Neonatal cholestasis
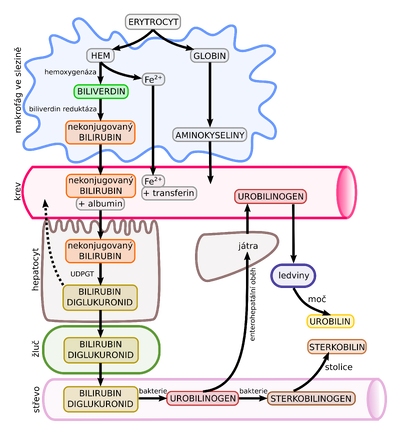
Neonatal cholestasis is conjugated hyperbilirubinemia that appears in the first months of life (i.e. in the neonatal period or shortly after). Cholestasis is the result of reduced production and/or excretion of bile due to a number of causes.
Cholestasis is defined as the impairment of bile excretion based on a disorder of intrahepatic bile production, transmembrane transport of bile, or mechanical obstruction of bile flow. The biochemical consequence is an increased serum level of bile components, i.e. of conjugated bilirubin, bile acids and/or cholesterol.
Conjugated hyperbilirubinemia or direct hyperbilirubinemia (as determined by direct van den Bergh reaction with diazotized sulfanilic acid) is definedd as an elevated level of conjugated/direct bilirubin above 17 μmol/L ( 1 mg/dl) with total bilirubin < 85.5 μmol/L (5 mg/dl) or above 20% with total bilirubin > 85.5 μmol/L (5 mg/dl).[1]
Causes[edit | edit source]
Causes of neonatal cholestasis:
- Obstructive (biliary atresia - progressive idiopathic disease of the extrahepatic bile ducts; biliary cysts; thickened bile syndrome; gallstones or sludge; tumors; neonatal sclerosing cholangitis);
- Infectious (cytomegalovirus, toxoplasmosis, rubella, herpes, syphilis; less often echovirus, adenovirus, parvovirus B19, E. coli);
- Metabolic/genetic, toxic, alloimmune (Alagillo syndrome; galactosemia, tyrosinemia, progressive familial intrahepatic cholestasis, disorders of lipid metabolism, disorders of bile acid metabolism, mitochondrial disease, citrin deficiency, alpha-1 antitrypsin deficiency; ARC syndrome - arthrogryposis, renal dysfunction, cholestasis; neonatal hemochromatosis - gestational alloimmune liver disease; cystic fibrosis; liver disease associated with intestinal failure - intestinal failure-associated liver disease, IFALD; idiopathic neonatal hepatitis).
Early diagnosis of biliary atresia is crucial, as early surgical intervention improves the prognosis. Early diagnosis of treatable causes - tyrosinemia, galactosemia, hypothyroidism and infection - is also important.[2]
Links[edit | edit source]
Related articles[edit | edit source]
References[edit | edit source]
- ↑ LOOMES, K M – ERLICHMAN, J. Approach to evaluation of cholestasis in neonates and young infants [online]. UpToDate, ©2020. The last revision 2018-02, [cit. 2020-07-25]. <https://www.uptodate.com/contents/approach-to-evaluation-of-cholestasis-in-neonates-and-young-infants>.
- ↑ ERLICHMAN, J – LOOMES, K M. Causes of cholestasis in neonates and young infants [online]. UpToDate, ©2020. The last revision 2020-04, [cit. 2020-07-25]. <https://www.uptodate.com/contents/causes-of-cholestasis-in-neonates-and-young-infants>.