Urinalysis/chemical
Commonly, urine is qualitatively measured for protein, glucose, hemoglobin, ketone bodies and bile dyes. These components are usually found in the urine of healthy persons, but in such small quantities that they cannot be demonstrated by conventional tests. Under various pathological conditions, their concentration in the urine increases.
Tube reactions
Chemické vyšetření moči mokrou cestou
Test (diagnostic) strips
The detection of pathological urine components at the bedside or in the line of first contact with the patient is possible by means of test strips.
Test strips consist of a plastic carrier on which one or more indication zones are fixed. They are produced by aspirating a liquid analytical reagent into a suitable material (e.g. special filter paper) and gently drying it.
Diagnostic strips are available as mono-functional, poly-functional or special examination strips.
Monofunctional strips contain basic indication zones for the semi-quantitative determination of a substance in urine. Polyfunctional strips consist of several indication zones, allowing the examination of several biochemical parameters at the same time. They are intended for cases where it is necessary to obtain as much information as possible about the patient's health status, e.g. during various screening events. In addition to monofunctional and polyfunctional strips, there are special test strips, which include combinations of two or more indication zones that are selected for the investigation of a specific disease, e.g. diabetes mellitus screening strips include a zone for the determination of glucose, ketone bodies, protein and pH.
With the help of test strips, the following parameters can be determined in the urine:
Principles of determination of individual parameters
Protein
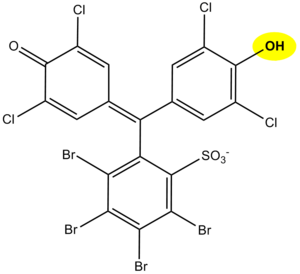
The principle of determination of proteins in urine using diagnostic strips is based on the so-called protein error of an acid-base indicator , eg tetrabromophenol blue , tetrabromophenolphthalein ethyl ester or 3´, 3´´, 5´, 5´´-tetrachlorophenol-3,4,5,6- tetrabromosulfophthalein. Like any acid-base indicator, these substances change color at a certain pH (they behave like weak acids, while the protonated form has a different color than the dissociated form): at pH below 3.5 they are yellow, at higher pH they are green to blue. In addition to the indicator, there is a buffer in the reaction zone of the test strip, which maintains the pH in the range of 3.0 to 3.5, so the indicator is yellow. If there are proteins in the sample, they bind to the indicator with their amino groups. However, this changes its properties - the transition area shifts towards a more acidic pH. This means that at the stated constant pH between 3.0 and 3.5, the protein-bound indicator will be green, as if it were in a more alkaline environment (hence the protein error of the indicator ).). The color intensity depends on the protein concentration, varies from green to blue and is evaluated visually or instrumentally.
In highly alkaline urine (pH above 8) or if the urine is very concentrated, the test may give false positive results (buffer will be depleted in the reaction zone). In these cases, acidify the urine with a few drops of dilute acetic acid to pH 5-6 and repeat the test. False positives can also be caused by high concentrations of some substances with amino groups (contamination of the sampling vessel with some disinfectants), which bind to the indicators similarly to proteins.
The disadvantage of the test strips is their different sensitivity to individual proteins. The strips react very well with albumin and indicate its presence in urine from 0.1 to 0.5 g / l. They are significantly less sensitive to globulins, glycoproteins and Bence-Jones protein . These diagnostic strips do not show an increase in albuminuria to values up to about 200 mg / l, resp. daily albumin losses in the range of 30 to 300 mg / 24 hours, which accompanies especially the earlier phases of some nephropathy. Immunochemical methods can be used to screen for increased albuminuria, such as special diagnostic strips based on immunochromatographic principles or immunoturbidimetry.
Hemoglobin
Hemoglobin catalyzes, like peroxidase, the oxidation (dehydrogenation) of some substrates (eg benzidine derivatives) with hydrogen peroxide:
However, it is not an enzyme activity (catalysis is conditioned by heme iron) and therefore it is not lost even after heat denaturation. We are talking about pseudoperoxidase activity, which is used for sensitive but non-specific evidence of hemoglobin or trace amounts of blood. It is preferable to use a chromogenic substrate to monitor the reaction, i.e., a substance that provides a markedly colored product by dehydrogenation (often benzidine or its non-carcinogenic derivatives, aminophenazone, etc.).
The reagent zone of the diagnostic strips contains a chromogen (eg tetramethylbenzidine) with stabilized hydrogen peroxide (eg cumene hydroperoxide). In the presence of free hemoglobin (hemoglobinuria), the indication zone turns uniformly blue. If erythrocytes are present in the urine (erythrocyturia), intensely green-blue dots to spots form.
Hemoglobinuria can be found in intravascular hemolysis. More damage to the glomerular membrane (glomerular hematuria) and bleeding from any part of the urinary tract lead to more frequent erythrocyturia. It is often found in urinary tract infections, urolithiasis and urogenital tract tumors.
In addition to hemoglobin, myoglobin also provides a pseudoperoxidase response, which can be excreted in the urine during skeletal muscle breakdown (rhabdomyolysis, crush-syndrome). The positivity of the test may also be due to peroxidases of leukocytes or certain bacteria, yeasts or fungi, which may occur in the urine, especially in urinary tract infections. To rule out the possibility of a false positive reaction due to cellular peroxidases, the reaction must be performed with boiled urine.
Contamination of the sampling vessel with strong oxidizing agents also causes a false positive reaction. On the other hand, the presence of strong reducing substances (eg ascorbic acid) can slow down or even stop the pseudoperoxidase reaction and thus cause false negative results.
Glucose
Diagnostic strips for the detection of glucose in urine are based on the principle of enzyme reactions with glucose oxidase and peroxidase (the same principle as glycemic determination). D-glucose is oxidized by oxygen using glucose oxidase to form D-glucono-1,5-lactone and hydrogen peroxide. In the subsequent peroxidase reaction, hydrogen peroxide oxidizes tetramethylbenzidine or another chromogen to color product. The light yellow color of the reaction surface changes to blue-green when positive. The test is specific for D-glucose, other sugars do not give a positive reaction.
High concentrations of reducing agents such as ascorbic acid slow color development and may lead to falsely lower results. In these cases, it is recommended to repeat the analysis at least 10 hours after stopping vitamin C. Conversely, false positive results may be caused by the presence of peroxidase substrates or oxidizing agents in the sampling container (e.g. H2O2, Persteril®, chloramine B). Urine glucose determination must be performed quickly to avoid bacterial contamination or urine stored at 4 °C.
Interference with ascorbic acid is a frequent source of false negatives. Diagnostic urine test strips from some manufacturers are therefore modified so that the reaction zone is at least to some extent resistant to ascorbic acid. Some diagnostic strips also have a detection zone for ascorbate to alert you to the possibility of a false negative.
Glucosuria is most often accompanied by a rise in glucose above the so-called renal glucose threshold (around 10 mmol/l). Glucose, which is normally filtered through the glomerular membrane, is in such high concentration in the primitive urine that it is not enough to be resorbed in the tubules and enters the final urine. Glucosuria with normal glycaemia is indicative of a defect in tubular transport mechanisms - we speak of renal glucosuria.
Urinary ketone bodies
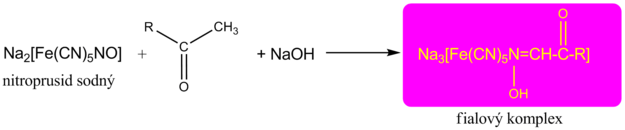
The detection of ketone bodies is based on the reactions of acetoacetic acid and acetone with sodium nitroprusside in an alkaline medium, which forms a red-violet-colored complex . This principle is used by Legal's and Lestradet's exams , as well as diagnostic strips. Β-hydroxybutyric acid (ie the most abundant ketone substance) does not provide a reaction and therefore a negative result does not completely rule out ketoacidosis.
Compounds with free sulfhydryl groups (eg the antihypertensive captopril or uroprotectant used in some mesna chemotherapeutic regimens ) provide false positivity for urinary ketone bodies . Quite often, bacterial products in urinary tract infections also provide a similar response.
False negatives , apart from the already mentioned insensitivity of the β-hydroxybutyric acid tests, are not significant.
See also Ketone bodies in urine.
Bilirubin
The determination of bilirubin in urine with paper chromatography is based on the Azo coupling reaction, which is provided by the conjugated bilirubin with a stable diazonium salt (e.g. 2,6-dichloride benzenediazonium tetrafluoroborate). The result is a pink/red color. with the simultanious presence of a high urobilinogen concentration the color changes to orange. In this case is recommended to evaluate the coloration after two minutes since the indication area was dipped. Lower or false negative results can be caused by a high concentration of ascorbic acid. Urine samples ought to be protected from direct sun rays, because they can provoke bilirubin's oxidation and consequently a false lower or negative finding.
In the urine is analyzed only the conjugated bilirubin as the unconjugated bilirubin cannot be expelled in it.
Urobilinogen
As with bilirubin, the principle of azocoupling reaction with a stable diazonium salt (eg 4-methoxybenzenediazonium tetrafluoroborate) is used to determine urobilinogen in urine . The indication zone turns pink to red in the presence of urobilinogen. The faint pink color still corresponds to the physiological excretion of urobilinogen. In the presence of bilirubin , the color is yellow, which turns green to blue after 1 minute.
Some heterocyclic nitrogenous substances produced by bacteria in urinary tract infections can cause false positives . High concentrations of ascorbate can cause false negatives .
Leukocytes
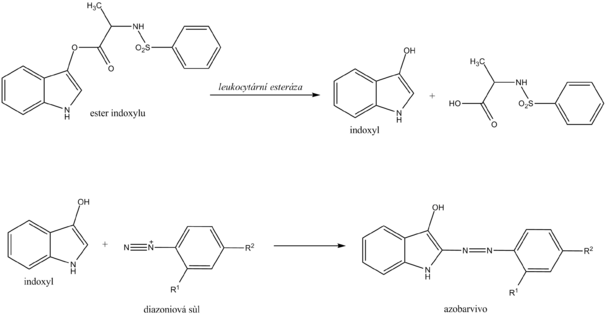
Chemical determination of leukocytes with a diagnostic strip is based on the detection of esterases that are abundant in granulocytes . Granulocyte esterases catalyze the hydrolysis of indoxyl ester to free indoxyl. The indoxyl then reacts with the stable diazonium salt to form the appropriate azo dye. In the case of a negative reaction, the zone turns cream yellow; in the case of a positive reaction, it changes to a pink to purple hue.
Chemical examination of leukocytes does not replace microscopic examination . On the other hand, it is possible to detect lysed leukocytes (eg in hypotonic urine ) in this way, which is not possible with microscopic examination.
Leukocyturia is a symptom of inflammation of the kidneys or urinary tract. The cause of most positive findings is a bacterial infection of the urinary tract . In case of a positive leukocyte finding, it is recommended to supplement the examination of proteinuria , hematuria , nitrituria , examination of urinary sediment and further microbiological examination .
Nitrite
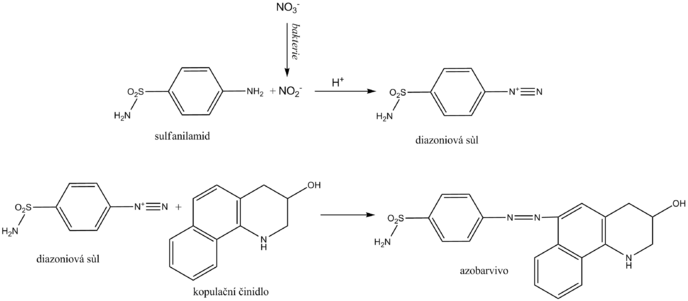
Nitrite is determined in the urine as an indirect sign of bacteriuria . Normal urine does not contain them in measurable concentrations. Some primarily gram -negative bacteria , such as Escherichia coli , Proteus , Klebsiella , staphylococci and others, have the ability to reduce the nitrates present in the urine to nitrite. Diagnostic strips for indirect detection of bacteriuria use nitrite in the so-called Griess reaction . Its essence is the diazotization of sulfanilamide with nitrite in the sample to form the diazonium salt. This is followed by azocoupling of the resulting salt with a coupling agent, developing a pink to purple color.
The nitrite urine test should be performed in the first morning urine, as in this case a sufficiently long time is guaranteed for the bacterial reduction of nitrates to nitrite in the bladder. Another recommendation is to consume enough vegetables (contains nitrates) the day before the examination. A positive urinary nitrite test confirms bacteriuria, while a negative one does not excrete it.
Indirect evidence of bacteriuria is indicative and does not replace microbiological examination.
Ascorbic acid
Ascorbic acid appears in the urine with high food intake. As a strong reducing agent, it can affect the determination of some analytes in urine, especially those that use hydrogen peroxide in the reactions. It is directly reduced with ascorbic acid. It also rapidly degrades diazonium salts used for azocoupling reactions.
The principle of ascorbic acid detection uses phosphomolybdic acid, which is reduced to molybdic blue by ascorbic acid. The reaction is not only specific for ascorbic acid, other substances with strong reducing effects react similarly.
pH
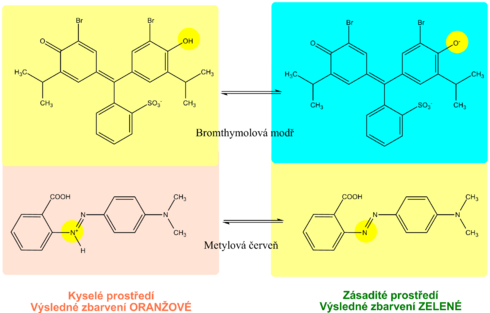
The pH indication zone contains a mixture of selected acid-base indicators. Most use two acid-base indicators - methyl red and bromothymol blue, or phenolphthalein . This ensures that the pH is read in the range 5-9 by changing the color from orange (acidic pH) to green to blue (alkaline pH). The reading is possible with an accuracy of 0.5.
Density
By relative urine density we mean the ratio of urine density to water density. The density of water is practically equal to 1 kg / l, so the difference between the density of water (in kg / l) and the relative density of urine is negligible. The density in the SI system is kg · m -3 . The density of the sample relative to the density of water is a relative quantity and is therefore given by a dimensionless number.
Determination of urine density
Urine density is estimated indirectly from cation concentrations using diagnostic strips. The indicator zone of the strip contains a suitable polyelectrolyte as an ion exchanger and the acid-base indicator bromothymol blue. The principle of diagnostic strips is based on the exchange of cations from urine, especially Na + , K + , NH 4 + , for H + polyelectrolyte ions in the indication zone. The released H + acidifies the weakly buffered acid-base indicator, which is in alkaline form. Acidification is accompanied by a change in the color of bromothymol blue. The disadvantage is that the examination with diagnostic strips does not take into account non-electrolyte substances such as glucose , proteins, urea ,creatinine and some others.
Urinary density is estimated indirectly by the concentration of cations using diagnostic strips. The indicator zone of the strip contains a suitable polyelectrolyte as an ion exchanger and the acid-base indicator bromthymol blue. The principle of diagnostic strips is based on the exchange of cations from urine, especially Na+, K+, NH4+, for H+ ions of the polyelectrolyte in the indication zone. The released H+ acidifies the weakly buffered acid-base indicator, which is in alkaline form. Acidification is accompanied by a change in colour to bromothymol blue. The disadvantage is that the diagnostic strip test does not take into account substances of a non-electrolyte nature such as glucose, proteins, urea, creatinine and some others.
Diagnostic strip test procedure
Remove only as many strips from the tube as you will need immediately. Immediately seal the tube with the remaining strips to protect the unused strips from moisture. Do not touch the indicator zone of the strips with your hands. Store the strips only in their original packaging and well sealed with a bag of desiccant, in a dark, dry place at a temperature of +2 to +30 °C.
Dip the strip briefly into the urine for 1-2 s so that all zones are wetted. Then remove the strip and remove the excess urine by wiping the edge of the strip on the rim of the container. Then place it in a horizontal position to prevent mixing of reagents from the individual reagent plates. After the prescribed reaction time, usually 60 s and 120 s for leucocytes, evaluate.
The assessment of the staining of the reaction zones of the diagnostic strips is carried out:
- subjective comparison of the resulting colour with the colour scale on the label of the tube in which the strips are stored;
- objectively' by reflection photometers, which measure the intensity of light of the appropriate wavelength reflected from the reaction field.
Overview of urine testing with diagnostic strips
| Analysis | Principle | False positives | False negative results |
|---|---|---|---|
| Protein | Acid-base indicator protein error | Alkaline pH, contamination of the sampling vessel with disinfectants based on quaternary ammonium salts, menstruation (do not test 3 days before and after), hemoglobinuria, mysoglobinuria | Globulins and immunoglobulin light chains are difficult to detect |
| Hemoglobine | Oxidation of chromogen by hydrogen peroxide by hemoglobin pseudoperoxidase activity | Microbial peroxidases, contamination of vessels with oxidative cleaning agents | High concentration of nitrite, vitamin C |
| Glucose | Glucose oxidase reaction coupled with peroxidase reaction | Contamination of vessels with oxidative cleaning agents | Vitamin C, other reducing agents (gentisic acid, DOPA), urinary infection |
| Ketone bodies | Reaction of acetoacetic acid and acetone with nitrpruside in alkaline media | Substances with free sulfhydryl groups (e.g. captopril). Some phenolphthalein- and sulfophthalein-based substances (laxatives and diagnostics) give similar colouration in alkaline environments. Phenylpyruvic acid. | β-hydroxybutyrate does not react |
| Bilirubin | Azocopulation reaction | Substances that have a similar coloration in acidic environments, nitrogen metabolites of bacteria in some urinary infections | High nitrite content, light exposure, ascorbic acid |
| Urobilinogen | Azocopulation reaction | Substances that have a similar coloration in acidic environments, nitrogen metabolites of bacteria in some urinary infections | Formaldehyde, light exposure, old urine, ascorbic acid |
| Nitrite | Griess reaction - diazotization of sulfanilamide by nitrite and subsequent azo copulation | Bacterial contamination | Dietary nitrate deficiency, Gram-positive bacteria, large diuresis, vitamin C |
| Leukocytes | Esterase activity of granulocytes and macrophages | Formaldehyde, alkaline pH, high urine density | Vitamin C, certain medications |
| pH | Mixture of acid-base indicators | Formaldehyde (apparently lower pH), old urine (alkaline pH) | |
| Density | Ion exchange of urine cations for H+, determination of pH with acid-base indicator | Alkaline pH shifts results to lower values |
Links
References
External links
- DASTYCH, Milan – WINKLER, Jaroslav. Automatická analýza moči [online]. Portál Lékařské fakulty Masarykovy univerzity, ©2005. [cit. 2011-11-25]. <http://portal.med.muni.cz/clanek-10-automaticka-analyza-moci.html>.
Used literature
- SCHNEIDERKA, Petr. Kapitoly z klinické biochemie. 2. edition. Karolinum, 2004. 365 pp. ISBN 80-246-0678-X.

![{\displaystyle \mathrm {H} _{2}\mathrm {O} _{2}+\mathrm {H} _{2}\mathrm {A} \ {\xrightarrow[{\mathrm {or\ hemoglobin\ and\ other\ substances} }]{\mathrm {peroxidases} }}\ 2\ \mathrm {H} _{2}\mathrm {O} +\mathrm {A} }](https://wikimedia.org/api/rest_v1/media/math/render/svg/fa4bd1ebd25f354a5f946fe1aa7959f58485ecf7)