Congenital Cytomegalovirus Infection
Congenital CMV infection affects about 1-2% of live births. About 90% of them are asymptomatic at birth, but 5-10% of children develop hearing problems in preschool age.[1]
Etiopathogenesis[edit | edit source]
Cytomegalovirus or HHV-5 is a widespread virus of the Herpesviridae family. It is transmitted mainly by body fluids (saliva, urine, blood, tears, semen, cervical secretion, and breast milk) and is one of the sexually transmitted infections. It can be transferred from mother to fetus transplacentally. CMV infection is most often asymptomatic, but may be accompanied by fever, sore throat, malaise, swelling of the glands, or may manifest as mononucleosis or hepatitis. After infection, the virus remains in the body for life and may be reactivated or infected with another type of CMV.
During pregnancy, maternal primary infection, reactivation of the infection, or infection with another strain of CMV (so-called non-primary infection) infection may occur.
CMV is transmitted to the fetus/newborn transplacentally, during delivery from infected birth canals, or postnatally from infected breast milk. Transplacental transmission is significantly more common during primary infection in the first half of pregnancy. It can also be transmitted to the newborn by blood derivatives, so blood from seronegative donors, frozen in glycerol, or depleted of leukocytes, is given.Cite error: The opening <ref> tag is malformed or has a bad name
Clinical Picture[edit | edit source]
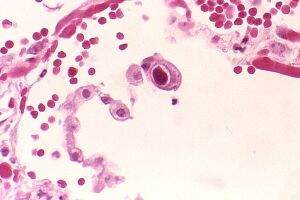
CMV-infected cell in microscopic image: enlarged cell with intranuclear inclusions. CMV crosses the placenta and the blood-brain barrier. CMV infection in early pregnancy has teratogenic potential, it can cause e.g. neuronal migration disorders. CMV can be transmitted to the fetus in both primary and non-primary maternal infections; the risk of congenital CMV infection is significantly higher in maternal primary infections (fetal infection occurs in about one-third of cases). Infection of the placenta leads to its inflammation and impaired function, i.e. impaired ability of the fetus to supply oxygen and nutrients. Fetal viraemia leads to multiorgan damage (especially CNS, eyes, liver, lungs, kidneys).[2]
Congenital cytomegal infection is asymptomatic at about 90% at birth, with about 10% of some of the following symptoms:
- petechiae, purpura;
- intrauterine growth restriction;
- hepatosplenomegaly;
- jaundice;
- mikrocefaly, intracranial calcifications;
- (chorio)retinitis.
Newborns with symptomatic CMV infection have a mortality rate of 20-30%.[2]
In preschool age, it manifests as unilateral or bilateral sensorineural hearing loss of various severity. It develops in about a third of children with symptomatic CMV infection and in about 10% of children asymptomatic at birth. It can progress up to 7 years of age.Cite error: The opening <ref> tag is malformed or has a bad name
In addition to hearing loss, long-term consequences of congenital CMV infection include psychomotor retardation, visual disturbances, microcephaly, and convulsions. These problems are more common in children with a symptomatic course at birth.[3]
Diagnostics[edit | edit source]
Detection of CMV DNA in urine in the first 2-4 weeks of life by PCR.Cite error: The opening <ref> tag is malformed or has a bad name
Congenital CMV can be retrospectively demonstrated by additional examination of the screening card (i.e. from a "dry drop") by PCR, but the examination has low sensitivity.[2]
Therapy[edit | edit source]
In symptomatic congenital CMV infection affecting the CNS, parenteral administration of ganciclovir for 6 weeks is likely to improve the prognosis. Oral administration of valganciclovir is also possible. Neutrophil levels should be monitored during treatment with ganciclovir due to the risk of developing significant neutropenia.Cite error: The opening <ref> tag is malformed or has a bad name
Links[edit | edit source]
Related Articles[edit | edit source]
- Infectious mononucleosis • Cytomegalovirus
- TORCH infections: Congenital Syphilis • Congenital Toxoplasmosis • Congenital Listeriosis • HBsAg positive mother and newborn • HIV infection during pregnancy • The Importance of Chlamydia and Mycoplasma Infections in Perinatology • Neonatal HSV Infection
- Neonatal infections
Externí odkazy[edit | edit source]
Reference[edit | edit source]
- ↑ name=NeoSecrets2013>POLIN, Richard – SPITZER, Alan. Fetal and Neonatal Secrets. 3. edition. 2013. pp. 359-360. ISBN 9780323091398.
- ↑ a b c GOMELLA, TL. Neonatology : Management, Procedures, On-Call Problems, Diseases, and Drugs. 7. edition. 2013. pp. 615. ISBN 978-0-07-176801-6.
- ↑ https://www.cdc.gov/cmv/clinical/congenital-cmv.html