ADH
ADH (antidiuretic hormone, vasopressin, adiuretin) is a neurosecretory hormone synthesized by the supraoptic and paraventricular nucleus of the hypothalamus and secreted by the posterior lobe of the pituitary gland along with oxytocin.
ADH (osmoreceptors in hypothalamus):
| nc. supraopticus and nc. paraventricularis of hypothalamus | |
| 9 amino acids | |
| collecting ducts | |
| for G-protein-coupled ADH | |
| increase in water resorption in the kidneys by increasing the permeability of cells of the end of DT and collecting ducts | |
| 192340 |
Production[edit | edit source]
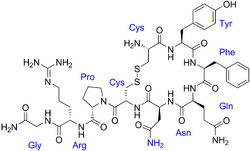
Vasopressin is also produced to a lesser extent in the gonads and in the adrenal glands. It is a cyclic nonapeptide containing a disulfide bond. In humans, it is found in the form of arginine-vasopressin (Arg at position 8). Other mammals, such as hippos or pigs, have lysine-vasopressin.
Function[edit | edit source]
The basic physiological function of the antidiuretic hormone is water resorption in the kidneys, allowing an increase in fluid intake and an increase in blood pressure. ADH increases the permeability of the cells at the ends of the distal tubules and collecting ducts for water and thus its retention in the body. Water channel passage (aquaporins) is a passive process that does not require energy. Reverse resorption works on the principle of osmosis and gives rise to a more concentrated urine even with a smaller volume.
Receptors[edit | edit source]
The effect of vasopressin is mediated by receptors. The antidiuretic effect is provided by V2 receptors, which cause an increase in cAMP levels. This mechanism is based on the transfer of protein channels for water (aquaporins) into the luminaire membranes of the collecting ducts and the subsequent diffusion of water. Another type of receptor is V 1 receptors, which increase the intracellular concentration of Ca2+. These receptors allow the vasoconstrictive effects of vasopressin. They occur, inter alia, in liver, where vasopressin acts glycogenolysis. In the anterior lobe of pituitary gland, these receptors mediate increased secretion of adrenocorticotropic hormone (ACTH).
Regulations[edit | edit source]
Vasopressin affects kidney function very rapidly, but is also rapidly inactivated (biological half-life = 18 min). Thus, increased vasopressin secretion causes an increase in body fluid volume and a decrease in osmolality blood plasma. Thus, an important factor in controlling ADH secretion is plasma osmotic pressure. Secretion is controlled by osmoreceptors located in the hypothalamus, which are also involved in triggering thirst. Another stimulus that promotes vasopressin secretion is extracellular fluid volume. With an increased amount of fluid, secretion is suppressed, a decrease in volume stimulates the secretion of antidiuretic hormone. The increase in secretion thus promotes an increase in osmotic pressure, a decrease in extracellular fluid volume and, in addition, heat, pain, emotions, physical and mental stress, physical exertion, nausea and vomiting, standing, nicotine, morphine, acetylcholine, angiotensin II. In contrast, attenuation of ADH secretion and diuretic effect are caused by factors such as decreased osmotic pressure, increased extracellular fluid volume, cold, adrenaline, alcohol and caffeine.
Clinical correlations[edit | edit source]
Bleeding causes a condition of hypotension and hypovolemia, thereby inducing copious ADH secretion. Insufficient production of vasopressin or inability of the target organs to respond to it manifests a syndrome called diabetes insipidus. A symptom of this is excessive excretion of highly hypotonic urine (polyuria). If the mechanism of thirst is not damaged, this is compensated by extreme fluid intake (polydipsia). Even if the feeling of thirst disappears, fatal dehydration of the body will occur. Another disorder associated with ADH production disorder is the antidiuretic hormone hypersecretion syndrome - SIADH. Patients with this syndrome are at risk of increased fluid intake, which can cause water poisoning. Paradoxically, this syndrome can also cause increased salt release if the volume of extracellular fluid increases so much that it causes a decrease in the secretion of aldosterone responsible for Na+ resorption.
Links[edit | edit source]
Related articles[edit | edit source]
External links[edit | edit source]
References[edit | edit source]
- GANONG, William F. Přehled lékařské fyziologie. 20. edition. Praha : Galén, 2005. 890 pp. ISBN 80-7262-311-7.
- LEDVINA, Miroslav – STOKLASOVÁ, Alena – CERMAN, Jaroslav. Biochemie pro studující medicíny. 2. edition. Praha : Karolinum, 2009. ISBN 80-246-0851-0.