Diagnosis of Helicobacter Pylori Infection
Helicobacter pylori is a Gram-negative, microaerobic human pathogen, and H. pylori infection is strongly related to many gastroduodenal diseases including chronic active gastritis, peptic ulcer diseases, atrophic gastritis, mucosa-associated lymphoid tissue (MALT) lymphoma, and noncardia gastric cancer (In 1994, H. pylori was recognized, as the only bacteria, as a type I carcinogen, and now it is considered the most common etiologic agent of infection-related cancers). H. pylori infection affects more than half of the adult population worldwide, but the prevalence of H. pylori infection varies widely by geographic area, age, race, and socioeconomic status.
Accurate diagnosis of Helicobacter pylori infection is a crucial part of the effective management of many gastroduodenal diseases. Several invasive and non-invasive diagnostic tests are available for the detection of H. pylori and each test has its usefulness and limitations in different clinical situations. Although none can be considered as a single gold standard in clinical practice, several techniques have been developed to give more reliable results.
Invasive testing[edit | edit source]
Invasive tests are performed via endoscopic biopsy specimens and these tests include histology, culture, rapid urease test as well as molecular methods. Developments of endoscopic equipment also contribute to the real-time diagnosis of H. pylori during endoscopy.
- The culture - the microbiological culture from endoscopy-based gastric biopsies, is considered a definite proof for H. pylori investigation. The culture of H. pylori from the gastric biopsy is characterized by a high specificity with low sensitivity. The culture has 100% specificity, but with significant variation regarding sensitivity ranging from 85% and 95%
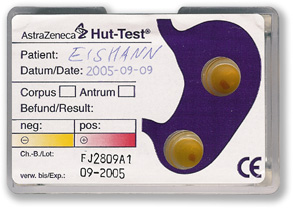
- Rapid urease test (RUT) - The basis of the test is the ability of H. pylori to secrete the urease enzyme, which catalyzes the conversion of urea to ammonia and carbon dioxide → the change of color from the original yellowish color to a red through 24 hours is reflecting the positivity of the test.
Non-invasive testing[edit | edit source]
Urea breathing test and stool antigen test are the most widely used non-invasive tests, whereas serology is useful in screening and epidemiological studies. Molecular methods have been used in variable specimens other than gastric mucosa. More than detection of H. pylori infection, several tests are introduced into the evaluation of virulence factors and antibiotic sensitivity of H. pylori, as well as screening precancerous lesions and gastric cancer.
- Urea Breath test (UBT) - the patient drinks 14C- or 13C-labelled urea, which the bacterium metabolizes, producing labeled carbon dioxide that can be detected in the breath. It is the first-choice test because of its specificity and sensitivity.
- Stool antigen test (SAT) is the other noninvasive method with good sensitivity and specificity
- Antibody-based test - numerous serological tests based on the detection of anti-H. pylori IgG antibody in patient's saliva or urine samples are widely available for H. pylori diagnosis
- However, the serological test is not a reliable test to assess eradication therapy because antibody levels can persist in the blood for long periods of time even after successful eradication[
GastroPanel[edit | edit source]
GastroPanel is a first-line non-invasive diagnostic blood test for dyspeptic patients. It gives information on the structure and function of the stomach mucosa, and of the risks caused by a possible abnormal inner lining. Based on the results, it is possible to get information to support the diagnosis of:
- Healthy stomach mucosa
- Functional and organic dyspepsia (when GastroPanel results indicate a healthy stomach mucosa, the cause of stomach problems is often functional dyspepsia or disease outside the stomach)
- Atrophic gastritis (damaged stomach mucosa that is severely dysfunctional) and likelihoods of the conditions specifically in the corpus and antrum areas of the stomach (normal, gastritis, or atrophic gastritis)
- Helicobacter pylori infection
- Achlorhydria of the stomach (anacidic stomach)
The test panel consists of four assays:
- Pepsinogen I ELISA
- Pepsinogen II ELISA
- Gastrin-17 ELISA
- Helicobacter pylori IgG ELISA
Links[edit | edit source]
Related articles[edit | edit source]
Reference[edit | edit source]
- with permission of the author
KOCNA, Petr. GastroLab : MiniEncyklopedie laboratorních metod v gastroenterologii [online]. ©2002. The last revision 2011-01-08, [cit. 2011-03-04]. <http://www1.lf1.cuni.cz/~kocna/glab/glency1.htm>.
Source[edit | edit source]
- BURES, J. , et al. Epidemiology of Helicobacter pylori infection in the Czech Republic. Helicobacter. 2006, vol. 11, no. 1, p. 56–65, ISSN 1523-5378 [online], 1083-4389 [print]. PMID: 16423091.
- BONAMICO, M. , et al. Evaluation of stool antigen test, PCR on ORAL samples and serology for the noninvasive detection of Helicobacter pylori infection in children. Helicobacter. 2004, vol. 9, no. 1, p. 69–76, ISSN 1083-4389 [print], 1523-5378 [online]. PMID: 15156906.
- SMITH, SI. , et al. Comparison of three PCR methods for detection of Helicobacter pylori DNA and detection of cagA gene in gastric biopsy specimens. World J Gastroenterol. 2004, vol. 10, no. 13, p. 1958–1960, ISSN 1007-9327. PMID: 15222045.
- NAKATA, H. , et al. Immunological rapid urease test using monoclonal antibody for Helicobacter pylori. Journal of Gastroenterology and Hepatology. 2004, y. 19, vol. 9, p. 970–974, ISSN 08159319. PMID: 15304111.
- HINO, B. , et al. Comparison of invasive and non-invasive tests diagnosis and monitoring of Helicobacter pylori infection in children. Journal of pediatric gastroenterology and nutrition. 2004, vol. 39, no. 5, p. 519–523, ISSN 0277-2116 [print], 1536-4801 [online]. PMID: 15572892.