Cardiac Output
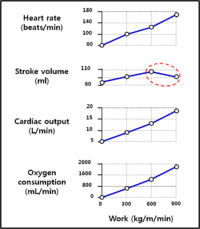
Cardiac output (CO) is the amount of blood pumped by the heart per unit of time and it depends on 2 important variables like below;
- Stroke volume (SV) = the amount of blood ejected per beat of the heart (Normally, 70 ml/beat).
- Heart rate (HR) = heart beats per minute (normally, 70 beats/min).
Therefore, the cardiac output (CO) is dependent on the stroke volume (SV) and the heart rate (HR): CO (L/min) = SV (ml/beat)Ⅹ HR (beats/min) = 4.9 L/min (normally).
Preload:
Afterload:
Cardiac output:
Stroke volume[edit | edit source]
Stroke Volume is the difference between end diastolic volume (EDV) and end systolic volume (ESV). ESV can be affected by 4 factors; preload, afterload, contractility, and Heart rate, and EDV also depends on 3 factors; venous return, Heart rate, and compliance.
- Preload (ie, the EDV):The more cardiac muscle is stretched, the harder it contracts (Frank & Starling's law).
- Positive agents:
- Slow heart rate,
- exercise.
- Negative agents:
- blood loss,
- rapid heart rate: when you exercise, heart rate can increase. See the graph.
- Contractility: Heart muscle fibers can contract at different strengths.
- Myocardial contractility is the intrinsic ability of the heart to contract independent of preload and afterload.
- Changes in the ability to produce force during contraction result from different degrees of binding between myosin and actin filaments.
- No relationship with the changes in the fiber length!
- The degree of binding that occurs depends on concentration of calcium ions in the cell;.
- In an intact heart, it is usually the action of the sympathetic nervous system (through catecholamines) that determines the concentration of calcium ions in the cytosol of cardiac muscle cells.
- All factors that cause an increase in contractility work by causing an increase in intracellular Ca2+ during contraction.
- Positive agents:
- ↑ Calcium of ICM by Hormones and sympathetic nervous system,
- cardiac glycosides (e.g. digoxin),
- drugs.
- Negative agents:
- ↑ extracellular K+ (Hypercalemia).
- Acidosis: H+ and K+ exchange across the membrane and if one H+ is heading in, a K+ is heading out and vice versa.
- Ca2+ channel blocker.
- Afterload (ie, the mean arterial pressure): Resistance to blood leaving the heart. In fact, afterload cannot be controlled by the cardiac function, but affects the cardiac out. So, these are the positive causes for afterload;
- High hematocrit,
- stenosis of vessels,
- high blood pressure,
- constricted blood vessels,
- lipids in vessels (atherosclerosis).
- Compliance: a measure of the tendency of a hollow organ to resist recoil toward its original dimensions upon removal of a distending or compressing force. It is the reciprocal of "elastance".
- Venous return: the amount of blood that enters the heart from the venous circulation and it can be controled by skeletal muscle contraction, venoconstriction, respiratory, venous valves, and so on.
Heart Rate[edit | edit source]
Heart rate can be determined by autonomic nervous system. An average resting heart rate in an adult is 70 beats per minute (bpm). The normal range for heart rate is highly variable, however. Trained athletes may have resting heart rates of 50 bpm or less. Someone who is excited or anxoius may have a rate of 125 bpm or higher. Children have higher average heart rates than adults. Although heart rate is initiated by autorythmic cells in the SA node, it is modulated by neural and hormonal input.
- Autonomic Nervous System
- Sympathetic NS: Fight or Flight → ↑ HR (→ always, ↑contractility);
- Parasympathetic NS: Rest and Digest → negative effect on HR.
- Bainbridge reflex (↔ Preload) increases the HR when the cardiac muscle is over-stretched.
- The Bainbridge reflex, also called the atrial reflex, is an increase in heart rate due to an increase in central venous pressure. Increased blood volume is detected by stretch receptors located in both atria at the venoatrial junctions.
- ↑ Venous return → ↑ the pressure of vena cavae and then the right atrium → stimulation of the stretch receptor at the venoatrial junctions → signaling the medullary control centers to decrease parasympathetic tone via the vagus → ↑HR.
- Drawing more blood out of the right atrium → a decrease in atrial pressure and the great veins.
- This continues until right atrial blood pressure returns to normal levels, upon which the heart rate decreases to its original level.
Links[edit | edit source]
Related articles[edit | edit source]
References[edit | edit source]
- Guyton Physiology, 11th edition
- Ganong’s Review of Medical Physiology, 22th edition
- Physiology at a glance, Cardiovascular physiology at a glance
- Silverthorne’s Human Physiology, 5th edition
- Essential Cell Biology, 3rd edition (cell communication)
- http://www.kirkwood.edu/- Kirkwood community college
- http://en.wikipedia.org/wiki/Bainbridge_reflex
- Contractility: http://en.wikipedia.org/wiki/Contractility
- hyperkalemia: http://en.wikipedia.org/wiki/Hyperkalemia
- Physiology at MCG 3/3ch7/s3ch7_10
- Vascular compliance