2008. 343 s. s. 130–132. ISBN 978-80-7262-501-7.
Kategorie:Gynekologie
Kategorie:Porodnictví
Kategorie:Patologie
Kategorie:Mikrobiologie