Rh system
Rh is a blood group, which antigens occurs only on erythrocytes. It is highly polymorphic- so far more than 40 serologically distinct Rh antigens have been identified.
Genetics[edit | edit source]
The control region of the expression of Rh antigens, is located on a short arm of the 1. chromosome. It consists of two closely related structural genes RHD and RHCE, which encode antigen-bearing membrane proteins D, d, C, c, E, e. Among the mentioned genes there is applied a very strong gene bond – a combination of alleles of both genes is transferred from generation to generation together – haplotype.
The most important is antigen D – which determines the Rh positivity (Rh+). Rh negative individuals (Rh-) are recessive homozygous (genotype dd) – approximately 17 % of Europe's population. The presence of D antigen cannot be serologically demonstrated, which is due to the deletion of the D gene in the Rh region of DNA.
Antigens C, c, E, e are not so strong and so significant as antigen D, despite this they can provoke a production of antibodies in case of incompatibility. Expression of the antigens C, c, E, e is controled by one gene and is a result of an alternative splicing of the primary transcript of RHCE gene. They appear as separate antigens on the plasma membrane of the erythrocyte. Amongst the alleles C/c a E/e is Codominance.
Antibodies[edit | edit source]
In the Rh system, antibodies do not occur naturally. (unlike in AB0 system). This means that, Rh- individuals do not have antibodies against antigen D. However antibodies can be produced in case of long-lasting (prolonged) contact with the RH+ blood, f.e. prolonged incompatible blood transfusion or pregnancy of Rh- mother bearing a Rh+ child.
Rh incompatibility in blood transfusion[edit | edit source]
The formation of antibodies in the body may be conditioned by the incompatibility of Rh factor with Blood transfusions. In this case is Rh+ blood administered to Rh -recipient. Following such a transfusion, anti-Rh antibodies are formed in the body and upon the every subsequent incompatible transfusion, the body's response is much greater.
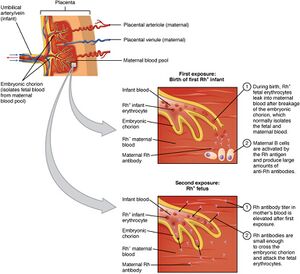
Rh incompatibility of mother and fetus[edit | edit source]
Another option for formation of the Rh antibodies is an incompatibility of the mother and fetus. In this case the mother is Rh- and the fetus is Rh+ (after the father). When fetal erythrocytes enter the maternal circulation (placenta separation during childbirth) D antigens stimulate the production of anti-D antibodies. At first, just IgM antibodies ,which are not able to permeate placenta. However in 72 hours the mother will start to produce type IgG antibodies, which are capable of permeating through placenta. Mother's antibodies permeate through placenta and a cause hemolysis of the fetal erythrocytes.
Sensitization of Rh- mother usually occurs after the delivery (during the delivery placenta is separated and some amount of the fetal blood penetrates into the maternal blood circulation). The first child is by rule not handicapped, however the risk increases with every next delivery or abortion.
Another symptoms of fetal damage include:
- hemolytic anaemia
- icterus (accumulation of bilirubin in the blood, damages the CNS when a certain limit is exceeded)
- fetal erythroblastosis (in tough cases fetus die in utero)
Fetal damage can be prevented by administration of the anti-D antibodies to mother 72 hours after a sensitizing dose of Rh-positive erythrocytes (after delivery or invasive prenatal diagnosis).
Links[edit | edit source]
Related articles[edit | edit source]
- AB0 system
- Blood groups
- Heredity of blood group systems
- Hemolytic disease of the newborn
- Hyperbilirubinemie in newborns and infants
- Exchange transfusion
Bibliography[edit | edit source]
- ŠTEFÁNEK, Jiří. Medicína, nemoci, studium na 1. LF UK [online]. [cit. 2009]. <https://www.stefajir.cz/>.
- KITTNAR, Otomar, et al. Lékařská fyziologie. 1. vydání. Praha : Grada, 2003. 790 s. ISBN 978-80-247-3068-4.
- HÁJEK, Zdeněk, Evžen ČECH a Karel MARŠÁL, et al. Porodnictví. 3. vydání. Praha : Grada, 2014. 538 s. ISBN 978-80-247-4529-9.