Nutritional disorders
Protein and energy malnutrition[edit | edit source]
Inadequate intake of protein and energy in food leads to a loss of both total body mass and adipose tissue, although not equally. Protein and energy malnutrition primarily occurs when the quality and quantity of nutrition is long-term insufficient. It is endemic in some developing countries, with a prevalence of up to 25 %. It is primarily a problem where the main food component is vegetable proteins with low biological value due to the current high incidence of infectious diseases. With insufficient energy supply, proteins are oxidized as an energy source and are not used for body protein synthesis. Clinical manifestations in children in developing countries are mainly two syndromes: kwashiorkor and marasmus.
Kwashiorkor[edit | edit source]
It is thought to be caused by a selective protein deficiency. It is manifested by short stature, edema, hypoalbuminemia, steatosis of the liver, and preservation of subcutaneous fat.
Marasmus[edit | edit source]
A condition caused by a total lack of energy. It manifests itself in the physical and mental assembly of the organism.
Secondary form of protein-energy malnutrition[edit | edit source]
It also occurs in industrialized countries as a result of pathological conditions leading to insufficient intake of nutrition in relation to the body's needs. The main causes can be:
- Reduced oral intake:
- Increased loss of nutrients:
- Increased need:
Malnutrition can develop slowly (chronic partial starvation) or rapidly on the basis of severe acute illness. In uncomplicated starvation or partial starvation, the organism can gradually adapt.
Eating disorders[edit | edit source]
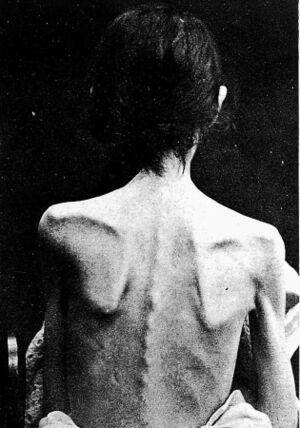
Anorexia nervosa[edit | edit source]
Anorexia It is a chronic disease characterized from a behavioral point of view by self-inflicted underweight, from a psychological point of view by the idea that thinness is the ideal of beauty, from a biological point of view by a number of disorders (e.g. amenorrhoea) caused by insufficient food intake. Metabolic disorders include loss of subcutaneous fat, decreased body core temperature, decreased blood pressure and pulse.
Discoloration of the skin (yellowing) is caused either by hypercarotenemia from an excess supply of β-carotene in a unilateral diet or by a breakdown in the degradation and utilization of carotenoids. Amenorrheic women have reduced FSH and LH, and the periodic release of LH during the day does not respond to the secretory stimulus via LH–RF (luliberin). The level of T3 tends to decrease, while its inactive isomer reverse T3 (rT3) increases. Under malnutrition and stress, the liver prefers deiodination of T4 to rT3. T4 and TSH response to TRH are normal. The level of cortisol in the plasma is normal or slightly reduced, the excretion of 17-hydroxycorticoids in the urine is reduced. The response to ACTH stimulation is increased, to metyrapone normal. The growth hormone level is normal or slightly elevated, while the somatomedin level is decreased.
Hematological findings usually include leukopenia, thrombocytopenia, and anemia, but resistance to infection is good.
Bulimia nervosa[edit | edit source]
It is a behavioral disorder characterized by episodes of excessive overeating, accompanied by feelings of "purging" again by induced vomiting, diarrhea (laxatives) or increased diuresis (diuretics). Unlike anorexics, bulimics have a normal body weight. Neurotransmitters such as serotonin, dopamine, noradrenaline, opioids and cholecystokinin, which modulate feelings of hunger and satiety, are involved in the development. Persistent vomiting is usually a finding of hypokalemic hypochloraemic alkalosis.
Obesity[edit | edit source]
Obesity and overweight are caused by the accumulation of body fat. A simple measure is Quetelet's "body mass index" (BMI), which is calculated according to the formula below:
hmotnost: mass
vyska: height
| BMI | Degree of obesity | |
|---|---|---|
| < 20 | Underweight | |
| 20–24,99 | Normal weight | |
| 25–29,99 | Overweight | I |
| 30–30,99 | Obesity | II |
| > 40 | Morbid obesity | III |
Obesity itself is not such a risk, but the location of accumulated fat is important. Fat in the abdominal area, especially fat around the abdominal organs (central obesity) is considered the most risky in terms of the occurrence of metabolic disorders. Abdominal adiposity can be indirectly measured using the waist and hip index (waist/hip). Visceral fat is an active metabolic tissue releasing fatty acids. The increased supply of fatty acids to the liver and peripheral tissues induces insulin resistance and, together with the alteration of the activity ratio of lipoprotein lipase and hepatic triacylglycerol lipase, this is the cause of dyslipidemia in obesity.
A fat cell (adipocyte) forms the body's energy reservoir by expanding or contracting according to the state of energy balance. It arises from a precursor - a preadipocyte, in order to adapt to the continued increased intake of energy in nutrition. During excessive intake, adipocytes gradually change their size up to a certain limit, which is 1 μg of weight. After that, preadipocyte differentiation is stimulated and new fat cells are produced, which can increase indefinitely, so that their total number in adipose tissue increases. However, once an adipocyte has formed, its dedifferentiation is very difficult. When energy intake is reduced, their number does not decrease, only their size decreases.
Genetic factors[edit | edit source]
So far, 23 genes have been identified that are associated with obesity. The mechanism of their action is not yet fully understood. It is assumed that more than 40% of cases of primary obesity are caused by genetics. Recently, attention has been focused on the so-called OB gene, which is responsible for the synthesis of leptin.
Leptin is a proteohormone of Mr= 16,000 belonging to the family of hematopoietic cytokines, which is the product of the OB-gene on chromosome 7q31.3, and which plays a key role in body weight regulation. It is produced by differentiated adipocytes. The main factor determining the level of circulating leptin is the amount of adipose tissue. Concentration increases with body mass index (BMI) or body fat percentage. Even small variations in the amount of body fat result in significant differences in leptin levels − from 0.03 μg/l in anorexic patients to values > 100 μg/l in extremely obese individuals. The level of leptin shows dependence on age (up to 20 years). The biological effect of leptin is mediated by the leptin receptor (OB–R), which belongs to the class I cytokine receptor family. Leptin causes a reduction in food intake (in experimental animals) and an increase in energy expenditure, including thermogenesis. In addition, leptin affects a number of endocrine systems. This effect is mediated by acting on the hypothalamus, namely on the production of neuropeptide Y (NPY) − leptin suppresses the expression and secretion of NPY, which is a food intake stimulator and regulates a number of pituitary hormones. In very simple terms, leptin represents a signal from adipose tissue, which informs the organism about the supply of energy stored in fat depots.
Diet[edit | edit source]
Genetic factors that underlie obesity are not enough on their own. Lifestyle and environmental factors allow these tendencies to manifest. The biggest role is played by the supply of energy-rich nutrients (hyperphagia = overeating) disproportionate to physical activity.
Endocrine causes[edit | edit source]
Some endocrine disorders are associated with adipose tissue accumulation and obesity. These include hypothyroidism, acromegaly, Cushing's syndrome, hyperprolactinemia (which is often attributed to obesity after childbirth). Growth hormone deficiency and hypogonadism are often associated with adiposity, but not necessarily with obesity. Type 2 diabetes mellitus, which is also often associated with obesity, probably have the same genetic predisposing factors. Increased insulin resistance and abdominal obesity are part of the so-called Reaven's metabolic syndrome (syndrome X).
Reaven syndrome[edit | edit source]
It is an association of several risk factors, the basis of which is apparently insulin resistance associated with obesity, hypertension, hypertriacylglycerolemia, hyperglycemia, to which others such as hyperuricemia, hirsutism, blood clotting disorders and fibrinolysis, microalbuminuria and the formation of so-called small LDL particles have been added; importantly, all these signs are associated with the development of premature atherosclerosis. However, metabolic syndrome and its causes cannot be understood as a manifestation of wear and tear or aging, but is based on a genetically disposed terrain.
Insulin resistance is a consequence of an alteration in insulin release from β-cells rather than a change in the threshold for glucose stimulation. An enlarged fat cell is less sensitive to the antilipolytic and lipogenic effect of insulin. Although a reduced number of insulin receptors is also involved in the development of insulin resistance, its result is much greater than the decrease in the number of receptors. So there must also be a postreceptor defect. It also occurs in other insulin-sensitive tissues, especially in muscle. As insulin resistance deepens, glucose uptake by peripheral tissues decreases and glucose output by the liver increases.
Links[edit | edit source]
Related articles[edit | edit source]
Other chapters from the book MASOPUST, J., PRÚŠA, R.: Pathobiochemistry of metabolic pathways
Source[edit | edit source]
- MASOPUST, Jaroslav a Richard PRŮŠA. Patobiochemie metabolických drah. 2. vydání. Univerzita Karlova, 2004. 208 s.