Congenital syphilis
Congenital syphilis (lues connata, congenita) is an acquired disease transmitted from an infected mother to the fetus, by the transplacental route during pregnancy. Syphilis is a sexually transmitted disease caused by the spirochete Treponema pallidum. It is a bacterium that has been shown to have teratogenic effects on fetal development. The consequences are very variable (from mild to infant death), usually very severe. The clinical manifestation is conditioned by the stage of the disease in the mother and the gestational age of the fetus.
Today, serological testing of antibodies against syphilis is one of the basic diagnostic tests in all pregnant women (in the first and third trimesters). In the case of positive screening, we initiate treatment with penicillin, which not only cures the mother's infection, but also acts to prevent the transmission of the infection to the fetus, but also in the treatment of the already infected fetus.
Etiopatogenesis[edit | edit source]
The causative agent of syphilis, is exclusively a human bacteria - spirochete Treponema pallidum (subspecies pallidum). It is a tissue parasite that has the typical shape of a helix and is capable of rotating around a long axis (not locomotion). Spirochetes are highly sensitive to exposure to disinfectants, but also to drought, but in an unfavorable environment they can form cysts, which also protect them from drug penetration and the immune response of the infected organism.
The fetus / newborn can become infected transplacentally (vertically) from about the 9th to the 10th week of pregnancy (ie after completion of placental development) at any time during its subsequent course or by direct contact with the mother's lesions during childbirth. The probability of transmission of the infection to the fetus depends on the stage of syphilis in the pregnant / mother: 60% to 100% during primary and secondary syphilis, 40% during early latent infection and 8% during late latent infection , ie the shorter the interval between untreated early maternal infections and pregnancy, the worse the consequences for the child (Kassovitz's law) . If the infection occurs in utero, spirochetes disseminate in the fetal body, similar to secondary, acquired syphilis. Untreated congenital syphilis may go through the same stages as postnatally acquired syphilis, only the primary stage is missing.
- Infection of the mother before or during the 1st trimester, the mother is treated correctly → a healthy fetus.
- Mother infection at conception, mother untreated → massive placental infections (placental villi contain syphilitic granulomatous tissue, so-called Fräkelk granulomas), T. pallidum penetrates transplacentally into the fetal blood → fetus is poorly nourished, remains small and in the 7th to 8th month of pregnancy abortion occurs.
- Infection of an elderly mother (late secondary syphilis) → less affected placenta (less treponemata) → living child with clinical signs of congenital syphilis.
- Infection of a mother of very old date (late syphilis) → the baby may be healthy.
- Infection of the mother only a few weeks before birth → the child may be healthy, but there is a risk of infection of the child with florid infectious lesions during childbirth → acquired syphilis with the development of primary effect at the site of inoculation (syphilis connatalis).
- Infection of the mother in the second trimester causes the birth of a sick child (syphilis congenita tarda).
- Infection of the mother in the third trimester causes the birth of a sick child (syphilis congenita recens).
Clinical picture[edit | edit source]
The Hutchinson triad is a manifestation of late congenital syphilis and includes barrel incisors, visual impairment (interstitial keratitis), and hearing impairment (cranial nerve damage VIII).
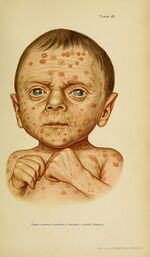
Syphilis congenita praecox / recens, lues connata praecox (manifestation in neonatal age);
- occurs in older maternal infections or maternal infections in the second half of pregnancy
- faded, yellowish, old, sagging skin;
- severe anemia, hepatosplenomegaly, failure to thrive;
- chrysanthemum (bloody rhinitis);
- pneumonia alba (fibrous pneumonitis - yellow-white enlarged lungs; histologically: connective tissue proliferation in interalveolar septa and interstitium with loss of alveolar space and obliterative fibrosis; on X-ray: complete opacity of both lung fields; in 10% of cases it can lead to chronic lung disease) ;
- interstitial hepatitis (flint liver);
- osteochondritis syphilitica (causes disintegration of the pineal gland and thus Parrot's pseudoparalysis), further causes deformation of the skull;
- Hochsinger infiltrates on the lips;
- Parrot scars or Fournier scars (radial scars around the lips caused by the healing of Hochsinger infiltrates);
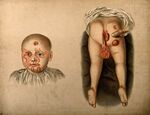
- syphilitic pemphigoid (blisters on the palms and palms);
- alopecia, paronychia;
- symptoms of adult secondary lues
- the fetus is usually born prematurely;
- hydrocephalus encephalomeningitis;
- skin - papular rashes, papulopustular, condylomata lata (in intertriginous areas; papules merging into painless, moist, grayish-white to red, highly infectious plaques);
- mucous membranes - enanthem, may be chronic rhinitis, vocal cord involvement (wheezing);
- Majority of children dies very young.
Syphilitic symptoms in the period of recurrence in 2-4. year of life
- clinical picture of acquired syphilis, in addition:
- condylomata lata, mucous plaques , gummata , tuberoserpiginous syphilms
Syphilis congenita tarda, lues connata tarda (school to adolescent) :
- occurs in latent maternal infections
- begins at five years, maximum change in puberty ;
- dorsal tabs, paralysis (quaternary metals), optic neuritis;
- defective healing lues connata praecox (luetic stigmata): Parrot grooves, caput natiforme / quadratum (cubic skull shape), saddle nose, gothic floor, swelling of the sternal end of the clavicle, saber-shaped tibia,
- Hutchinson trias (blindness - keratitis parenchymatosa / keratitis profunda , corneal opacity; hearing loss due to inner ear involvement - vestibular deafness, barrel incisors - upper incisors narrow to the cutting edge, which is cut crescently)
| Early form of congenital syphilis (up to 2 years of age) | Late form of congenital syphilis |
|---|---|
| Hepatosplenomegaly | Hutchinson's teeth |
| Hemorrhagic rhinitis (coryza) | Interstitial keratitis of the eyes (aged 5 to 20 years) |
| Condylomata lata | Deafness based on VIII (aged 10 to 14 years) |
| Osteochondritis, periostitis | Saddle-shaped nose, prominent mandible |
| Mucocutaneous lesions (bulls on palms and soles) | Perioral fissures (ragads) |
| Jaundice | Mental retardation, convulsions |
| Non-immune hydrops fetus | saber like shin, Olympic forehead |
| Hemolytic anemia, coagulopathy, thrombocytopenia | Clutton joints (symmetrical painless swelling of the knees) |
| Pneumonitis | |
| Nephrotic syndrome | |
| Intrauterine Growth Retardation (IUGR) |
Diagnosis[edit | edit source]
Diagnosis of congenital syphilis in the newborn can be difficult because maternal treponemal and non-treponemal IgG antibodies cross the placenta into the fetal blood. Diagnosis of congenital syphilis includes:
- maternal history (syphilis status, details of possible treatment),
- the child's clinical condition (presence of clinical, laboratory and radiological signs of syphilis),
- examination of paired serum of newborn and mother, ie. comparison of antibody titers.
- definitive serological diagnosis is usually possible only after the age of 18 months, when the antibodies transmitted from the mother completely disappear.
Laboratory diagnostics[edit | edit source]
- Direct identification of the causative agent from lesions or body fluids
- microscopically in the shadow or by PCR,
- possible only in manifest stages, suitable only in situations where the presence of T. pallidum can be expected;
- Indirect detection of specific antibodies in serum, plasma or cerebrospinal fluid
- non-treponemal tests – detection of non-specific anticardiolipin antibodies
- VDRL (Venereal Disease Research Laboratory) micro test, RPR (Rapid Plasma Reagin) test;
- treponemal tests – detection of specific antibodies against antigens (lipoproteins) of T. pallidum;
- include screening (TPHA, TPPA, EIA) and confirmatory tests (IgM detection by FTA-abs, ELISA, WB); in immunocompetent patients, antibody activity can be demonstrated from about 4 to 5 weeks after infection; furthermore, mostly even after adequate lifelong therapy (in the IgG class);
- TPHA (Treponema pallidum hemagglutination test), TP-PA (Treponema Pallidum Particule Agglutination), ELISA and EIA (Enzyme immunolinked assay) and others.
Decree No. 306/2012 Coll. determines the screening for syphilis during pregnancy and after delivery as follows: The doctor performs a clinical and serological examination for syphilis using one non-specific and one specific reaction in
- all pregnant women in the third and seventh months of pregnancy,
- the umbilical cord blood of each newborn,
- each woman before the abortion.
In the case of a reactive result for syphilis examination, with the exception of patients with already treated syphilis or without suspicion of relapse or reinfection, the biological material is sent to the National Reference Laboratory for Syphilis established by the Ministry of Health to provide a confirmatory examination. Syphilis is reported.
Newborns of mothers with reactive non-treponemal or treponemal tests should be tested by a quantitative non-treponemal serum serological test (RPR or VDRL), as umbilical cord blood testing may be false positive for maternal blood contamination or false negative wharton umbilical cord jelly. Performing treponemal tests such as TP-PA, FTA-ABS, EIA or CIA is not recommended for infants due to difficult interpretation. None of the commercially available IgM tests are recommended.
Diagnostic criteria according to CDC[edit | edit source]
The Centers for Disease Control and Prevention (2015) developed a list of criteria for diagnosing congenital syphilis.
- Criteria:
- an abnormal physical finding that matches the picture of congenital syphilis OR
- quantitative non-treponemal serum serological test (RPR or VDRL) with a titre 4x higher than in the mother OR
- (absence of 4x higher titer in novo does not rule out the diagnosis of congenital syphilis)
- positive shadow test or positive PCR from lesions or body fluids.
- Recommended additional examinations:
- cerebrospinal fluid examination: VDRL, leukocyte count, protein levels (however, interpretation is difficult in neonates);
- blood count, differential, platelet count;
- according to the clinical picture: long bone X-ray, chest X-ray, liver tests, CNS imaging, ophthalmological examination, hearing examination (BAEP).
- Criteria:
- Possible congenital syphilis
- Criteria:
- Newborn with normal physical findings and a serum quantitative non-treponemic serological titre equal to or less than 4 times the maternal titre A:
- the mother was not adequately treated OR
- the mother was treated with erythromycin or otherwise than recommended by the CDC OR
- the mother was treated less than 4 weeks before delivery.
- Recommended additional examinations:
- cerebrospinal fluid examination: VDRL, leukocyte count, protein levels (however, interpretation is difficult in neonates);
- blood count, differential, platelet count;
- X-ray of long bones.
- Criteria:
- Congenital syphilis unlikely
- Criteria:
- A neonate with a normal physical finding and a serum quantitative non-treponemic serological titre equal to or less than 4 times the maternal titre A
- the mother was properly treated during pregnancy according to the stage of infection and the treatment was administered more than 4 weeks before delivery A
- the mother shows no signs of reinfection or relapse.
- Criteria:
- Congenital syphilis not probable
- Criteria:
- A neonate with a normal physical finding and a serum quantitative non-treponemic serological titre equal to or less than 4 times the maternal titre A
- mother was properly treated before pregnancy
- maternal non-treponemal serological titers remained low and stable before and during pregnancy and childbirth (VDRL <1: 2; RPR <1: 4).
- Criteria:
Note: The BWR or Bordet- (Gengou-) Wassermann reaction is the designation of the first serological diagnostic method using the principle of complement fixation reaction, which dates from the early 20th century.
Therapy[edit | edit source]
- Recommended treatment of pregnant women according to CDC (2015)
- Penicillin G - the only effective prevention of mother-to-fetal infection and treatment of fetal infection;
- in case of penicillin allergy, an attempt at desensitization and subsequent treatment with penicillin is recommended.
- Recommended treatment of newborns according to CDC (2015)
- Proven or highly probable congenital syphilis in the newborn
- Crystalline penicillin G: 100,000-150,000 units / kg / day i.v. - for the first 7 days 50,000 units / kg / dose every 12 hours and from the 8th to the 10th day every 8 hours OR Procaine penicillin G 50,000 units / kg i.m. Once a day for 10 days.
- Possible congenital syphilis in a newborn
- Crystalline penicillin G i.v. OR Procaine penicillin G i.m. OR Benzathine penicillin G 50,000 units / kg i.m. in a single dose.
- Congenital syphilis unlikely
- Benzathine penicillin G 50,000 units / kg i.m. in a single dose OR the newborn can be left untreated and serology checked regularly
- Congenital syphilis not probable
- treatment of the newborn is not indicated, in reactive non-treponemal tests it is necessary to check serology regularly (every 2-3 months) until the tests are negative (titers should decrease by 3 months of age and be non-reactive by 6 months of age if it was only a passive maternal transfer). IgG antibodies).
Decomposition by trepon may lead to the Jarisch-Herxhaimer reaction. It can occur 1-2 hours after the start of therapy, most often in the treatment of the second stage of the disease. The cause is the release of large amounts of thermostable pyrogens from decayed spirochetes. It is manifested by a sharp rise in temperature, chills, myalgias, headaches, tachycardia, hyperventilation, vasodilation and flushing, moderate hypotension. It usually lasts 12-24 hours, then disappears spontaneously. Symptoms can be alleviated by the administration of corticosteroids.
Prevention[edit | edit source]
- Mandatory syphilis screening in all pregnant women.
Links[edit | edit source]
Related articles[edit | edit source]
- Syphilis • Sexually transmitted infections
- Fetal infections : Congenital toxoplasmosis • Congenital listeriosis • HBsAg positive mother and newborn • HIV infection in pregnancy • Importance of chlamydia and mycoplasmas in perinatology • Congenital cytomegalovirus infection • Adnate HSV infection
- Infection in newborns
Externí odkazy[edit | edit source]
Reference[edit | edit source]
- ČGPS ČLS JEP. Principles of dispensary care in pregnancy (Revision of the recommended procedure of the CGPS ČLS JEP No. 1/2019 Coll.) [Online]. © 2021. [feeling. 15.10.2021]. < https://www.pro-kosmeticky.cz/clenove/postupy/doc/2021-01%20-%20Zasady%20dispenzarni%20pece%20v%20tehotenstvi%20-%20DP%20CGPS%20CLS%20JEP%20-%+20REVIZE.pdf >. .
- ↑Jump up to:a b PAVELKA, J, et al. A case of secondary syphilis in a 15-year-old boy. Pediatrics for practice [online] . 2010, vol. 11, vol. 5, pp. 330-332, also available from < https://www.pediatriepropraxi.cz/pdfs/ped/2010/05/11.pdf >.
- ↑Jump up to:a b c d e f g BOŠTÍKOVÁ, V, et al. Selected viral and bacterial perinatally transmissible infections - sexually transmitted infections. Pediatrics for practice [online] . 2015, vol. 16, vol. 1, pp. 37-39, also available from < https://www.pediatriepropraxi.cz/pdfs/ped/2015/01/08.pdf >.
- ↑Jump up to:a b c d e POLIN, Richard and Alan SPITZER. Fetal and Neonatal Secrets. 3rd edition. Elsevier Health Sciences, 2013. 558 pp. 355-357. ISBN 9780323091398 .
- ↑ SPLIT, H and B SPLIT. SCREENING SEROLOGICAL EXAMINATIONS IN GRAVITY. Modern Midwifery [online] . 2006, vol. -, vol. -, p. 3, also available from < https://www.levret.cz/publikace/casopisy/mb/2006-11/?pdf=46 >.
- ↑Jump up to:a b c MUNTAU, Ania Carolina. Pediatrics. 4th edition. Prague: Grada, 2009. pp. 32-34. ISBN 978-80-247-2525-3 .
- ↑Jump up to:a b c BENEŠ, Jiří. Study materials [online]. © 2007. [feeling. 2009]. < http://www.jirben.wz.cz/ >.
- ↑Jump up to:a b c d e f g Centers for Disease Control and Prevention. Congenital Syphilis [online]. © 2015. [feeling. 2019-01-03]. < https://www.cdc.gov/std/tg2015/congenital.htm >.
- ↑Jump up to:a b State Institute of Public Health. Syphilis - Traditional Disease, Contemporary Problem II [online]. © 2007. [feeling. 2019-01-02]. < http://www.szu.cz/tema/prevence/syfilis-tradicni-choroba-soucasny-problem-ii >.
- ↑ https://www.zakonyprolidi.cz/en/2012-306
- ↑ Centers for Disease Control and Prevention. Syphilis During Pregnancy [online]. © 2015. [feeling. 2019-01-03]. < https://www.cdc.gov/std/tg2015/syphilis-pregnancy.htm >.