Pharmacological possibilities of influencing diabetes
Type 1 diabetes mellitus therapy[edit | edit source]
Therapies vary widely from type to type of diabetes. While in type 1 diabetes we rely on insulin therapy, in type 2 diabetes diet or oral antidiabetic drugs are used depending on the degree of insulin resistance and insulin therapy we use in the more severe cases. The cornerstone of the treatment of type 1 diabetes is insulin substitution, which must be supplemented with alimentary and regimen restrictions.
Cooperation between the doctor and the patient is necessary since an individual treatment plan is drawn up for the patient, consisting of:
- dietary regimen with detailed instructions;
- lifestyle changes;
- education;
- psychosocial care;
- pharmacological treatment of diabetes and associated diseases;
- regular checks.[1]
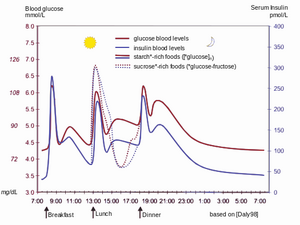
We start insulin therapy on an ambulance check or during hospitalization. We always apply a lower dose at the beginning to hypoglycaemia, as endogenous insulin secretion still persists. We collect a large glycemic profile which consists of glycemia always before and after meals, at 10 pm and at 3 a.m. at night. Based on regular glycemic profiles, we adjust the dosage to adjust the optimal compensation.
Insulins are not binding to plasma proteins in the bloodstream, so they quickly leave circulation and bind to insulin receptors. Exogenous insulin is more than 60% degraded in the kidneys, the rest of the degradation is carried out in the liver (unlike endogenous insulin, which is degraded for the most part in the liver). Only a small part of the insulin administered is excreted in the urine in an unchanged form.
Types of insulins by origin[edit | edit source]
Animal insulins are used the longest, previously isolated from beef or pork pancreas, today monocomponent and highly purified. Beef insulin differs by three, pork one amino acid from human insulin. Due to the risk of BSE beef insulins are no longer used.
Human insulin has been prepared through recombinant DNA transfer technologies to Escherichia coli. Compared to animal insulins, human insulin is a more polar substance, has faster absorption from the place of application and has shorter action. While applying human insulin will better replicate the physiological function of this hormone, we will mask some of the warning signs of hypoglycaemia that are otherwise present when we applicate animal insulins.
Insulin analogues are also used, which are biosynthetic differing in order of amino acids and pharmacokinetics.
Types of insulin according to the duration of action[edit | edit source]
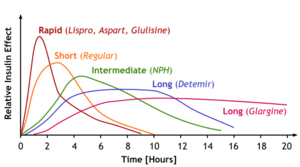
Insulins with different duration of action have been developed to compensate for diabetes properly.
Short-acting insulins[edit | edit source]
Short-term insulins are produced to cope with acute hyperglycaemia situations as well as for intensified insulin therapy as clear water-soluble solutions of crystalline insulin complexes with zinc with neutral pH. For acute intervention in case of hyperglycemic ketoacidosis coma and during anaesthesia or other extreme loads in diabetics can also be applicated intravenously, which has almost immediate effect. As part of the intensified insulin therapy, it is then applicated subcutaneously, when it works within 15-30 minutes, the peak of the action takes 1-3 hours and lasts 4-6 hours. Short-acting insulins include:
- Insulin lispro – its advantage is less propensity to produce hexamer and dimers, which facilitates absorption and accelerates the onset of action. Therefore, it can be applied just before meals, and due to its short effect, the risk of hypoglycemia is reduced.
- Insulin aspart – has similar properties to insulin lispro.
Medium-acting insulins[edit | edit source]
These are cloudy suspensions (mixtures of crystalline and non-crystalline insulin) that are intended only for subcutaneous application.
- Amorphous insulin: a mixture of pork or human insulin with particles of 2 μm with a duration of action of 8-12 hours.
- Zinc-insulin suspension: 330% amorphous insulin and 70% crystalline insulin, the effect lasts differently (from 7 to 24 hours).
- Isophan insulin (NPH insulin or protamine-zinc-insulin): protamine is a mixture of peptides isolated from sperm from river trout. The ratio of protamine molecules to insulin is about 1:6.
- Stabilized insulin mixtures are mixtures of short-acting insulin and insulin isophan. The advantage is a rapid onset and prolonged effect.
Long-acting insulins[edit | edit source]
These insulins are slowly absorbed as they contain large zinc-insulin crystals, so their effect takes slowly but also lasts for a long time (26-28 hours). They are applied subcutaneously, exceptionally intramuscularly. For example, insulin glargine, which has a duration of action of up to 36 hours, is used and must not be mixed with other insulins in one syringe for large crystals.
Schemes[edit | edit source]
Conventional schemes[edit | edit source]
If a certain degree of endogenous insulin secretion is still maintained, the following schemes are used:
- Two-dose scheme: fast and moderate-acting insulin in two daily doses, of which 2/3 of the total daily dose in the morning and 1/3 in the evening.
- Three-dose mode:
- morning: fast insulin + medium-speed insulin,
- before dinner: fast insulin,
- before going to bed: moderate insulin.
Intensified schemes[edit | edit source]
In patients with Type 1 DM, we strive to ensure that the exogenous delivery of insulin best replicates the secretion of insulin from the pancreas of healthy people. These schemes are also used for DM 2nd type with the complicated course.
- Scheme to quickly compensate for diabetes, suitable even for more lymable diabetes: short-acting insulin before the main meals, medium-acting insulin before bedtime.
- Basal-bolus scheme: short-acting insulin before main meals and long-acting insulin in one or two daily doses.
- Schedule of short-acting insulin in at least four daily doses.
- Insulin pump: continuous subcutaneous infusion of fast-acting insulin.
Methods of insulin administration[edit | edit source]
Insulin is given as an injectable solution, most often subcutaneously (rapid insulin can also be given intravenously). Since insulin therapy is permanent, it is necessary to instruct patients accurately and teach them the technique of application so that their diabetes is fully compensated. To apply insulin is used:
Cathegory:Pharmacology Cathegory:Endocrinology Cathegory:Internal Medicine
Type 2 diabetes mellitus therapy[edit | edit source]
Non - pharmacological therapy[edit | edit source]
- diet
- physical activity
- bariatric treatment
Oral antidiabetics[edit | edit source]
Oral antidiabetics (PADs) are drugs used in the treatment of diabetes mellitus. The mechanism of their action depends on the production of endogenous insulin and therefore cannot be used in patients with type 1 diabetes.
According to the place of operation, PAD can be divided into 4 groups:
- insulin sensitisers - increase the sensitivity of cells to insulin (biguanides, thiazolidinedionesState Office for Drug Control ATC group: A10BG);
- insulin secretagogue - increase insulin delivery from pancreatic β-cells (sulfonylurea derivativesState Office for Drug Control ATC group: A10BB, glinides);
- intestinal glucosidase inhibitors - reduce intestinal glucose absorption - alpha-glucosidase inhibitorsState Drug Administration ATC Group: A10BF;
- proximal tubule glucose reuptake inhibitors - increase glycosuria (gliflosins).
Insulin sensitizers[edit | edit source]
They increase the sensitivity of cells to insulin. They do not cause hypoglycaemia and are therefore referred to as "euglycaemic drugs"
Biguanides
Metformin is the basic PAD today. It is well tolerated and can be advantageously combined with other antidiabetics. It reduces cardiovascular mortality by 50% and has positive late effects of treatment (it is advisable to start treatment already in the period of prediabetes). It does not cause weight gain (unlike secretagogues and thiazolidinediones), so it is also beneficial for obese patients.[2] It is a cheap drug without a prescription restriction.
Mechanism of action
They increase the sensitivity of tissues (especially liver and skeletal muscle) to insulin and reduce blood glucose:
- promoting glucose utilization in skeletal muscle and adipose tissue (by stimulating glycolysis),
- attenuation of gluconeogenesis in the liver,
- by reducing the absorption of glucose from the gut.
Side effects
They support glycolysis and thus lactate production. Thus, lactic acidosis can be a serious complication. Individuals with failing kidneys, cardiopulmonary insufficiency, liver insufficiency (alcoholics) are predisposed to this. In these cases, biguanides are contraindicated.
Gastrointestinal problems may occur at the beginning of treatment.
Intravenous administration of an iodinated contrast agent may lead to renal failure. This may cause accumulation and increase the risk of lactic acidosis. Therefore, biguanide use must be discontinued 48 hours before the examination. They are also discontinued before surgery.
They are not recommended for the treatment of diabetes during pregnancy. Insulin should be used to maintain blood sugar levels to minimize the risk of fetal malformations.
Thiazolidinediones
Mechanism of action
They have similar effects as biguanides. Through the nuclear receptor, PPAR-γ activates the transcription of genes responsible for carbohydrate and fat metabolism.
Side effects
They cause mild fluid retention (therefore diuretics are sometimes added), therefore they are not used in patients with heart failure, edema conditions, during pregnancy. Pioglitazone is contraindicated in haematuria of unclear origin. They require regular liver function tests. There is often an increase in weight (fluid retention, increase in adipose tissue). An eye examination is also appropriate before use, due to the risk of worsening diabetic macular edema.
Today, only one pioglitazone is used (rosiglitazone does not have a beneficial effect on cardiovascular mortality and is currently withdrawn from the market [4]), it is well tolerated, it is suitable for the contraindication of metformin.
Insulin secretagogue[edit | edit source]
They increase insulin delivery from pancreatic β-cells.
They are risky in terms of possible induction of hypoglycemia and cause weight gain.
Sulphonylureas Mechanism of action Increased insulin release from pancreatic β-cells is achieved by blocking ATP-sensitive K + channels in the membrane. This reduces the flow of potassium from the cell, depolarizes the membrane and opens Ca2+ channels. Penetrating Ca2+ ions cause insulin to wash out.
Side effects The most serious complication may be hypoglycaemia, especially with longer-acting substances. This group of drugs also increases appetite, so treatment is often associated with weight gain.
Drugs II are used in practice. generation (glipizide) and III. generation (glimepiride). Most often in combination therapy with metformin (especially in case of insufficient compensation of type II DM monotherapy with metformin).
Glinides Newer drugs also block the ATP-sensitive K + channel in β-cell membranes. They work quickly, making them ideal for use with food to compensate for postprandial hyperglycemia. Examples of substances are repaglinide and nateglinide.
Intestinal glucosidase inhibitors[edit | edit source]
They are used to control postprandial hyperglycemia. The basic substance used in this group is acarbose.
Mechanism of action
By inhibiting enzymes, they reduce and slow down the absorption of carbohydrates in the small intestine. The blocked enzyme does not cleave them and therefore cannot be resorbed (absorption of monosaccharides remains unchanged).
Side effects
Flatulence, diarrhea and abdominal pain caused by the action of microbial intestinal flora on undigested compound carbohydrates.
If a patient develops hypoglycaemia due to other medications, they cannot be treated orally with sucrose but only glucose.
Gliflozins[edit | edit source]
Mechanism of action
They inhibit the SGLT-2 transporter in the proximal tubule of the nephron, thereby blocking glucose reuptake and increasing glycosuria. Thus, the renal threshold for glucose is shifted and blood glucose is lowered. Increased glucose losses lead to energy loss and weight loss. At the same time, they reduce glycated hemoglobin, uricaemia, slightly increase HDL cholesterol and, due to osmotic diuresis, a slight decrease in blood pressure.
Side effects
Increasing the frequency of urogenital tract infections. These are most often fungal infections in women. Due to increased diuresis, caution should be exercised in patients at risk of hypotension or volume depletion.
The risk of hypoglycaemia is minimal with gliflozin.
In the Czech Republic dapagliflozin, canagliflozin and empagliflozin, is available.
Incretins[edit | edit source]
Incretin-modulating agents can now be used in the treatment of type 2 diabetes. They are very effective, safe, but expensive. They increase insulin secretion, inhibit glucagon and act only in hyperglycemia.
Exenatide is a synthetic analogue of GLP-1 (glucagon-like peptide 1), an analogue of incretins. It applies s. C., So it does not belong to the PAD.
Dipeptidyl peptidase 4 (DPP-4) inhibitors block an enzyme that inactivates endogenous incretins. They are less effective than incretin analogues, but are cheaper and orally administrable. Example of a substance: sitagliptin, inagliptin.
Links[edit | edit source]
Related Articles[edit | edit source]
- Diabetes mellitus
- Type 1 diabetes mellitus (endocrinology)
- Type 1 diabetes mellitus (biochemistry)
- Type 2 diabetes mellitus (endocrinology)
- Type 2 diabetes mellitus (biochemistry)
- Insulin
Reference[edit | edit source]
- CZECH, Richard, et al. Internal. 1st edition. Prague: Triton, 2010. 855 pp. 233. ISBN 978-80-7387-423-0.
- TREVOR, Anthony J. Katzung & Trevor's pharmacology: examination & board review. 10th ed. New York: McGraw-Hill Medical, c2013. a LANGE medical book. ISBN 978-0-07-178923-3.
- SUCHOPÁR, Josef, VALENTOVÁ, Štěpánka, ed. Remedia compendium. 4th edition Prague: Panax, 2009. ISBN 978-80-902806-4-9.
- SCHEEN, A J. [Suspension of the commercialization of sibutramine and rosiglitazone in Europe]. Rev Med Liege [online]. 2010, vol 65, no. 10, pp. 574-9, also available from <https://www.ncbi.nlm.nih.gov/pubmed/21128363>. ISSN 0370-629X.
- SANUSI, Himawan. The role of incretin on diabetes mellitus. Acta Med Indones [online]. 2009, vol 41, no. 4, pp. 205-12, also available from <https://www.ncbi.nlm.nih.gov/pubmed/20737753>. ISSN 0125-9326.
Used literature[edit | edit source]
- LINCOVÁ, Dagmar – FARGHALI, Hassan. Basic and applied pharmacology. 2. edition. Galen, 2007. 0 pp. ISBN 978-80-7262-373-0.
- CZECH REPUBLIC, Richard. Internal. 1. edition. Triton, 2010. 855 pp. ISBN 978-80-7387-423-0.
- ↑ ČEŠKA, Richard. Interna. 1. edition. Praha : Triton, 2010. 855 pp. pp. 233. ISBN 978-80-7387-423-0.