The effect of drugs on heart rate
The activity of the heart is controlled by the autonomic nervous system through mediators. The mediator of the sympathetic nervous system is noradrenaline, the mediator of the parasympathetic system is acetylcholine. Cardiac activity is also affected by adrenaline from the adrenal medulla. Acetylcholine suppresses cardiac activity, while norepinephrine has a stimulating effect on the heart. The action of mediators is mediated by specific receptors located on the cell membrane. Cardiac activity depends on the presence of calcium in the extracellular space and in the endoplasmic reticulum.
Drugs that affect the rhythm (and other functions) of the heart pump include cardioinhibitors, cardiotonics and antiarrhythmics.
Cardioinhibitors[edit | edit source]
Cardioinhibitors (drugs that reduce heart function) have a negative effect chronotropically (by reducing the heart rate) and inotropically (by reducing the contractility of the heart muscle), which leads to a reduction in cardiac output and blood pressure. These changes reduce the activity of the heart and thus the consumption of oxygen by the myocardium. The mechanisms of action of these drugs also include a reduction in electrical conduction (negative dromotropic effects).
The mechanical and metabolic effects of these drugs predispose them to the treatment of hypertension, angina pectoris and myocardial infarction. In addition, due to their effect on the electrical activity of the heart, they are suitable for the treatment of cardiac arrhythmias[1]. Some cardioinhibitors (especially certain β-blockers) are used to treat heart failure.
Hypertension[edit | edit source]
It is caused by an increase in cardiac output or an increase in systemic vascular resistance. Cardioinhibitors reduce the heart rate and heart rate, which leads to a reduction in cardiac output and thus to a decrease in blood pressure.
Angina pectoris and myocardial infarction[edit | edit source]
Cardioinhibitors (by reducing heart rate, contractility and arterial pressure) reduce the heart's work and its oxygen requirements. In this way, they can relieve the patient of anginal pain, which most often arises due to lack of oxygen during increased exertion. Significance in the treatment of myocardial infarction lies not only in the increase in the ratio of oxygen supply and demand, but also in the ability to inhibit post-infarction remodeling of cardiac tissue[1].
Cardiac arrhythmia[edit | edit source]
Cardioinhibitors alter pacemaker activity and conduction control, and are therefore useful in the treatment of arrhythmias caused by both abnormal automation and abnormal conduction[1].
Heart Failure[edit | edit source]
Although it may seem paradoxical that cardioinhibitors are used in heart failure when the myocardium is functionally suppressed, clinical studies have shown that certain cardiohibitors have been shown to improve cardiac function in certain types of heart failure[1]. This effect can be deduced from their blocking of excessive sympathetic effects on the heart, which damage failing hearts.
Drug classes and general mechanisms of their action[edit | edit source]
Clinically used cardioinhibitors can be divided into three groups: beta-blockers, calcium channel blockers and centrally acting sympatholytics.
Beta-blockers (beta-adrenergic receptor antagonists))[edit | edit source]
It binds to β-adrenergic receptors in the conduction system and in the working myocardium. There are both types in the heart: β-1 and β-2 adrenoreceptors. However, β-1 predominates numerically and functionally. These receptors primarily bind norepinephrine released from sympathetic adrenergic nerve endings. In addition, it weighs adrenaline and norepinephrine circulating in the blood. β-blockers prevent the binding of these ligands to receptors by competing with them for binding site. They reduce the effects of sympathetic drugs (ie, sympatholytics) that normally stimulate chronotropy, inotropy, and dromotropy. Their effect even increases when sympathetic activity is increased. Clinically used β-blockers are either non-selective (β-1 or β-2) blockers or relatively selective β-1-blockers (relative selectivity may be lost at higher drug doses). Some of the β-blockers have other effects besides β-blocking. The third generation of β-blockers are substances that have additional vasodilatory effects by acting on α-adrenoreceptors of blood vessels.
Some beta-blockers, upon binding to the β-adrenoceptor, partially activate this receptor while preventing noradrenaline binding. These so-called partial agonists (partial β-blockers) therefore provide a certain background for sympathetic activity, even if they prevent normal or increased sympathetic effects. We speak of them as carriers of intrinsic sympathomimetic activity (ISA). Some β-blockers also carry membrane stabilization activity (MSA), which is also found in sodium channel blockers belonging to antiarrhythmics.
β-adrenoceptors are coupled to Gs-proteins that activate adenyl cyclase. The increase in cAMP activates cAMP-dependent protein kinases (PK-A), which phosphorylate calcium channels and thus cause increased calcium flux into the cell. An increase in intracellular calcium during action potentials leads to increased calcium release from the sarcoplasmic reticulum, which ultimately increases inotropy (contractility). Gs-protein activation also leads to an increase in the frequency of heartbeats (chronotropy). PK-A protein kinases also phosphorylate portions of the sarcoplasmic reticulum, leading to increased calcium release via ryanodine receptors (ryanodine-sensitive calcium channels) associated with the sarcoplasmic reticulum. This provides more calcium for its binding to troponin-C, which increases inotropy. PK-A can further phosphorylate myosin light chains, which may contribute to the positive inotropic effect of β-adrenoceptor stimulation. They are used to treat hypertension, angina pectoris, myocardial infarction and arrhythmias[1].
Hypertension[edit | edit source]
β-blockers reduce arterial blood pressure by reducing cardiac output. They can thus be an effective treatment for hypertension, especially when used in combination with diuretics [1]. Hypertension in some patients is caused by emotional stress, which activates the sympathetic nervous system, while in other cases, for example, pheochromocytoma, which increases the level of circulating catecholamines. Even in these cases, treatment with β-blockers is successful. In addition, β-blockers inhibit the activity of the renin-angiotensin-aldosterone system. Acute treatment with β-blockers is not very effective in lowering blood pressure due to the compensatory increase in vascular resistance in the systemic circulation. The hypotensive effect of the substances in this group is detectable during the first days of treatment, but they do not reach full effect until after 2-3 weeks of administration[2].
Angina pectoris and myocardial infarction[edit | edit source]
The antianginal effect of β-blockers is attributed to their depressant effect on heart rate, contractility and their hypotensive effects. β-blockers reduce cardiac work and thus the need for myocardial oxygen saturation (see above).
Cardiac arrhythmia[edit | edit source]
The antiarrhythmic properties of β-blockers (class II antiarrhythmics) are related to their ability to inhibit the effect of sympathetic nervous activity. The sympathetic nervous system increases the frequency of excitations in the sinoatrial node, which increases the sinus rhythm. It also increases the rate of transmission of excitation to the ventricular myocardium and stimulates the formation of ectopic excitations. These sympathetic effects are mediated mainly through β-1-adrenoceptors. Therefore, β-blockers may reduce these effects, thus reducing sinus rhythm, atrial conduction velocity (which may block re-entry mechanisms), and inhibit abnormal pacemaker activity. β-blockers also affect non-pacemaker action potentials by increasing action potential duration and relative refractory periods. This effect may play a major role in preventing arrhythmias caused by the reentry phenomenon[1].
Heart Failure[edit | edit source]
Most heart failure patients suffer from systolic dysfunction, ie. the contraceptive function of the heart is limited (ie loss of inotropy). Although it is not entirely clear what mechanism β-blockers help with heart failure, it is certain that they improve heart function and reduce mortality[1].
| Class / Medicine | HTN | Angina | Arrhy | IM | CHF | Comment |
|---|---|---|---|---|---|---|
| Non-selective β-1/2 | ||||||
| carteolol | X | ISA; long acting; also used in glaucoma | ||||
| carvedilol | X | X | α α-blocking effect | |||
| labetalol | X | X | ISA, α α-blocking effect | |||
| nadolol | X | X | X | X | long acting | |
| penbutolol | X | X | ISA | |||
| pindolol | X | X | ISA, MSA | |||
| propranolol | X | X | X | X | MSA; a typical β-blocker | |
| sotalol | X | still has other effects | ||||
| timolol | X | X | X | X | still has other effects | |
| β-1-selective | ||||||
| acebutol | X | X | X | ISA | ||
| atenolol | X | X | X | X | ||
| betaxolol | X | X | X | MSA | ||
| bisoprolol | X | X | X | |||
| esmolol | X | X | particularly short effec | |||
| metoprolol | X | X | X | X | X | MSA |
Abbreviations: HTN - hypertension, Arrhy - arrhythmia, IM - myocardial infarction, CHF - congestive heart failure, ISA - own sympathomimetic activity
Calcium channel blockers (CCB)[edit | edit source]
It binds to L-type calcium channels (slow calcium channels[2]) in the cardiomyocyte membrane and nodal tissue. These channels are responsible for regulating calcium influx into the myocardial cell, which stimulates its contraction. In cardiac node tissue (SA and AV node), these channels play a role in pacemaker currents and the initial phase of action potential formation. Thus, by blocking the entry of calcium into the cell, these drugs act negatively inotropically (reduce the strength of the heartbeat), negatively chronotropically (reduce the heart rate) and reduce the rate of excitation transmission by the cardiac conduction system (negatively dromotropically affects the AV node in particular). In vascular smooth muscle, they induce relaxation and a decrease in peripheral resistance with a decrease in blood pressure[2]. They are used to treat hypertension, angina and arrhythmias.
Hypertension[edit | edit source]
By causing smooth muscle relaxation in the blood vessel wall, CCBs reduce systemic vascular resistance, thereby lowering blood pressure. These drugs act mainly on arterial resistant vessels, with minimal effect on venous capacity vessels[1].
Angina pectoris[edit | edit source]
The antianginal effects of CCBs are derived from their vasodilatory and cardiac suppressive effects. Systemic vasodilation reduces arterial pressure, which leads to a reduction in ventricular afterload, thereby reducing oxygen demand. For the heart, more selective CCBs (verapamil and diltiazem) reduce the frequency of heartbeats and myocardial contractility, making them (based on the reduction of myocardial oxygen requirements) excellent anti-angiogenic drugs[1]. CCBs can also cause coronary arteries to dilate, thus preventing their spasm (Prinzmetal's angina pectoris).
Cardiac arrhythmia[edit | edit source]
The antiarrhythmic group CCB (class IV antiarrhythmics) acts mainly by reducing the conduction velocity and prolonging repolarization, especially in the atrioventricular node. Delayed AV node action helps prevent reentry mechanism, which may cause supraventricular tachycardia.
Calcium channel blocker classes[edit | edit source]
We distinguish three classes of CCB. They differ not only in their basic chemical structure, but also in their relative selectivity to cardiac or vascular calcium channels. Most CCBs acting on vascular smooth muscle are dihydropyridines.. They are therefore mainly used to reduce vascular resistance and blood pressure, ie to treat hypertension. They are not used to treat angina pectoris, due to its strong vasodilatory and pressure-lowering effects, which can lead to reflex cardiac pacing (tachycardia and increased inotropy), which leads to a dramatic increase in myocardial oxygen consumption. Dihydropyrinidins include the following specific drugs:
- amlodipine;
- felodipine;
- isradipine;
- nikardipine;
- nifedipine;
- nimodipine;
- nitrendipine.
(Note: some newer substances such as amlodipine or isradipine are also called second-generation dihydropyridines[2].)
Non-dihydropyridines include two other classes of CCBs. Verapamil(phenylalkylamine class) is relatively selective for the myocardium and is less effective as a systemic vasodilator. This drug is very important in the treatment of angina and arrhythmias. Diltiazem (benzothiazepine class) is an intermediate step between verapamil and dihydropyridines in terms of selectivity for vascular calcium channels. It lowers the heart rhythm and has a vasodilating effect. Through these mechanisms, it is able to lower blood pressure without causing the same degree of reflex pacing as dihydropyridines[1].
Side effects and contraindications[edit | edit source]
Dihydropyrinidine CCBs can cause congestion, headache, excessive hypotension, edema, and reflex tachycardia. In terms of activation of sympathetic reflexes and lack of direct effects on the heart muscle, they are not very suitable for the treatment of angina pectoris[1].Long-acting dihydropyridines have been shown to be safer antihypertensives due to reduced reflex responses. Cardiac-selective non-dihydropyridine CCBs can cause excessive bradycardia, electrical transmission impairment (AV node blockage) and decreased contractility. Therefore, they should not be used in patients with chronic bradycardia, cardiac conduction defects or heart failure. CCBs (mainly non-dihydropyridine) should also not be prescribed to patients treated with β-blockers[1].
Centrally acting sympatholytics[edit | edit source]
The sympathetic nervous system plays a major role in the regulation of arterial blood pressure. It increases the heart rate (has a positive chronotropic effect), myocardial contractility (positively inotropically) and the conduction velocity in the heart (positively dromotropic effect). The adrenergic sympathetic fibers that innervate the heart and blood vessels are postganglionic efferent nerve fibers. The cell bodies of these nerves are found in the prevertebral and paravertebral sympathetic ganglia. The preganglionic sympathetic fibers that lead to the spinal ganglia originate in the elongated spinal cord. There are sympathetic excitatory neurons that have significant basal activity, which gives the heart a certain tone under basal conditions. These neurons receive signals from other vagal neurons from the nucleus tractus solitarii (it receives signals from peripheral baroreceptors and chemoreceptors) and from neurons in the hypothalamus. Together, this neural system regulates sympathetic (and parasympathetic) transmission to the heart and blood vessels. Sympatholytic drugs can block the sympathetic adrenergic system at three levels. The first, peripheral sympatholytics - α and β-adrenoceptor antagonists - block the effect of norepinephrine on the effector organ (heart or blood vessels). The others are so called ganglion blockers, which block the transmission of impulses in the sympathetic ganglia. The third group consists of drugs that block sympathetic activity within the brain. We call them centrally acting sympatholytics.
Centrally acting sympatholytics block sympathetic activity by binding and activating α2-adrenoceptors in the membrane of elongated spinal cord cells, which regulate cardiac activity. This reduces the effect of sympathetic nervous system and reduces cardiac output. These drugs are only used to treat hypertension[1].
Therapeutic indications[edit | edit source]
Centrally acting α-2-adrenoceptor agonists are used to treat hypertension, but are not used as first-line drugs due to their side effects in the brain. They are usually prescribed in combination with diuretics to prevent the accumulation of fluids, which would increase blood volume and thus reduce the effect of the drug. These drugs are useful in patients with kidney disease because they do not affect renal function[1].
Specific drugs[edit | edit source]
Several different centrally acting antihypertensives are used in clinical practice:
- clonidine;
- guanabenz;
- guanfacine;
- α-methyldopa.
Clonidine, guanabenz and guanfacine are structurally similar drugs and have identical antihypertensive effects. α-methyldopa is a structural analogue of dopa and must first be converted to α-methynoradrenaline, which only acts as an α-2-adrenoceptor agonist in the spinal cord and reduces sympathetic irritation. α-methyldopa is the drug of choice in the treatment of hypertension in pregnancy when its teratogenicity has not been established[1].
Side effects and contraindications[edit | edit source]
Side effects of centrally acting sympatholytics include sedation, xerostomia, bradycardia, orthostatic hypotension, impotence, and nausea. Swelling may occur during long-term therapy.
Cardiotonics Cardiotonics (pacemakers) potentiate heart function by increasing heart rate (chronotropy) and myocardial contractility (inotropy), which increases cardiac output and arterial pressure. Many of them also have a positive dromotropic and lusitropic effect. Some of these drugs cause systemic vasodilation, while others have vasoconstrictive effects. The effects of these drugs on the heart muscle predispose them to use in heart failure, cardiogenic shock and hypotension[1]. In the treatment of heart failure, cardiotonics today prefer procedures that reduce the demands on myocardial function - ie reduce afterload or preload, or both (diuretics, organic nitrates, calcium channel blockers, ACE inhibitors).[2]
Heart failure and cardiogenic shock[edit | edit source]
The main cause of heart failure and hypotension caused by acute heart failure (cardiogenic shock) is loss of myocardial contractility, which leads to reduced organ perfusion and hypotension. Cardiac function can be improved by reducing afterload, increasing preload (increased fluid volume) and increasing cardiac contraction. Cardiotonics work by this mechanism. Sympathomimetics or phosphodiesterase inhibitors are used for short-term therapy and may be harmful if used for a long time[1]. In contrast, cardiac glycosides (digitalis and others) are safe and effective in the long-term treatment of heart failure[1].
Circulatory shock[edit | edit source]
It is a form of shock caused by hypovolemia (for example in bleeding conditions) or vasodilation during infection (septic shock). Cardiotonics, especially sympathomimetics such as beta-agonists, are used to improve (ie increase) blood pressure. They are often used in conjunction with infusions and vasoconstrictor drugs.
Drug classes and general mechanisms of their action[edit | edit source]
Cardiotonics can be divided into four basic classes: beta-adrenoceptor agonists (beta-agonists), cardiac glycosides (digitalis and others), phosphodiesterase inhibitors and calcium sensitisers.
Beta-agonists[edit | edit source]
These are sympathomimetics that bind to cardiac β-adrenoreceptors. Activation of β-1 and β-2 adrenergic receptors leads to an increase in heart rate and contractility, which increases cardiac output. Their activation also has a positive dromo- and lusitropic effect. These drugs are indicated for both acute and refractory heart failure and circulatory shock. Β-Adrenoceptor agonists bind to β-receptors in the heart and smooth muscle. They also have effects in tissues other than the heart, especially in the smooth muscle of the bronchi (relaxation), liver (stimulating glycogenolysis) and kidneys (stimulating renin release). They therefore cause cardiac pacing (increased heart rate, contractility, rate of transfer, relaxation) and systemic vasodilation. An increase in arterial pressure may occur, but not necessarily, as a decrease in vascular resistance interferes with an increase in cardiac output. Thus, the final effect on blood pressure depends on the relative effect on cardiac or vascular receptors[1]. β-agonists cause β-receptor down-regulation, which limits their use to short-term. As they are catecholamines (and have low bioavailability), they must be administered by intravenous infusion. [1]. The principle of operation of β-adrenergic receptors - see above.
Specific drugs and their therapeutic use[edit | edit source]
The table shows several different β-agonists that are used clinically to treat heart failure and circulatory shock. These are either natural catecholamines or their analogues. Almost all have a certain degree of α-agonist activity. For some of these drugs, receptor selectivity is highly dose dependent.
| Drug | Receptor selectivity | Clinical use | Comment |
|---|---|---|---|
| Adrenalin | β-1 = β-2> α-1 = α-2 | Anaphylactic shock; cardiogenic shock; cardiac arrest | Low doses cause cardiac pacing and vasodilation. It has a vasoconstrictive effect at high doses. |
| Noradrenaline | β-1 = α-1> β-2 = α-2 | Severe hypotension; septic shock | Reflex bradycardia masks direct stimulatory effects on the SA node. |
| Dopamine | β-1 = β-2> α-1 | Acute heart failure, cardiogenic shock and acute renal failure | Biosynthetic precursor of noradrenaline, stimulates its release.
At low doses, it stimulates the heart and reduces systemic vascular resistance. It has a vasodilating effect at high concentrations. |
| Dobutamine | β-1> β-2> α-1 | Acute heart failure; refractory heart failure | The net effect is cardiac pacing with weak vasodilation. |
| Isoproterenol | β-1 = β-2 | Bradycardia and AV block. | The net effect is cardiac pacing and vasodilation with little pressure change. |
Side effects and contraindications[edit | edit source]
The main side effect of β-agonists is cardiac arrhythmias. Because they increase myocardial oxygen demand, they can accelerate the development of angina pectoris in patients with coronary artery disease. They can also cause headaches and tremors[1].
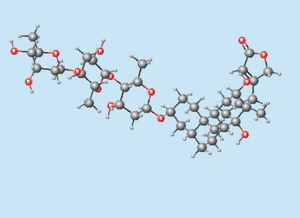
Cardiac glycosides (digitalis)[edit | edit source]
They have been used for more than 200 years to treat heart failure.They represent a family of compounds derived from the plant Digitalis purpurea (foxglove). These drugs inhibit Na + / K + ATPase in cardiac sarcolemma, leading to an increase in intracellular calcium through the Na + / Ca 2+ -exchange system. The increase in intracellular calcium subsequently stimulates the release of additional calcium from the sarcoplasmic reticulum, its binding to troponin C, which increases contractility.
Due to the long half-life of digitalis, this fact should be considered when dosing. It should be administered for several days to reach its therapeutic plasma level (0.5-1.5 ng / ml[1]). Digitalis has a relatively narrow therapeutic window. Plasma concentrations higher than 2.0 ng / ml can be toxic[1]. Digitalis toxicity is manifested by (sometimes life-threatening) cardiac arrhythmias. Digibind (immune mechanism) or potassium supply are used to reduce digitalis levels (especially if toxicity is associated with hypokalaemia).
Therapeutic use:
Heart Failure[edit | edit source]
Digitalis compounds have cardiotonic effects and are used in heart failure. Although new and more effective drugs are already available, digitalis is still widely used. Clinical studies in patients with heart failure have shown that digoxin, when used in combination with diuretics and vasodilators, increases cardiac output and ejection fraction and reduces filling and capillary wedge pressures[1]. This reduces congestion in the lungs and the risk of edema. Heart rate changes slightly. These effects are expected with a drug that increases inotropy.
Atrial fibrillation and flutter[edit | edit source]
Atrial fibrillation and atrial flutter lead to an accelerated ventricular rate that can affect their filling (reducing their filling time). Digoxin and other drugs in this group are useful in reducing the ventricular rate, which was initiated by the increased rate of atrial contractions. The mechanism of this beneficial action of digoxin is its parasympathomimetic effect. Activation of the vagus can reduce the rate of conduction through the atrioventricular node to the point that some impulses are blocked. A smaller number of pulses is then fed to the chambers and the frequency of the chamber contractions decreases. In addition, digoxin increases the relative refractory period in the AV node.
| Drug | Oral absorption | Half-life (hours) | Elimination |
|---|---|---|---|
| Digoxin | 75 % | 40 | kidneys |
| Digitoxin | >90 % | 160 | liver |
| Oubain | 0 % | 20 | kidneys |
Note: Oubain is no longer used today. [2]
Side effects and contraindications[edit | edit source]
The most significant side effect of digitalis is cardiac arrhythmias, especially atrial tachycardia and atrioventricular block. The drug is contraindicated in patients with hypokalaemia, AV block or Wolff-Parkinson-White syndrome. Impaired renal function leads to increased plasma concentrations of digitoxin as it is eliminated by the kidneys.
Phosphodiesterase inhibitors[edit | edit source]
These are drugs that inhibit the enzyme (cAMP-dependent phosphodiesterase, PDE) responsible for reducing cAMP. This leads to an increase in cAMP levels, which has a positive inotropic and chronotropic effect in the heart. cAMP is the second messenger in the pathway initiated by the binding of catecholamines to beta1-adrenergic receptors coupled to Gs-proteins. This is followed by activation of the adenyl cyclase and the formation of cAMP. cAMP (reaction with other intracellular messengers) increases contractility, heart rate and conduction velocity.
These drugs are used to treat acute and refractory heart failure, but not chronic heart failure. The drugs used target cAMP-dependent phosphodiesterase (PDE3) isoform 3 [1].
Therapeutic indication[edit | edit source]
The pacing and vasodilatory properties of PDE3 inhibitors predispose them to the treatment of heart failure. Artery dilation reduces the afterload of a failing ventricle and leads to an increase in ejection fraction and organ perfusion. The reduction in afterload leads to a secondary decrease in preload, which increases the mechanical efficiency of the dilated heart and reduces the oxygen requirements of the failing myocardium. The pacing effect of these drugs increases inotropy, which leads to an increase in heart rate and ejection fraction. However, tachycardia is also the result, so drugs are dosed to minimize the positive chronotropic effect. The baroreceptor reflex, which appears in response to hypotension, may also contribute to tachycardia. Clinical trials have shown that long-term therapy with PDE3 inhibitors increases the mortality of heart failure patients. These drugs are very useful in the treatment of acute decompensated heart failure[1].They are always used together with other drugs such as diuretics, ACE inhibitors, β-blockers or digitalis.
Specific drugs[edit | edit source]
PDE3 inhibitors are milrinone and amrinone (possibly emoximone and piroximone[2]). ((PDE5 inhibitors are used to treat erectile dysfunction).
Side effects and contraindications of PDE3 inhibitors[edit | edit source]
The most common and at the same time most serious side effect of PDE3 inhibitors are ventricular arrhythmias, some of which can reach life-threatening proportions. Some patients may experience headaches and low blood pressure[1].
Calcium sensitizers[edit | edit source]
They represent the most pacemaker class. These drugs increase the sensitivity of troponin-C to calcium, so more calcium binds to it, which increases the contractility of the heart. These drugs are currently undergoing clinical trials for possible use in heart failure[1].These include, for example, some phosphodiesterase III inhibitors (sulmazol, imobendan, levosimendal)[2].
>Antiarrhythmics (also antidysrhythmics) are drugs used to treat heart rhythm disorders, and in some cases preventively. They affect cardiac contractility and hemodynamics[2].
Arrhythmia pharmacotherapy depends on the type of arrhythmia, its duration, severity, and the condition of the heart muscle. Arrhythmias are divided into tachyarrhythmias and bradyarrhythmias.
The mechanisms of tachyarrhythmias may be increased irritability, increased automaticity, or reentry. Treatment - reduction of excitability and automaticity, treatment of ischemia is based on the diagnosis of the mechanism of arrhythmia.[3]
Therapeutic use[edit | edit source]
The main goal of antiarrhythmic treatment is to restore normal heart rhythm and transmission; possibly at least to prevent more severe to fatal arrhythmias. They reduce or increase the speed of conduction, change the excitability of the heart cells and suppress abnormal automation.
All antiarrhythmics alter membrane conductivity by the following mechanisms:
- By blocking fast sodium channels. These channels determine the rate of membrane depolarization during the action potential, which can help eliminate tachyarrhythmias caused by the reentry mechanism.
- By influencing the course of action potentials and especially the relative refractory period.Prolonging the relative refractory period can often eliminate tachycardias. These drugs affect potassium channels and delay the repolarization phase.
- By blocking slow calcium channels. These drugs reduce the sinus frequency by slowing the depolarization of pacemaker cells. They also reduce the excitation speed of the AV node.
- By blocking sympathetic activity, which can also cause arrhythmias, β1-adrenergic receptor blocking drugs are used to suppress this sympathetic effect on the heart. Because β-adrenoceptors are coupled to ion channels, β-blockers also indirectly alter ion flux across the membrane, especially calcium and potassium.
- In the case of AV block, vagal inhibitors (eg atropine, a muscarinic receptor antagonist) are sometimes used. AV block may occur during treatment with β-blockers.
- In some cases, the ventricular rate is inadequate because it is initiated by atrial flutter or atrial fibrillation. Because it is very important to prevent ventricular tachycardia, drugs are often used to slow the excitation of the AV node. Calcium channel blockers and β-blockers are often used for this purpose. For the same reason, the parasympathomimetic effect of digitalis can be used.[4][1]
Antiarrhythmics often have a proarrhythmic effect, so they should only be used for symptomatic arrhythmias that worsen the patient's quality of life or prognosis.[3]
Classes of drugs used to treat arrhythmias[1][edit | edit source]
- Class I - Fast sodium channel blockers – atrial fibrillation cardioversion, etc.
- Ia - blockade of Na + channels - quinidine,
- Ib - blockade of Na + channels - lidocaine, trimecaine, phenytoin
- Ic - blockade of Na + channels - propafenone, flecainide
- Class II - β-blockers (see above) - control of ventricular response in supraventricular tachycardia,
- Class III - Potassium channel blockers (eg amiodarone) - supraventricular and ventricular tachycardia,
- Class IV - Calcium channel blockers (verapamil, diltiazem) - supraventricular tachyarrhythmias only.
- Next:
- adenosine,
- electrolyte supplementation (magnesium and potassium salts),
- cardiac glycosides (digitalis),
- atropine (muscarinic receptor antagonist),
- bradines (SA node blockers)[3].
Class Ia antiarrhythmics[edit | edit source]
Class Ia antiarrhythmic sodium channel blockade prolongs action potential duration and slightly prolongs repolarization[2].
- Quinidine
For pharmacological cardioversion of atrial fibrillation and flutter. It has many side effects.
- Procainamide
Used to treat ventricular and supraventricular arrhythmias.
- Disopyramide
For the treatment of tachyarrhythmias, especially after a heart attack.
Class Ib antiarrhythmics[edit | edit source]
They block the sodium channel, but have little effect on the rate of increase in action potential. They shorten the repolarization time[2].
- Lidocaine, trimecaine
Used mainly in the treatment of ventricular tachycardia.
Class Ic antiarrhythmics[edit | edit source]
They block the sodium channel, significantly slowing down the rate of action potential onset and conduction. The time of repolarization is little affected by them[2].
- Propafenone
Used to treat atrial fibrillation and ventricular tachycardia.
Class I antiarrhythmics are not commonly used today, except for propafenone and phlecainide (both of Class Ic)[3].
Class II antiarrhythmics[edit | edit source]
These are β-adrenergic blockers. They reduce calcium channel phosphorylation. They negatively affect the frequency of spontaneous depolarization in the SA and AV nodes. They do not affect the repolarization time[2].
Class III antiarrhythmics[edit | edit source]
They block potassium channels, prolong the action potential and dampen the effect of sympathetic nervous system. They prolong the refractory of the atria, transmission system and ventricles[3].They are used in atrial fibrillation and ventricular tachycardia.
- Amiodarone
It has a slow onset of action and an extremely long elimination half-life (up to 100 days), so we must monitor its plasma level. It is the most effective antiarrhythmic in suppressing ventricular and supraventricular tachycardias. It is indicated after an acute myocardial infarction, at a high risk of sudden cardiac death and impaired left ventricular systolic function. Amiodarone has an undesirable negative inotropic effect, which requires careful use in heart failure. At the same time, however, it is the only antiarrhythmic that reduces the risk of atrial fibrillation (eg again in heart failure)[3].It has numerous side effects, especially thyroid disorders (hypothyroidism, rarely hyperthyroidism), bradycardia, pulmonary fibrosis, hepatotoxicity and corneal deposits.
- Sotalol
It prolongs the duration of the action potential and slows down the repolarization phase. Use is limited due to its lower antiarrhythmic effect[3].
Class IV antiarrhythmics[edit | edit source]
Calcium channel blockers verapamil and diltiazem inhibit conduction in the AV node. They do not affect the repolarization time. They are mainly used for supraventricular tachycardias[2].
Adenosine[edit | edit source]
Adenosine acts by stimulating potassium channels. It is given intravenously for its short duration of action. It reduces the automation of the sinus node and slows down the conduction of excitation in the atrial node. It slows the response of the ventricles in supraventricular arrhythmias (it is the medicine of first choice). It can also be given during pregnancy.
Bradins[3][edit | edit source]
Bradins act selectively in the sinus node, where they slow down spontaneous diastolic depolarization. Their effect is only to slow down the heart rate.
The main indication for bradin is angina pectoris.
Summary of antiarrhythmic classes[1][edit | edit source]
| quinidine | anticholinergic (moderate)) | cinchonismus (visual disturbances, tinnitus, headache); nausea; potentiates digitalis toxicity |
| procainamide | anticholinergic (weak); relatively short half-life | lupus-like syndrome in 25-30% of patients |
| disopryamide | anticholinergic (strong) | negative inotropic effect |
| lidocaine | IV only; VT and PVC | high efficiency in ischemic myocardium |
| mexiletine | orally active lidocaine | analogue high potency in ischemic myocardium |
| phenytoin | digitalis-induced arrhythmias |
| flecainide | SVT | can induce life-threatening VT |
| propafenone | SVT & VT | β-blocking and Ca2 + -channel blocking activity may exacerbate heart failure |
| moricizin | VT | activity IB |
Arrhythmia treatment - summary[1][edit | edit source]
| Status | Drug | Comment |
|---|---|---|
| Sinus tachycardia | Class II, IV | Other related conditions may require treatment. |
| Atrial fibrillation/ flutter | Class IA, IC, II, III, IV, digitalis, adenosine | The goal is to control ventricular rate; necessary anticoagulant treatment. |
| Paroxysmal supraventricular tachycardia | Class IA, IC, II, III, IV, adenosine | |
| AV reentry tachycardia | atropine | Acute reversal. |
| Ventricular tachycardia | Class I, II, III | |
| Premature ventricular complexes (PVC) | Class II, IV; Mg2 + salts | Often benign and do not require treatment |
| Digitalis toxicity | Class IB, Mg2 + salts; KCl |
Cardioinhibitory[edit | edit source]
Cardiotonika[edit | edit source]
__ Kardiotonika
Arrhythmia treatment - summary[edit | edit source]
Links[edit | edit source]
References[edit | edit source]
- KLABUNDE E., Richard. Cardiovascular Pharmacology Concepts [online]. © 2005. Last revision 2009, [cited. 4/24/2010]. < http://www.cvpharmacology.com/ >.
- ↑Jump up to:a b c d e f g h i j k l m n HYNIE, Sixtus. Pharmacology in a nutshell. 2nd edition. Prague: Triton, 2001. ISBN 80-7254-181-1 . Wrong citation: Invalid tag
<ref>; the name "Hynie" is used multiple times with different content - ↑Jump up to:a b c d e f g h BULTAS, Jan. Course Pharmacotherapy of cardiovascular diseases . 3. LF UK, 2010
- ↑ SCHROETER, Ute and James ROGERS. Cardiovascular pharmacology for anesthetists (World Anesthesia Online, issue 11) [online]. © 2000. [feeling. 4/22/2010]. < https://www.ndcn.ox.ac.uk/divisions/nda/wfsa/html/u11/u1102_01.htm >