Congenital hypertrophic pyloric stenosis
From WikiLectures
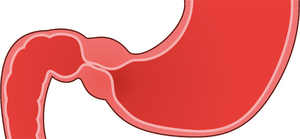
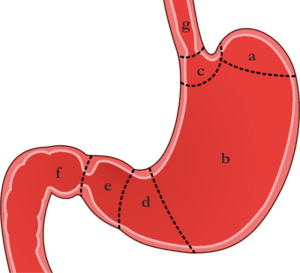
Hypertrophic pyloric stenosis is an acquired diffuse hypertrophy and hyperplasia of the smooth muscle of the pylorus and the entire stomach.
Etiology[edit | edit source]
Etiology is unknown, polygenic inheritance and environment are assumed. Familial occurrence was demonstrated in 15%. It is sometimes associated with hiatal hernia, esophageal atresia or Turner syndrome. The incidence of the disease varies greatly geographically, with around 1:5000 live births in the Czech Republic, it is up to five times more often in first-born boys. Newborns and infants between 3-6 weeks of life are affected. Children older than 3 months are rarely affected.
Clinical picture[edit | edit source]
- Explosive arc vomiting dominates, projectile (up to 1 m);
- Vomit contains acidic gastric juices, usually the content is digested milk, vomit is free of bile;
- there is dehydration, the child has a large appetite, he/she drinks eagerly; he/she loses weight (dehydration, insufficient caloric intake)
- the child is lethargic, has constipated or hungry stools, has an olf-fashioned appearance;
- can lead to severe hypochloremic alkalosis and hypokalemia - severe condition, shallow breathing, loss of consciousness, convulsions - coma pyloricum;
- A peristaltic wave (from left to right epigastrium) can be observed on the abdomen immediately after drinking;
- with gentle palpation, about 70% of children have palpable resistance = olive, the size of a cherry in the epigastrium, to the right of the midline - tumor pylori;
- icterus may occur rarely
Laboratory examination[edit | edit source]
- typically hypochloremic alkalosis with hypokalemia, hyponatremia and dehydration;
- hypochloremia can reach extreme values (below 75 mmol / l), its degree better reflecting potassium loss than potassium;
- elevated gastrin levels
Diagnostics[edit | edit source]
- clinical picture
- abdominal ultrasound
- the length (17 mm and more) and width (4 mm and more) of the pyloric channel are measured
- sensitivity 97%
- X-ray contrast examination (GIT passage) is currently used for diagnostic doubts
- stomach dilatation
- elongated and narrow pyloric canal (so-called rail or shoelace image)
- contrast medium must be aspirated with a nasogastric tube after examination (possible aspiration)
- rapid passage of contrast through the stomach eliminates pyloric stenosis
- this test may reveal other causes of vomiting without bile:
- gastric atony
- delayed gastric emptying,
- gastroesophageal reflux
Differential diagnosis[edit | edit source]
- other causes of explosive vomiting:
- intracranial hypertension,
- pyloric atresia,
- antral membrane,
- stomach duplications,
- gastric atony
- delayed gastric emptying,
- gastroesophageal reflux;
- other causes of similar metabolic breakdown:
- acute adrenal insufficiency - bleeding or congenital hyperplasia - MAc,
- hyperkalemia,
- sodium loss in urine;
- hereditary metabolic disorders – Metabolic alkalosis can cause disorders of AMK metabolism (urea cycle disorder).
Therapy[edit | edit source]
- a conservative approach is not recommended
- the treatment is surgical
- longitudinal pyloromyotomy of hypertrophic pyloric muscle is most often performed (Weber-Ramstedt operation):
- it begins with a transverse laparotomy in the right part of the epigastrium
- the straight abdominal muscles and the oblique abdominal muscles are intersected longitudinally
- after opening the peritoneal cavity, a hypertrophic pylorus is luxated into the surgical wound
- a sharp longitudinal incision is made of serosa and superficial muscle fibers (the incision starts 1-2 mm from the pyloroduodenal junction and ends in the area of the pyloric junction in the stomach)
- the muscle fibers are separated (along the entire length of the incision) by blunt dissection
- complication is perforation of the mucosa - this must be sutured with absorbable material and covered with omentum
- patients with more than 5% weight loss, metabolic alkalosis and hypochloremia must parenterally rehydrate and correct the internal environment within 24 hours before surgery
- longitudinal pyloromyotomy of hypertrophic pyloric muscle is most often performed (Weber-Ramstedt operation):
- can also be performed by laparoscopic technique
- prognosis - good with timely operation.
References[edit | edit source]
Related articles[edit | edit source]
- Esophageal atresia
- Atresia and stenosis of the small intestine
- Anal and rectal atresia
- Superior mesenteric artery syndrome
Source[edit | edit source]
- BENEŠ, Jiří. Studijní materiály [online]. ©2007. [cit. 2010-04]. <http://www.jirben.wz.cz/>.
Literature[edit | edit source]
- HRODEK, Otto a Jan VAVŘINEC, et al. Pediatrie. 1. vydání. Praha : Galén, 2002. ISBN 80-7262-178-5.
- ŠAŠINKA, Miroslav, Tibor ŠAGÁT a László KOVÁCS, et al. Pediatria. 2. vydání. Bratislava : Herba, 2007. ISBN 978-80-89171-49-1.
- ŠNAJDAUF, Jiří a Richard ŠKÁBA. Dětská chirurgie. 1. vydání. Praha : Galén, 2005. ISBN 807262329X.