Syndrome of inappropriate antidiuretic hormone secretion
The syndrome of inappropriate antidiuretic hormone secretion, Schwartz-Bartter syndrome ( SIADH ) , is characterized by increased secretion of ADH (vasopressin), which is not dependent on plasma osmolality . Most children have lung or intracranial disease, and this syndrome can also occur iatrogenically (treatment of enuretics with adiuretin). Patients have normovolemia or relative hypervolemia. There is dilute hyponatremia , serum hypoosmolality . Urinary sodium loss is slightly higher, certainly not reduced. It has low uremia and increased urikosurie .
Etiology[edit | edit source]
- CNS disorders: meningitis , encephalitis , brain abscess , tumor, trauma / bleeding , hydrocephalus
- malignancies: Hodgkin 's disease , neuroblastoma , tumors of the lung , GIT and uropoietic tract
- pulmonary involvement: pneumonia , TB , UPV , PNO , acute respiratory insufficiency , chronic obstructive pulmonary disease
- drugs: DDAVP, paracetamol , indomethacin, barbiturates, carbamazepine, indapamide, SSRIs, donepezil, thiazide diuretics
Physiology[edit | edit source]
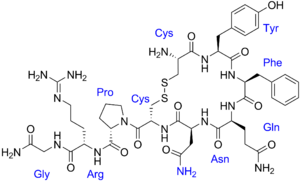
ADH (antidiuretic hormone) , also known as arginine-vasopressin (AVP), is a nonapeptide that is synthesized in ncl cells . supraopticus a ncl . paraventricular hypothalamus. It is transported by axonal transport to the neurohypophysis , from where it is released, along with the neurophysin transport protein, in response to a change in serum osmolality. A change in osmolality of ≥ 2% is already detected by osmoreceptors in the hypothalamus . Increased osmolality leads to an increase in ADH secretion and conversely a decrease in serum osmolality leads to suppression of ADH secretion. In the kidneysADH increases the permeability of the terminal part of the distal tubule and the collecting ducts in the marrow region through the induction of specific membrane transport channels for water - aquaporins .
Pathophysiology[edit | edit source]
SIADH was first described by Schwartz in 1957. SIADH results in excessive release of ADH from the neurohypophysis (intracranial disease, drug induction: barbiturates, carbamazepine) or ectopic production of ADH (tumors: lymphomas , Ewing's sarcoma ). Elevated levels of ADH occur in pathological conditions that are associated with redistribution of blood in the vascular bed with subsequent hypovolemia in the area of large vessels in the chest and in the left atrium. In bacterial and viral pneumonias, emphysema , cystic fibrosis , UPV causes increased pulmonary vascular resistance, decreased left atrial filling and increased ADH levels.
Increased ADH secretion causes water reabsorption in the renal collecting tubules. This tends to expand both intravascular and extravascular volume . This tendency is compensated by the increased secretion of the atrial natriuretic peptide , so we find increased natriuresis despite the low plasma sodium level. However, the cause of increased natriuresis in SIADH is not fully elucidated; other options for increased natriuresis include increased glomerular filtration and decreased aldosterone secretion . And it is the presence of higher natriueza that is the basic problem in distinguishing SIADH from CSWS .
SIADH is accompanied by a slight increase in body water volume. An immediate response to the rapid decrease in osmolality of extracellular fluids is the passive transfer of water from the extracellular space to the more hypertonic intracellular. This leads to an expansion of the volume of organ cells ( brain swelling ). Because most of the excess body water is found intracellularly, hypehydration does not manifest itself clinically for a long time.
Diagnostics[edit | edit source]
Traditional SIADH criteria:
- S-Na < 130 mmol/l
- S-osmolalita < 280 mOsmol/l
- U-Na > 20 mmol/l
- U-osmolalita > S-osmolalita
- normal thyroid , kidney and adrenal function
- absence of peripheral edema or dehydration
Serum contains hyponatremia, hypoosmolality, normal or decreased potassium , urea, creatinine , uric acid . U-Na> 20 mmol / l (however, at low sodium intake, losses may be significantly lower). Intravascular volume is normal or slightly increased. Patients are normotensive. Another laboratory finding may be MAC with decreased AG , but not compensatory hypocapnia .
In case of doubt in the diagnosis, determination of serum or urinary ADH concentration can be used. Under normal circumstances, ADH cannot be detected in hyponatremic conditions; on the contrary, we demonstrate increased levels in SIADH. However, we must interpret ADH levels carefully, because ADH secretion is not only affected by osmolality, but also by stress, pain, increased intracranial pressure , etc.
Another possibility is to determine the serum concentration of copeptin , which is excreted together with ADH in equimolar amounts, but is more stable than ADH.
Clinical Picture[edit | edit source]
Clinical signs are a manifestation of cerebral edema . During an acute course, lethargy, apathy, disorientation, nausea, vomiting , muscle cramps , decreased deep muscle reflexes, pathological reflexes and Cheyne-Stokes breathing occur . If hyponatremia develops over several days and weeks, the patient may be asymptomatic or with non-specific symptoms such as nausea, vomiting or lethargy. Rhabdomyolysis may rarely occur .
Symptomatology is not given by the absolute value of sodium, but by the rate of its decline. This must be kept in mind during treatment. Prolonged hyponatremia must be corrected slowly, whereas acute neurological symptoms require prompt intervention.
Therapy[edit | edit source]
In the case of a chronic course, it is usually sufficient to restrict fluids to 2/3 (or less) daily needs and after sodium substitution. In acute conditions and critical value of sodium Na <120 mmol / l we administer 1/1 FR or hypertonic solutions (eg 3% NaCl 3 to 5 ml / kg iv as a slow bolus) + furosemide 1-2 mg / kg iv (can be repeated according to the response and the state of the internal environment). As soon as the acute symptom subsides, we return to fluid restriction. The long-term goal of treatment is to correct hyponatremia within 48 hours. It is essential to eliminate the root cause.
The condition of treatment is monitoring of body weight, diuresis and internal environment, including correction of sodium and osmolality in serum and urine.
Another possibility is the use of vaptans - eg tolvaptan.
| Pediatricians must keep in mind that hypoosmolar syndrome can also be caused iatrogenically by supplying more 5% or 10% glucose without ions! |
Links[edit | edit source]
Source[edit | edit source]
- HAVRÁNEK, Jiří: SIADH, syndrome of inadequate ADH secretion . (managed)
- JAVORKA, Kamil. Medical physiology: a textbook for medical faculties. 2nd edition. Martin: Osveta, 2006. ISBN 8080632316 .
- RUDNAY, Maroš, Petra HRABČÁKOVÁ and Ivica LAZÚROVÁ. Hyponatremia in the syndrome of inappropriate vasopressin secretion (SIADH) - treatment options. Indoor Medicine. 2012, vol. 58, vol. 1, p. 52-55,
- VOKURKA, Martin and Jan HUGO, et al. Great medical dictionary. 9th edition. Prague: Maxdorf, 2009. 1159 pp. ISBN 978-80-7345-202-5 .
- CZECH, Richard, et al. Internal. 2nd edition. Prague: Triton, 2015. 909 pp. ISBN 978-80-7387-895-5 .
Related Articles[edit | edit source]
- Cerebral Salt Loss Syndrome (CSWS)
- Indoor environment (pediatrics) • Serum osmolality • Sodium imbalance (pediatrics)
- ADH