Hemoglobin in urine
Up to a million erythrocytes per day are excreted in the urine of completely healthy people. This very small amount cannot be demonstrated by conventional chemical tests. Occurrence of a larger number of erythrocytes ( 'hematuria' , erythrocyturia) or penetration of free hemoglobin, or muscle myoglobin, into definitive urine (hemoglobinuria or myoglobinuria) is almost always a pathological finding. 'Macroscopic hematuria' is observed with the naked eye; the urine is pinkish (comparable to water from washed meat) and hemoglobin can be detected spectroscopically in it. There is at least 1 g of hemoglobin per liter in the urine. In massive hemoglobinuria, the urine may be dark beer (hemoglobin degradation to hematin]). 'Microscopic hematuria' can only be detected biochemically.
Determination of hemoglobin in urine[edit | edit source]
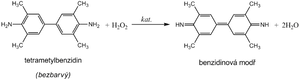
Hemoglobin catalyzes, similarly to peroxidase , the oxidation (dehydrogenation) of some substrates (e.g. benzidine derivatives ) by hydrogen peroxide:
However, it is not an enzyme activity (catalysis is conditioned by heme iron), and therefore it is not lost even after thermal denaturation. We are talking about pseudoperoxidase activity , which is used for sensitive but non-specific evidence of hemoglobin or trace amounts of blood. It is advantageous to use a chromogenic substrate to monitor the reaction, i.e. a substance that gives a distinctly colored product by dehydrogenation (often benzidine or its non-carcinogenic derivatives, aminophenazone, etc.).
The reagent zone of diagnostic strips contains a chromogen (e.g. tetramethylbenzidine ) with stabilized hydrogen peroxide (e.g. cumene hydroperoxide ). In the presence of free hemoglobin ( hemoglobinuria ), the indicator zone becomes uniformly blue. If erythrocytes are present in the urine ( erythrocyturia ), intensely greenish-blue colored dots or spots are formed.
Hemoglobinuria can be seen in intravascular hemolysis . Damage to the glomerular membrane ( glomerular hematuria ) and bleeding from any part of the urinary tract lead to more frequent erythrocyturia. It is often found in urinary tract infections , urolithiasis and tumors of the urogenital tract .
In addition to hemoglobin, myoglobin also provides a pseudoperoxidase reaction , which can be excreted in the urine during the breakdown of skeletal muscle ( rhabdomyolysis , crush syndrome ). The positivity of the test can also be caused by peroxidases of leukocytes or some bacteria, yeasts or fungi, which can occur in urine, especially during urinary tract infections . If we want to exclude the possibility of a false positive reaction due to the effect of cellular peroxidases, the reaction must be performed with boiled urine.
Contamination of the collection vessel with strong oxidizing agents also causes a false positive reaction. On the other hand, the presence of strongly reducing substances (e.g. ascorbic acid ) can slow down or stop the pseudoperoxidase reaction and thus be the cause of false negative results.