Perthes disease
Perthes disease (synonyms: Calvé-Legg-Perthes disease, coxa plana ) is the most common and severe avascular bone necrosis .
The disease was described independently in 1910 by: Georg Perthes (German), Jacques Calvé (Fr.) and Arthur T. Legg (USA).
Idiopathic disease of the hip joint caused by impaired blood supply to the proximal epiphysis of the femur, The ossification center of the femoral head succumbs to necrosis , is resorbed and gradually rebuilt into living bone . The result can be a fully functional hip joint or various deformities leading to the development of early osteoarthritis . It mainly affects (4x more often) boys aged 3–8 years, in 10% it is bilateral.
Etiopathogenesis[edit | edit source]
Transient disorder of the vascular supply of the head , thinning of its structure, subchondral fracture, gradual fragmentation of the necrotic epiphysis and subsequent remodeling.
The triggering factor of ischemia of unknown cause and duration. It leads to the development of avascular necrosis of the proximal epiphysis of the femur (more and more importance is attached to discrete forms of coagulopathies with the participation of proteins C and S and hypofibrinolysis ). There is an attenuation of enchondral ossification . The superficial cartilaginous part of the epiphysis continues to grow. In the next phase, the vascular supply and new bone formation gradually occur ( condensation stage ).
As a result of loading the limb, subchondral fractures appear (disrupting vascularization and prolonging the stage of necrosis). Further revascularization takes a long time ( stage of gradual remodeling ). The head of the femur is gradually formed depending on its relationship to the acetabulum and the degree of load.
Clinical picture[edit | edit source]
It often begins with a painless limp associated with secondary hypotrophy of the thigh muscles. Adduction and external rotation contracture in the hip gradually develops (slight pain in the groin).
The course is individual. The age of onset of the disease plays a decisive role (younger people are better). The course in children older than 9 years is usually very serious and the result is never perfect (so-called back Perthes
Display methods [ edit | edit source ][edit | edit source]
X-ray image [ edit | edit source ][edit | edit source]
At first we see the widening of the joint space ( Waldenström's sign , due to cartilage edema and synovialitis). Later, symptoms of structural irregularity (slight demineralization of the epiphysis, then its condensation and gradually appearing subchondral fracture ). According to the native x-ray image, Waldenström (1922) distinguished 4 stages of the disease (simplified: normal finding → head condensation → fragmentation to pulverization → remodeling).
- Initial stage
- Lasts 6 months, pathology: ischemia / necrosis.
- Pre-radiological stage : lateralization of the head, ossification core slightly smaller, widening of the medial joint space, thickened capsule, soaked muscles around the hip joint.
- Necrotic stage : subchondral fracture - Salter's sign, increased density of the head.
- Fragmentation stage
- Lasts 8 months, pathology: revascularization. Fragmentation and collapse of the ossifying nucleus of the head. Critical period – decentration (consequences) may occur: or it may occur without serious symptoms, ending with the formation of newly formed bone in the subchondral areas of the head.
- Reossification, healing stage
- Lasts 21 months, begins with subchondral bone neoplasia. Most heads improve their shape at this stage.
- Residual stage
- A final state in which the warhead density is no longer changing. The remodeling process continues until growth stops.
Scintigraphy[edit | edit source]
Suitable for early diagnosis, already in the 1st stage of the disease there is an increased metabolic turnover.
Magnetic resonance imaging[edit | edit source]
Changes in the T1W + T2W image depend on the degree of the disease. MRI is especially useful for early diagnosis.
Arthrography[edit | edit source]
Assessment of congruence and head placement prior to planned osteotomy of the proximal femur or pelvis. The concept of the so-called head at risk is important for determining the treatment procedure, which includes X-ray and clinical symptoms (horizontal course of the physis, Gage's sign - a line in the shape of the letter "V" on the lateral side of the metaphysis and epiphysis, calcification lateral to the epiphysis ,
Diffuse metaphyseal reaction – lateral subluxation of the head, obesity , adduction contracture with restriction of movement.
Classification schemes[edit | edit source]
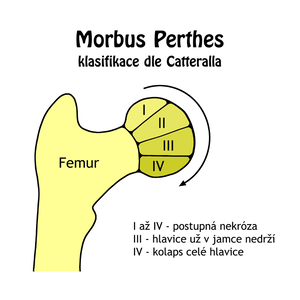
Classification according to Catterall[edit | edit source]
According to the extent of necrosis . Evaluation is performed from images in anteroposterior and Lauenstein projection.
Classification according to Catterall[edit | edit source]
According to the extent of necrosis . Evaluation is performed from images in anteroposterior and Lauenstein projection.
- Group I – affected only the front part of the pineal gland up to 25% of its extent.
- II. group – a larger part of the head is affected (the front half of the pineal gland, up to 50%), the affected segment of the head may collapse, the height of the pineal gland is preserved.
- III. group - the majority of the pineal gland is "sequestered" (75% of the pineal gland is involved), changes in the adjacent metaphyses.
- IV. group – the entire epiphysis is affected, extensive changes on the metaphysis and acetabulum.
Classification according to Herring[edit | edit source]
It assesses the extent of involvement of the lateral pillar of the head on the anteroposterior projection.
- type A – normal lateral pillar height.
- type B – more than 50% of the height of the lateral pillar remains.
- type C – the collapse of the external pillar is greater than 50% of the original height.
Classification according to Salter and Thompson[edit | edit source]
It assesses the extent of the subchondral fracture.
- type A – affects less than ½ of the head.
- type B – affects more than ½ of the head.
Differential diagnosis[edit | edit source]
Transient synovialitis – mostly post-infectious ( HCD virus ), manifested by general symptoms (temperature, increased sedimentation and CRP ) and local symptoms. Concentric contracture with limitation of hip joint mobility.
Treatment[edit | edit source]
Conservative therapy[edit | edit source]
Traction treatment to remove the contracture → Atlanta splint (30° abduction). Long-term relief. Indicated for children up to 6 years old without a so-called risk head. Previously (ie until the 1970s), conservative treatment was preferred, but it meant a stay in a sanatorium for 1-2 years.
Operative therapy[edit | edit source]
It consists in the so-called containment therapy - immersion of a biologically malleable head into the spherical space of the acetabulum. If containment is observed, the head will not be deformed during rebuilding.
Children with a finding of risk head, older than 6 years, second or higher degree according to Catterall. The most frequently used 2 surgical procedures (separately / in combination).
- Varis osteotomy of the proximal femur ,
- pelvic osteotomy (Salter, Steel), in which the head is fully immersed by lowering the acetabulum.
Before surgery, RHB is suitable , which serves to release the contracture and restore the full range of motion in the hip joint. After the operation, a plaster cast is applied for 6 weeks. After 3 months, walking is allowed with the exclusion of sports activities.
Links[edit | edit source]
References[edit | edit source]
- DUNGLE, P., et al. Orthopedics. 1st edition. Prague: Grada Publishing, 2005. ISBN 80-247-0550-8 .
- KOUDELA, K., et al. Orthopedics. 1st edition. Prague: Karolinum, 2004. ISBN 80-246-0654-2 .
- SOSNA, A., P. VAVŘÍK and M. KRBEC, et al. Basics of orthopedics. 1st edition. Prague: Triton, 2001. ISBN 80-7254-202-8 .
Individual references[edit | edit source]
- ↑Jump up to:a b c d e f g h i j k l m DUNGL, P., et al. Orthopedics. 1st edition. Prague: Grada Publishing, 2005. ISBN 80-247-0550-8 .
- ↑Jump up to:a b c d e f g h i KOUDELA, K., et al. Orthopedics. 1st edition. Prague: Karolinum, 2004. ISBN 80-246-0654-2 .
- ↑Jump up to:a b c d SOSNA, A., P. VAVŘÍK and M. KRBEC, et al. Basics of orthopedics. 1st edition. Prague: Triton, 2001. ISBN 80-7254-202-8 .