Pulmonary embolism
Pulmonary embolism[edit | edit source]
Pulmonary embolism (PE) is life threating condition, which occure when there is an obstruction of a. pulmonalis or its branches. The most common cause of embolism is trombembolis, most comonly from the lower limb. Another cause is fat embolism, amniotic fluid embolism, air embolism or cancer cell embolism.
The effect of a pulmonary embolus is mechanical (obstruction of the pulmonary artery or its branches), until secondary vasoconstriction and bronchoconstriction are associated.
Origins of trombembolus[edit | edit source]
Most thromboemboli originate from the proximal deep veins of the lower limbs (popliteal veins and femoral veins) and pelvic veins. More than 50% of patients with proximal deep vein thrombosis are reported to have concomitant evidence of pulmonary embolism. Other, less frequent, sources include vv. renales, v. cava inferior, right heart and also, in connection with the introduction of central venous catheters, v. cava superior.
Pulmonary embolization rarely occurs with deep vein thrombosis in the calf region. Up to two-thirds of thrombi in this location dissolve spontaneously. However, a certain risk is represented by their possible extension to veins located proximally, from where embolization is much more likely.
Risk factors[edit | edit source]
Congenital risk factors primarily include genetically determined thrombophilic conditions.
The most common is:
- the Leiden mutation
- the prothrombin gene mutation
Also common risk factors
- protein S and C
- anithrombin III defects
- antiphospholipid syndrome
Among the main acquired risk factors we count:
- a history of thrombosis or pulmonary embolism,
- major surgery (especially orthopedic) and trauma (mainly lower limbs),
- oncological disease (up to 20% of patients with symptomatic deep vein thrombosis have known active malignancy),
- pregnancy and oral contraceptives,
- immobilization (often after operations and injuries, or during long trips
- primary varices,
- older age and obesity,
- venous catheters and others
Several risk factors, either acquired or congenital, are often involved in the pathogenesis of venous thrombosis simultaneously. It is reported that up to 50% of cases of venous thrombosis in patients with congenital thrombophilia are associated with the presence of another acquired risk factor. An example of a combination of several risk factors can be the so-called economy class syndrome, in which there is a combination of lack of movement, compression of the veins of the lower limbs and dehydration during a long flight.
In general, this is blood stasis in the veins, trauma to the venous wall, hemocoagulation defect.
Consequences of embolization[edit | edit source]
The effect of embolization includes:
- ventilation-perfusion disorder with systemic hypoxia
- sudden pulmonary hypertension with right-sided heart failure
Classification[edit | edit source]
It is clinically advantageous to distinguish between the following types of pulmonary embolism:
- acute massive pulmonary embolism; pulmonary trunk obstruction occurs, the patient dies of acute right ventricular failure (dilatation)
- acute submassive pulmonary embolism; a large part of the bloodstream is obstructed, but if the patient was in good cardiac condition before the embolism, he usually survives (thromboembolus dissolves further or granulation tissue is organized to form a scar or fibrous loop),
- acute small pulmonary embolism
- subacute massive pulmonary embolism
- chronic thromboembolic pulmonary hypertension
Symptoms[edit | edit source]
Clinical symptoms can be of different levels- from asymptomatic emboli to manifestations of shock, heart failure and sudden death. It depends on the extent of the embolism and the physiological reserves of the patient.
The most common subjective symptoms include:
- sudden onset of shortness of breath (rest or exertion);
- chest pain of any nature (substernal, pleuritic) due to RV ischemia or pulmonary infarction;
- cough;
- hemoptysis in pulmonary infarction;
- syncope.
The most common objective symptoms include:
- tachypnea;
- tachycardia;
- hypotension, syncope to cardiogenic shock;
- sweaty, pale skin, cyanosis, delirium;
- signs of deep vein thrombosis;
- fever (above 38.5°C)
Diagnostics[edit | edit source]
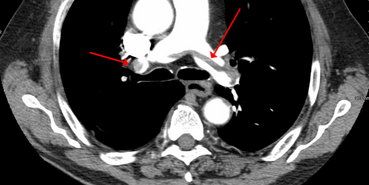
The methods with the most evidence are CT-angiography and ventilation-perfusion lung scan (failure of perfusion with maintained ventilation; this method is not completely reliable).
Other appropriate tests include:
- D-dimers (ELISA test/LIA test - a value below 500 μg/l with high sensitivity excludes pulmonary embolism);
- X-ray of the chest (insufficient for diagnosis);
- echocardiography (overloading of the right heart chamber leading to its dilatation can be detected, or TEE access to a thrombus in the a. pulmonalis);
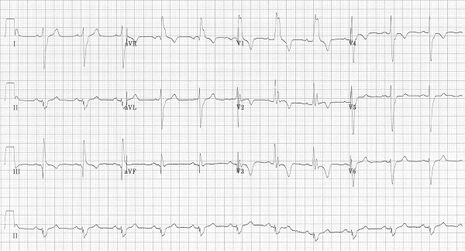
- ECG
- examination of blood gases (hypoxemia with hypocapnia and respiratory alkalosis; in shock, on the contrary, hypercapnia and respiratory acidosis);
- pulmonary angiography;
- MRI (accurate, non-invasive, expensive, time-consuming);
- Duplex ultrasound examination of DK veins to confirm/exclude phlebothrombosis
Differencial diagnostics[edit | edit source]
In differencial diagnostics we must exclude:
- heart attack
- aortic dissection;
- in case of syncope, also cardiac tamponade, massive bleeding, severe arrhythmias;
- bronchial asthma;
- pneumothorax;
- bronchopneumonia;
- COPD
Diagnostics algorithm[edit | edit source]
Hemodynamically unstable patient
1. CT-angiography is immediately available → we will perform CT-angiography
→ positive result → treatment (thrombolysis, embolectomy)
→ negative result → we look for another cause
2. CT-angiography is not immediately available → we will perform echocardiography
→ positive result → confirmation by CT-angiography or immediate treatment (thrombolysis, embolectomy)
→ negative result → we look for another cause
Hemodynamically stable patient → we estimate the probability of pulmonary embolism
1. high probability → CT-angiography
→ positive result → treatment
→ negative result → we look for another cause
2. low or medium probability → we determine D-dimers
→ negative result → we look for another cause
→ positive result → CT-angiography (when pulmonary embolism is confirmed → treatment)
Treatment[edit | edit source]
There is a possiblity, that with severe PE, the shock will occure, so we must treat the shock - we can aplicate dopamine or if necessery, we start CPR.
Farmacotherapy[edit | edit source]
- Anticoagulation treatment.
- Heparin/Low molecular weight heparin.
- Warfarin, NOAC
- Thrombolytic treatment (t-PA - alteplase, streptokinase, urokinase) with subsequent anticoagulant treatment.
Surgical therapy[edit | edit source]
- Catheterization techniques (percutaneous mechanical thrombectomy via femoral vein or jugular vein) – in massive PE with contraindications to fibrinolysis.
- Classic pulmonary thrombectomy according to Trendelenburg (without the use of extracorporeal circulation, time-limited retraction of the inferior vena cava and superior vena cava, opening of the trunk of the a. pulmonary artery, removal of the thrombus; this technique is no longer used today).
- Pulmonary thrombectomy currently used (with the use of extracorporeal circulation after median sternotomy, cannulation of vv. cavae and aorta, cardioplegic cardiac arrest, opening of the a. pulmonary trunk, thrombus removal, revision of the main a. pulmonary branches).
Supportive treatment[edit | edit source]
Supportive therapy includes modification of the internal environment, oxygen therapy, inotropic agents (dopamine, dobutamine, noradrenaline, levosimendan) or mechanical support of the heart.
Prevention of pulmonary embolism[edit | edit source]
Primary prevention is key to reducing morbidity and mortality in high-risk patients (predisposition, present disease, performance, etc.). Secondary prevention to prevent recurrence, at least 3 months after experiencing PE.
Things we can do
- early mobilization after surgery, support of physical activity, physiotherapy, dorsal-plantar flexion, compression stockings;
- anticoagulant treatment – low molecular weight heparin;
- caval filter implantation.
Non-trombtotic pulmonary embolism[edit | edit source]
- Air embolism – neck injury, some types of surgery
- Fat embolism – bone fractures or orthopedic operations, cardiopulmonary resuscitation
- Septic emboli – in infective endocarditis from the tricuspidal valve (especially drug addicts)
- Tumor cells
- Amniotic fluid – complicated by the development of DIC
Indication of imagining methods[edit | edit source]
CT angiography has a non-negligible risk of false-positive diagnosis of pulmonary embolism. It is necessary to indicate an examination after a clinical assessment. Otherwise, the patient will be at risk of unnecessary treatment.
Sources[edit | edit source]
Related articles[edit | edit source]
Sources[edit | edit source]
- WIDIMSKÝ, J a J MALÝ, et al. Doporučení diagnostiky, léčby a prevence plicní embolie, verze 2007. Cor et Vasa [online]. 2008, roč. 50, vol. supplementa, s. 1S25–1S72, dostupné také z <http://www.kardio-cz.cz/resources/upload/data/128_22-plicni_embolie2008.pdf/>. ISSN 0010-8650.
- THOMPSON, Taylor B a Christopher KABRHEL. UpToDate : Overview of acute pulmonary embolism [online]. Wolters Kluwer, ©2018-08-21. [cit. 2019-08-27]. <https://www.uptodate.com/contents/overview-of-acute-pulmonary-embolism-in-adults?search=lung%20embolism&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H446824308>.s?
- BAUER, Kenneth A a Gregory YH LIP. UpToDate : Overview of the causes of venous thrombosis [online]. Wolters Kluwer, Poslední revize 2019-02-05, [cit. 2019-07-09]. <https://www.uptodate.com/contents/overview-of-the-causes-of-venous-thrombosis?>.
- TORBICKI, Adam, et al. Acute Pulmonary Embolism (Diagnosis and Management of). Eur Heart J [online]. 2008, roč. -, vol. 19, s. 2276-2315, dostupné také z <https://www.escardio.org/guidelines-surveys/esc-guidelines/GuidelinesDocuments/guidelines-APE-FT.pdf>. ISSN 1522-9645.
- THOMPSON, Taylor B a Christopher KABRHEL. UpToDate : Overview of acute pulmonary embolism [online]. Wolters Kluwer, ©2018-08-21. [cit. 2019-07-06]. <https://www.uptodate.com/contents/overview-of-acute-pulmonary-embolism-in-adults?search=lung%20embolism&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H446824308>.
- VANĚK, Ivan, et al. Kardiovaskulární chirurgie. 1. vydání. Praha : Karolinum, 2003. 236 s. ISBN 8024605236.Použitá literatur
- BARRY DONALD HUTCHINSON, Patrick Navin. Overdiagnosis of Pulmonary Embolism by Pulmonary CT Angiography. 2015.
- ČEŠKA, Richard, ŠTULC, Tomáš, Vladimír TESAŘ a Milan LUKÁŠ, et al. Interna. 3. vydání. Praha : Stanislav Juhaňák - Triton, 2020. 964 s. s. 234-239. ISBN 978-80-7553-780-5.
- PASTOR, Jan. Langenbeck´s medical web page [online]. [cit. 2010-05-10]. <https://langenbeck.webs.com/>.