Icterus
Icterus or jaundice (Latin icterus) is a yellow discoloration of the tissues, which is visible on the skin, mucous membranes and the whites of the eyes of the affected person. The yellow discolouration of the tissues in jaundice is caused by the accumulation of bilirubin, which diffuses into the tissues after the binding capacity of albumin is exhausted (with bilirubinemia above 35 μmol/l). Jaundice is only a symptom accompanying a number of disease states and not a disease in itself.
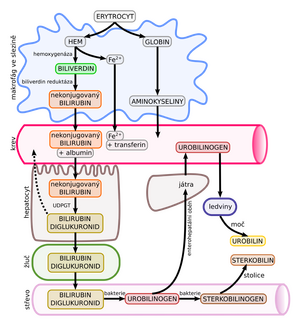
Bilirubin metabolism[edit | edit source]
The breakdown of erythrocytes releases haemoglobin, which is further broken down into haem and globin. Haem is then converted to biliverdin, which is converted to unconjugated bilirubin. The unconjugated bilirubin is then bound to blood proteins (albumin) and transported to the liver where it is conjugated with glucuronic acid. The conjugated bilirubin is water soluble (so it can be excreted in the urine if it accumulates) and is secreted from the liver into the bile ducts, which gradually coalesce and empty into the main bile duct. Through the bile duct, bilirubin as part of the bile enters the intestine, where it is converted by intestinal bacteria into stercobilinogen and causes a brownish discoloration of the stool. Part of the bilirubin is degraded by bacteria to urobilinogen, which is reabsorbed into the circulation and excreted in the urine (called enterohepatic circulation). The subsequent oxidation of urobilinogen to urobilin gives the concentrated urine a dark yellow colour.[1]
Briefly, the above metabolic process can be described as follows: heme → biliverdin → unconjugated bilirubin → conjugation in the liver → conjugated bilirubin → bile → faeces → excretion from the body/absorption (enterohepatic circulation) and conversion to urobilinogen.
If, for whatever reason, bilirubin (whether conjugated or unconjugated) begins to accumulate in the body, jaundice will result. The disorder can be at any level of its metabolism.
Manifestatitons of icterus[edit | edit source]
Macroscopically (colour of sclerae, skin, mucous membranes and body fluids)
- flavin icterus - yellow-green, in hemolytic icterus,
- verdine icterus - greenish, in obstructive icterus,
- icterus melas - olive-grey-green, in severe obstructive icterus,
- ruby icterus - orange-yellow, in hepatocellular icterus.
In addition, in newborns (immature blood-brain barrier), yellow-green staining of the nuclei of the thalamus, cerebellum, basal ganglia and olivary nuclei of the oblongata can be observed - the so-called nuclear icterus (kernicterus).
Microscopically
Well demonstrated in the kidney, where bilirubin forms granules in the proximal tubules and pigmented cylinders in the distal tubules.
Classification[edit | edit source]
According to the type of elevated bilirubin
- unconjugated icterus - hemolytic icterus,
- mixed icterus - hepatic icterus,
- conjugated icterus - obstructive icterus.
Depending on the cause
- prehepatic (hemolytic, dynamic, flavin) - increased production of bilirubin,
- hepatic (hepatocellular, hepatotoxic, ruby) - impaired transport of bilirubin into the hepatocyte, impaired intracellular transport and conjugation, impaired excretion into the bile,
- posthepatic (obstructive, cholestatic, mechanical, verdin) - impaired bilirubin transport through the bile ducts.
| type of icterus | Bilirubin in blood | Urine | stool | ||
|---|---|---|---|---|---|
| non-conjugated | conjugated | bilirubin | urobilinogen | ||
| prehepatic | + | normal | - | + | hypercholic |
| hepatic | + | + | + | + | hypocholic |
| posthepatic | slightly + | + | + | - | acholic |
Prehepatic icterus[edit | edit source]
Increased red blood cell breakdown (intravascular or extravascular haemolysis) is the dominant cause. If the red blood cells break down more, a lot of haemoglobin is released from them and a large amount of bilirubin is formed in the body. This amount exceeds the liver's capacity to conjugate and expel bile from the body. The accumulating bilirubin then stains the tissues yellow. The concentration of unconjugated bilirubin in the serum increases (but this is insoluble and does not pass into the urine - acholuria), bile drains into the intestine and contains increased amounts of bilirubin - more urobilinogen (resorbed into the blood and excreted by the kidneys - urobilinogen in the urine) and stercobilinogen (which darkens in the air to form stercobilin - hypercholar stools) is formed. Flavin icterus appears on the skin, bile acids do not enter the circulation and itching (pruritus) of the skin is not present.
Examples include icterus in hemolytic anemias (hereditary spherocytosis, immune destruction of erythrocytes, malaria), pernicious anemia, administration of incompatible transfusions, and in neonates where it occurs as icterus neonatorum simplex or icterus neonatorum gravis.
Hepatic icterus[edit | edit source]
Damage to the liver tissue from any cause will make it difficult to conjugate and excrete bilirubin into the bile. Bilirubin begins to accumulate in the body again and jaundice develops. Both conjugated bilirubin (water soluble, excreted in urine and giving it a dark colour) and unconjugated bilirubin accumulate in the body. The intestinal contents are hypocholic, the colour of the skin is orange-yellow (ruby icterus). A number of diseases belong to this group of causes:
- Alcohol damage to the liver: Alcohol abuse damages the liver and leads to alcoholic steatosis to cirrhosis. Jaundice is a rather late and very serious symptom of liver damage in the alcoholic cirrhotic.
- Wilson's disease: A hereditary disease characterized by the accumulation of copper in the liver, damaging it and the whole process can end in cirrhosis again.
- Infectious hepatitis: this is an infectious disease of the liver caused by many types of viruses - these are referred to by the letters A-F. Infectious hepatitis A, B, C, D are particularly well known.
- Liver tumours: advanced malignant liver tumours, whatever the cause, may be accompanied by jaundice. The malignant tumor tissue destroys the surrounding healthy liver tissue.
- Autoimmune hepatitis: Inflammation of liver tissue that is non-infectious. It is more common in women. The consequences are severe and the whole process can again end in cirrhosis.
- Liver damage by toxic substances (other than alcohol): There are a number of toxic substances that damage liver cells. These include, for example, high doses of paracetamol or poisons from certain fungi (amanitin and phalloidin in the green toadstool), chloroform, amphetamines, carbon tetrachloride. Jaundice may accompany acute poisoning with all these substances.
- Genetic disorders: there are genetic disorders that cause impaired uptake, conjugation or excretion of bilirubin:
- an increase in indirect (unconjugated) bilirubin,
- Gilbert's syndrome - defect in glucuronidation of bilirubin, possibly also a defect in the uptake of bilirubin by hepatocytes, manifested in adulthood,
- Crigler-Najjar syndrome - reduced UDP-glucuronate transferase activity (absent completely - type I or only partially - type II), manifested after birth (kernicterus),
- an increase in direct (conjugated) bilirubin,
- Dubin-Johnson syndrome - impaired hepatic secretion of bilirubin into bile, UDP-glucuronate transferase activity is normal, microscopically visible pigmentation of hepatocytes,
- Rotor syndrome - similar to Dubin-Johnson syndrome but without pigmentation.
- an increase in indirect (unconjugated) bilirubin,
Posthepatic icterus[edit | edit source]
Posthepatic or obstructive icterus is manifested by impaired bile outflow. Conjugated bilirubin cannot be excreted into the intestine and begins to accumulate in the body similar to the previous types of jaundice. Since in this type of jaundice the bile does not enter the intestine at all, the stool is not coloured with bile dyes and is pale to whitish. The absence of bile in the intestine causes malabsorption of fats - steatorrhoea, which can result in a deficiency of fat-soluble vitamins (hypovitaminosis A, D, E, K). In addition, accumulating bile acids often cause severe itching of the skin. Again, conjugated bilirubin accumulates and may be excreted in the urine, causing a dark colour in the urine, but no urobilinogen is found in the urine.
Obstruction of the bile ducts leads to the congestion of bile (cholestasis) - at first it is compensated by the accumulation of bile in the gallbladder (resorption of water and salts - its contents are dark and dense). Bile from the small bile ducts enters the interstitium of the liver, later up to the spaces of Disse (initially in the center of the lobules and spreading to the periphery), where it forms so-called biliary thrombi. Often an ascending infection from the intestine (Escherichia coli) joins - purulent cholangitis with sepsis develops, inflammation leads to fibroproduction up to the so-called cholestatic cirrhosis of the liver (secondary biliary cirrhosis).
Causes:
- Pancreatic tumours: very often, a tumour growing from the pancreas can obstruct the bile duct and prevent bile from draining out. Painless, sudden-onset jaundice in an elderly person is a classic symptom.
- Gallbladder tumors: A gallbladder tumour can obstruct the bile duct in a similar way to a pancreatic tumour and the symptoms will be exactly the same. Again, sudden painless jaundice occurs.
- Effects of alcohol: Alcohol has a dual effect on the liver. First, it damages the liver tissue and its ability to conjugate bilirubin. Secondly, alcohol prevents the liver cells from releasing bile into the bile duct, causing a condition similar to classic biliary obstruction.
- Cholelithiasis: If a gallbladder stone obstructs the bile duct, in addition to painful colic, jaundice can occur with prolonged obstruction.
- Autoimmune cholangiohepatitis: This is a condition similar to autoimmune hepatitis. In this case, the immune system of the patient attacks the tiny bile ducts in the liver and damages them. It causes impaired outflow of bile into the bile ducts and accumulation of bilirubin in the body.
- Congenital biliary atresia.
- Injury to the bile ducts in surgery (cholecystectomy).
Diagnosis[edit | edit source]
It is important to take a history, whether the jaundice was suddenly developed or whether the patient has any other symptoms (inappetence, nausea, pain, increased temperature, whitish stools, itchy skin, dark urine), (ab)anxiety of alcohol, etc. Abdominal examination by palpation is important.
Among others, the determination of the level of liver enzymes from the blood (ALT, AST, GGT, ALP) is used, which are elevated in hepatocyte damage (rather elevated ALT, AST) and in bile duct obstruction (rather elevated GGT, ALP). From blood samples, we can also determine the presence of viral infection in different types of infectious hepatitis, as well as the level of bilirubin itself, whose high concentration is crucial for the diagnosis of jaundice. In addition to the level, we are interested in whether the bilirubin is unconjugated or conjugated. Unconjugated bilirubin informs us of increased breakdown of red blood cells and conjugated bilirubin of liver damage or impaired bile outflow.
The examination is then supplemented by imaging methods: ultrasound, ERCP, MRCP and other examination methods according to the specific suspicion.
Prevention and treatment[edit | edit source]
For prevention and treatment, see individual diseases. Jaundice is a very serious symptom, and suspected cases must be reported to a doctor urgently. Jaundice can point to infections, dangerous tumors, poisoning, and liver damage in general.
Summary video[edit | edit source]
Links[edit | edit source]
Related articles[edit | edit source]
- Hyperbilirubinemia of newborns and infants
- Hepatite A, Hepatitis B,
- Hepatitis C, Hepatitis D, Hepatitis E, Hepatitis F, Hepatitis G
- Liver tumors
- Liver Function Tests
Sources[edit | edit source]
- ŠTEFÁNEK, Jiří. Medicína, nemoci, studium na 1. LF UK [online]. [cit. 31.3.2010]. <https://www.stefajir.cz/>.
References[edit | edit source]
- ↑ BILLING, B H a M BLACK. Bilirubin metabolism. Gut [online]. 1969, vol. 10, no. 4, s. 250-4, dostupné také z <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1552848/?tool=pubmed>. ISSN 0017-5749.