Defects in cellular immunity
Disorders of cellular immunity are characterized by susceptibility to infections caused by viruses, fungi, parasites and intracellular bacteria. Recurrent infections that do not resolve spontaneously or on antibiotic therapy are characteristic. Disorders of cellular immunity can be divided into primary and secondary immunodeficiencies. Due to the synergism of T- and B-lymphocytes in antibody production, T-lymphocyte disorders usually present secondarily in antibody immunity disorders.
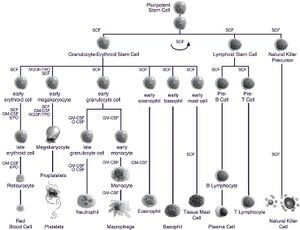
Cells of the immune system[edit | edit source]
The cells of the immune system are divided into 2 lineages according to their development.
The lymphoid line contains:
- T-lymphocytes (mediate a specific immune response),
- B-lymphocytes (provide specific antibody immunity),
- NK cells (cytotoxic cells of non-specific immunity).
The myeloid series includes:
- monocytes - macrophages (antigen-presenting phagocytic cells),
- dendritic cells,
- neutrophils (phagocytic cells of early inflammatory reaction),
- mast cells (cells of the type I hypersensitivity reaction)
- basophils (peripheral blood cells involved in the inflammatory reaction),
- eosinophils (cells involved in the hypersensitivity reaction and antiparasitic defence)
Etiology[edit | edit source]
Microorganisms causing disease in persons with predominantly impaired cellular immunity are usually typical opportunistic pathogens:
- Bacteria: Mycobacterium tuberculosis and atypical mycobacteria, Salmonella enterica, Legionella pneumophila, Listeria monocytogenes, Nocardia sp.,
- Fungi: Pneumocystis carinii, Candida sp., Cryptococcus neoformans, Histoplasma capsulatum, Coccidioides immitis, Mucorales (class Zygomycetes),
- Parasites: Toxoplasma gondii, Cryptosporidium parvum, Microsporidia, Strongyloides stercoralis
- Viruses: Cytomegalovirus, Herpes simplex virus, Varicella-zoster virus, Epstein-Barr virus, Papovaviruses,
Clinical manifestations[edit | edit source]
Severe combined immunodeficiency manifests as early as a few days after birth. Some congenital syndromes associated with immune deficiency (DiGeorge syndrome) may first manifest with associated symptoms, and infections do not occur until later.
Pneumonia (mycotic, legionella, pneumocystis, cytomegalovirus), pulmonary and extrapulmonary tuberculosis, pulmonary and disseminated mycobacteriosis, orogastrointestinal infections (esophagitis candida, cytomegalovirus, herpetic; intestinal cryptosporidiosis, perianal cellulitis or abscess), hepatic infections (cytomegalovirus hepatitis), skin infections (herpetic, ecthyma, gangrene), neuroinfections (listeria meningitis, corynebacterial meningitis, cryptococcal meningitis, tuberculous meningitis), generalised infections (salmonella bacteraemia, fungemia (Candida, Aspergillus, cytomegaly).
Primary cellular immunodeficiencies[edit | edit source]
Primary immunodeficiencies are usually caused by a disorder at the gene level.
- DiGeorge syndrome - a congenital abnormality in the development of the 3rd and 4th Gill flaps → craniofacial dysmorphism, hypoparathyroidism (hypocalcemia), congenital heart defects, and thymic hypoplasia (rarely a complete absence of the thymus, and T-lymphocyte development is provided by either residual thymic tissue or extrathymic differentiation of T-lymphocytes in the gastrointestinal tract); incidence: 1:50,000.
- Chronic mucocutaneous candidiasis - fungal involvement of mucous membranes and skin caused by selective impairment of T-lymphocyte response to candida antigens
- Differential diagnosis: may also be a rare manifestation of mannosidosis or biotin deficiency; also part of autoimmune polyglandular syndrome type I; may be a manifestation of SCID.
Combined immunodeficiency (CID)[edit | edit source]
- functional disorders of T-lymphocytes, the molecular basis of which is heterogeneous
- the concentration of lymphocytes in the blood may be normal
- the clinical picture is similar to that of SCID, but infections usually occur later in life; various manifestations of autoimmunity are common
- treatment symptomatic, bone marrow transplantation indicated
Secondary cellular immunodeficiencies[edit | edit source]
Cell-mediated immunodeficiency is particularly common in HIV infection, Hodgkin's disease, trichocellular leukemia, after immunosuppressive therapy and occurs about one month after organ transplantation or bone marrow transplantation. Lymphocytotoxic cytostatic drugs, which significantly reduce the number of CD4+ lymphocytes, are particularly risky in terms of impaired cellular immunity.
Diagnostics[edit | edit source]
The number of lymphocytes, T-lymphocytes, CD4 (helper T-lymphocytes) and CD8 (cytotoxic T-lymphocytes) is examined; in vitro stimulation of T-lymphocytes (so-called blastic transformation). Skin tests, HLA typing and cytokine testing are performed.
Impaired cellular immunity is usually characterized by a decrease in T-lymphocytes <1000/mm3 or CD4+ lymphocytes <500-200/mm3.
Links[edit | edit source]
Related articles[edit | edit source]
External links[edit | edit source]
References[edit | edit source]
- MUNTAU, Ania Carolina. Pediatrie. 4. vydání. Praha : Grada, 2009. s. 213-214. ISBN 978-80-247-2525-3.
- ↑ LEBL, J, J JANDA a P POHUNEK, et al. Klinická pediatrie. 1. vydání. Galén, 2012. 698 s. s. 231. ISBN 978-80-7262-772-1.
- ↑ http://fvl.vfu.cz/export/sekce_ustavy/mikrobiologie/imunologie/Prednasky/02_8_bunky_organy_bariery.pdf
- ↑ Skočit nahoru k:a b c d ROZSYPAL, H. Infekce specifických skupin : Porucha buněčné imunity [online]. Klinika infekčních a tropických nemocí 1. LF UK, ©2001. [cit. 2011-02-28]. <http://www1.lf1.cuni.cz/~hrozs~hrozs/disp1.htm>.
- ↑ Skočit nahoru k:a b c HRODEK, Otto a Jan VAVŘINEC, et al. Pediatrie. 1. vydání. Praha : Galén, 2002. s. 140-145. ISBN 80-7262-178-5.